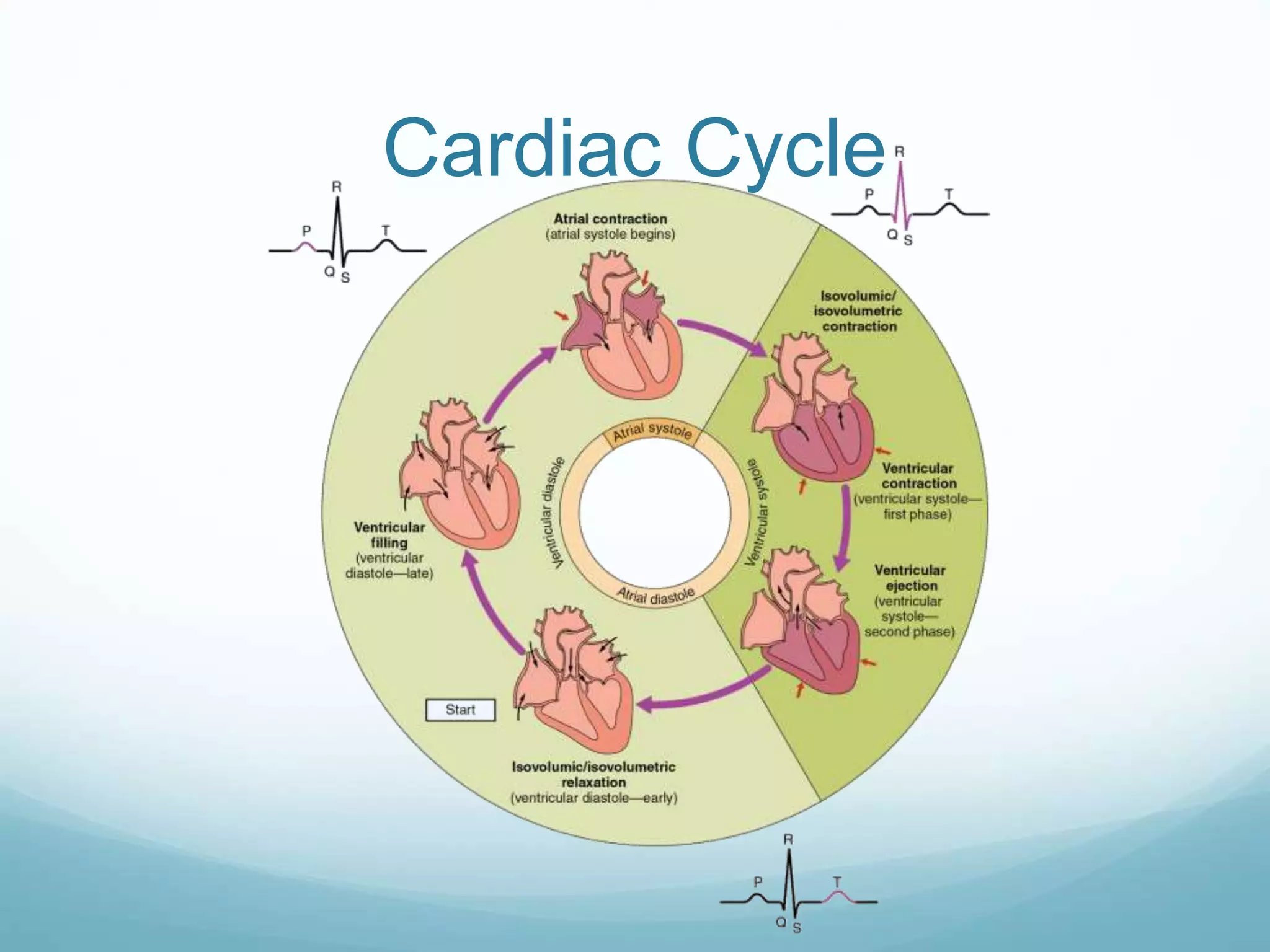
