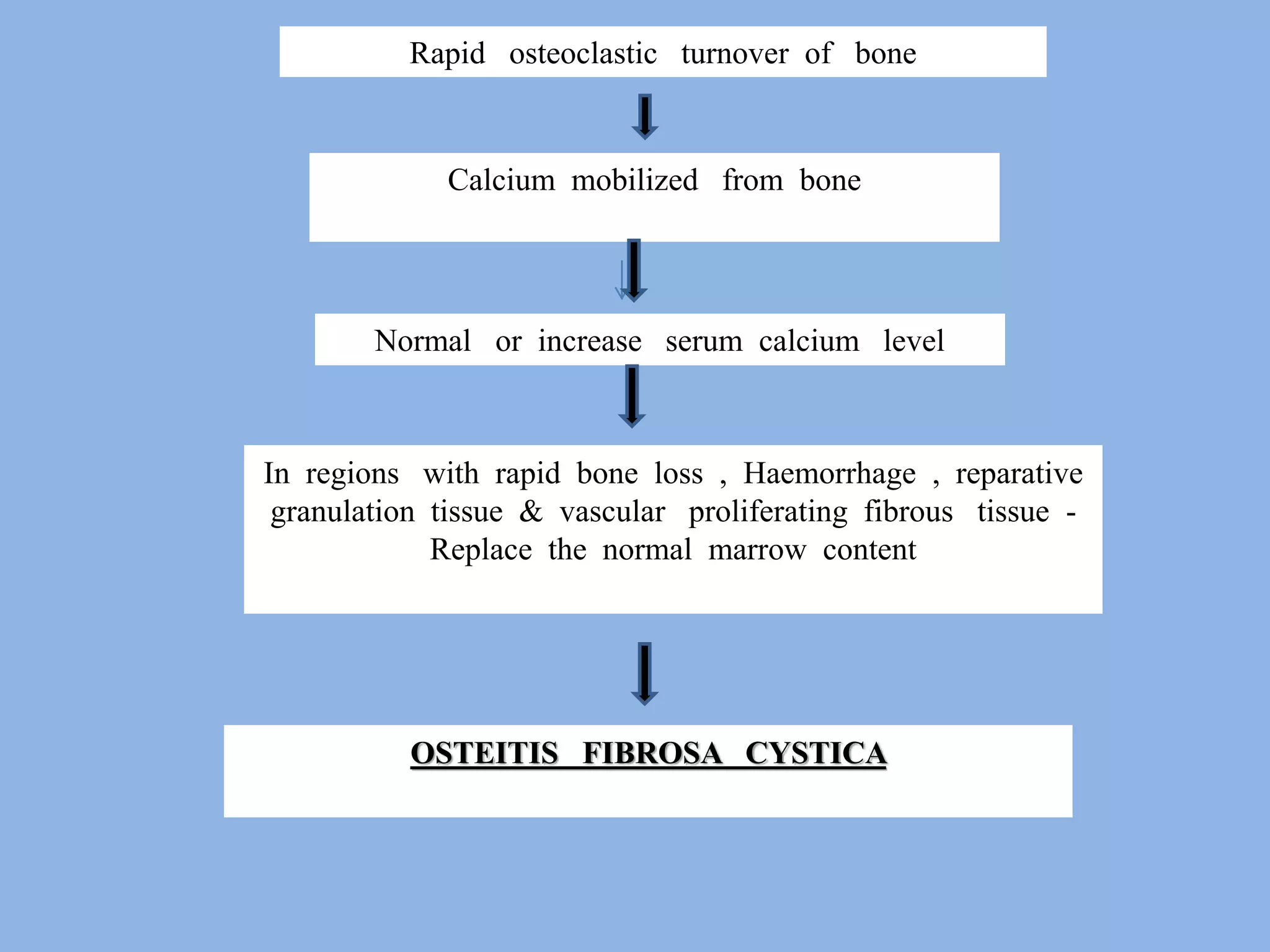
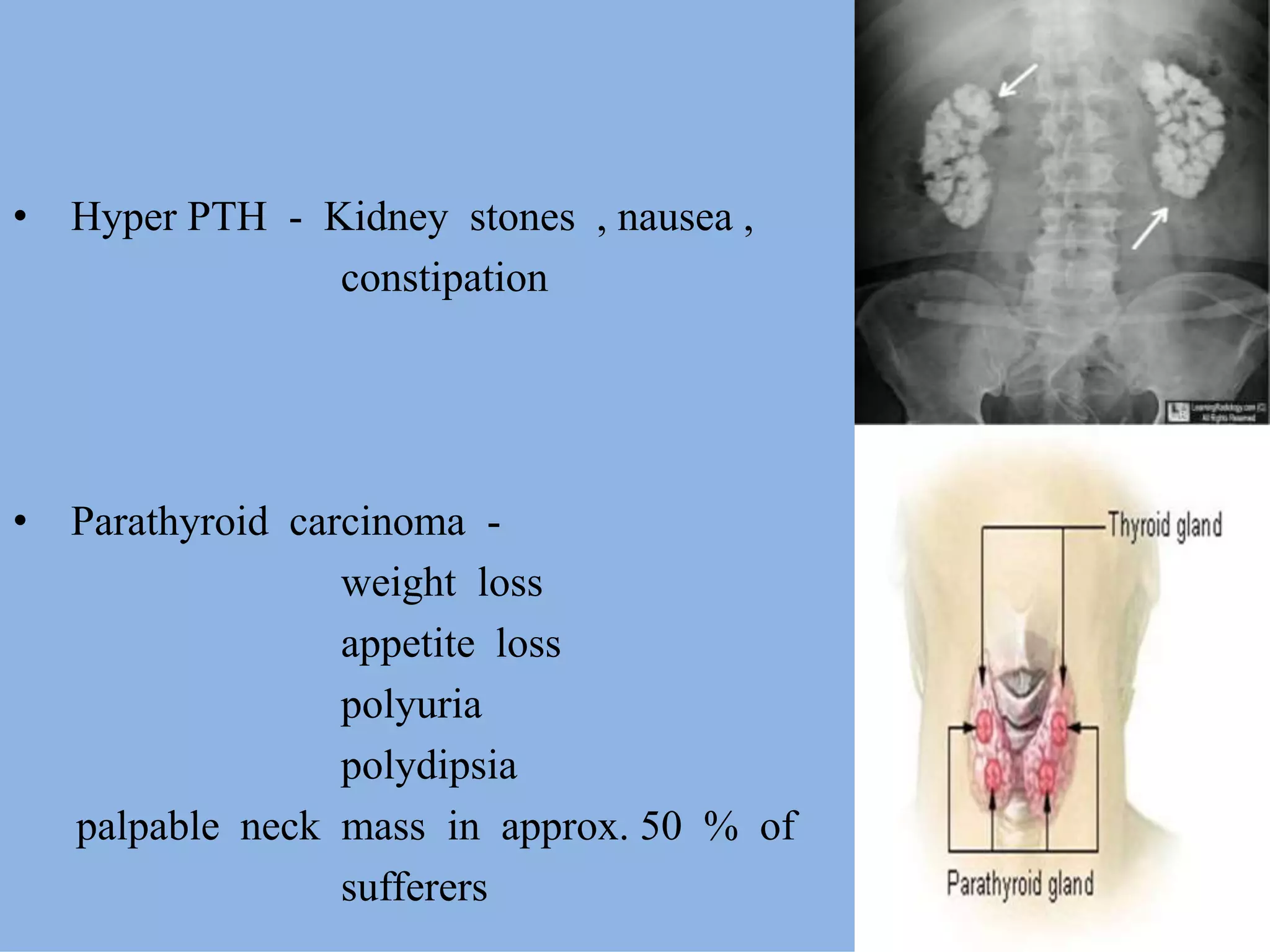
This document discusses osteitis fibrosa cystica (OFC), a rare bone disease caused by hyperparathyroidism. It defines OFC as a loss of bone mass replaced by fibrous tissue. Clinical features include bone pain, fractures, and brown tumors. Diagnosis involves lab tests showing high calcium and PTH levels. Treatment is typically parathyroidectomy to remove the overactive parathyroid gland(s), which can reverse bone changes. Prognosis is good if caught early and treated with surgery.