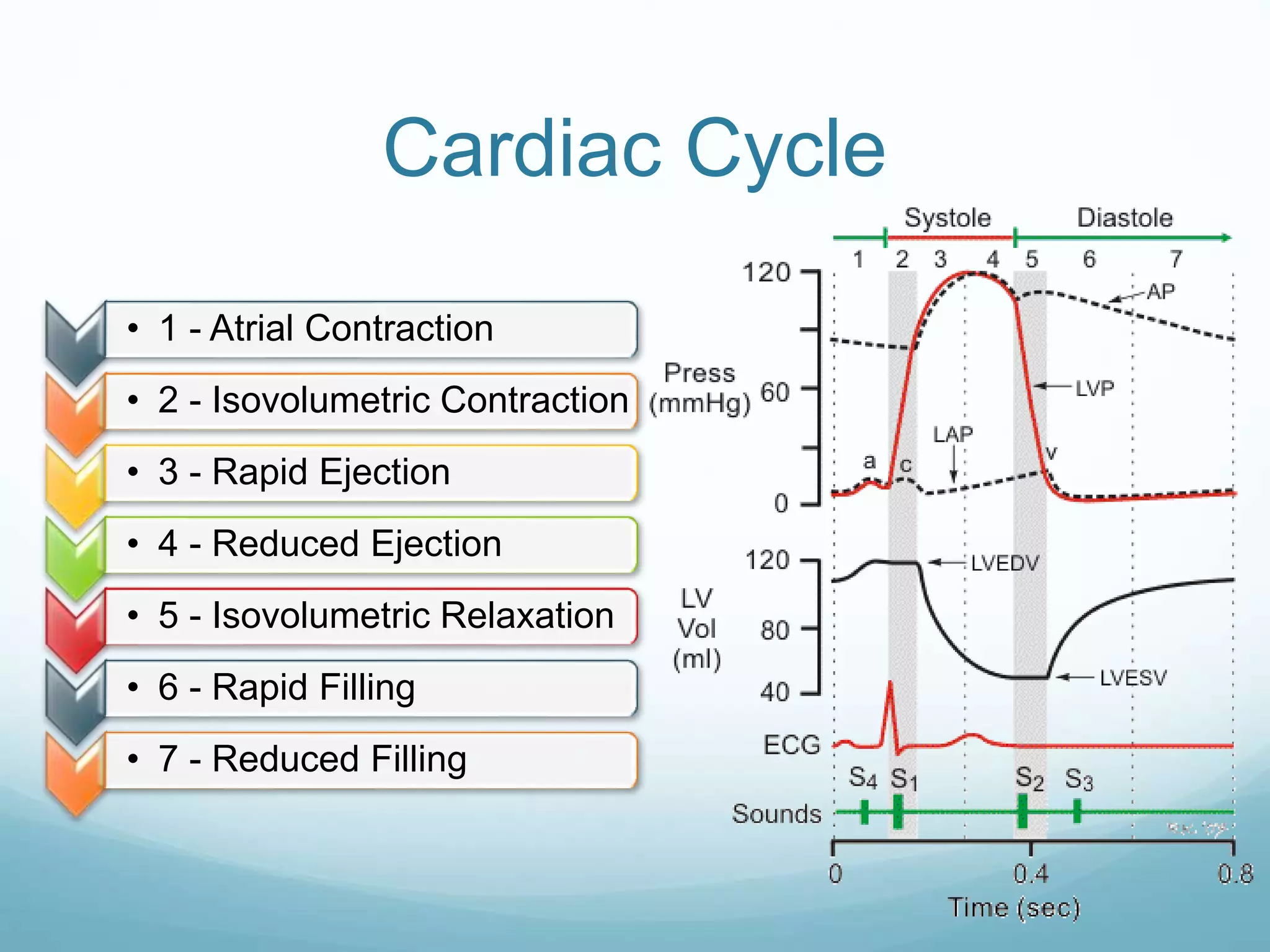
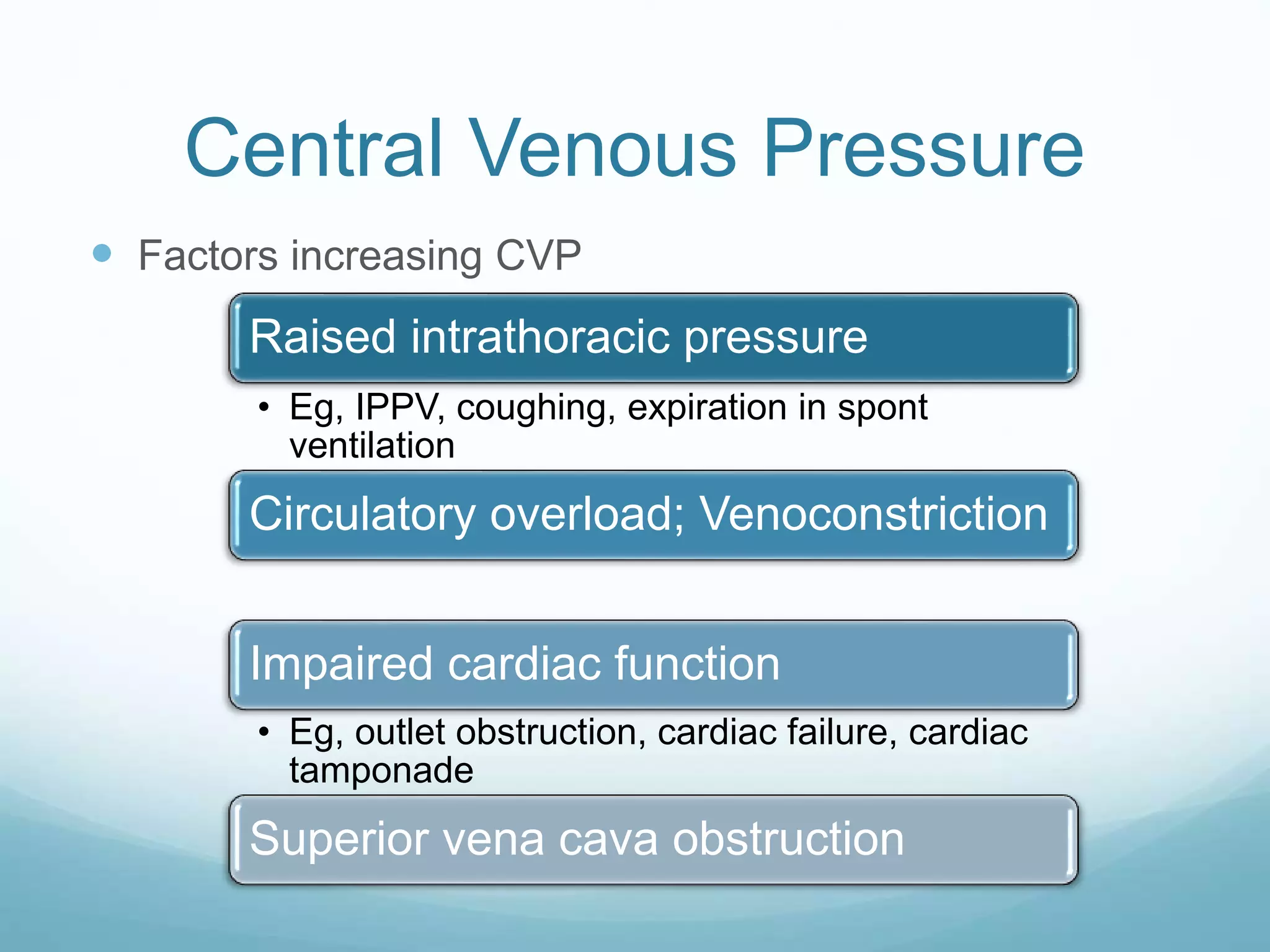
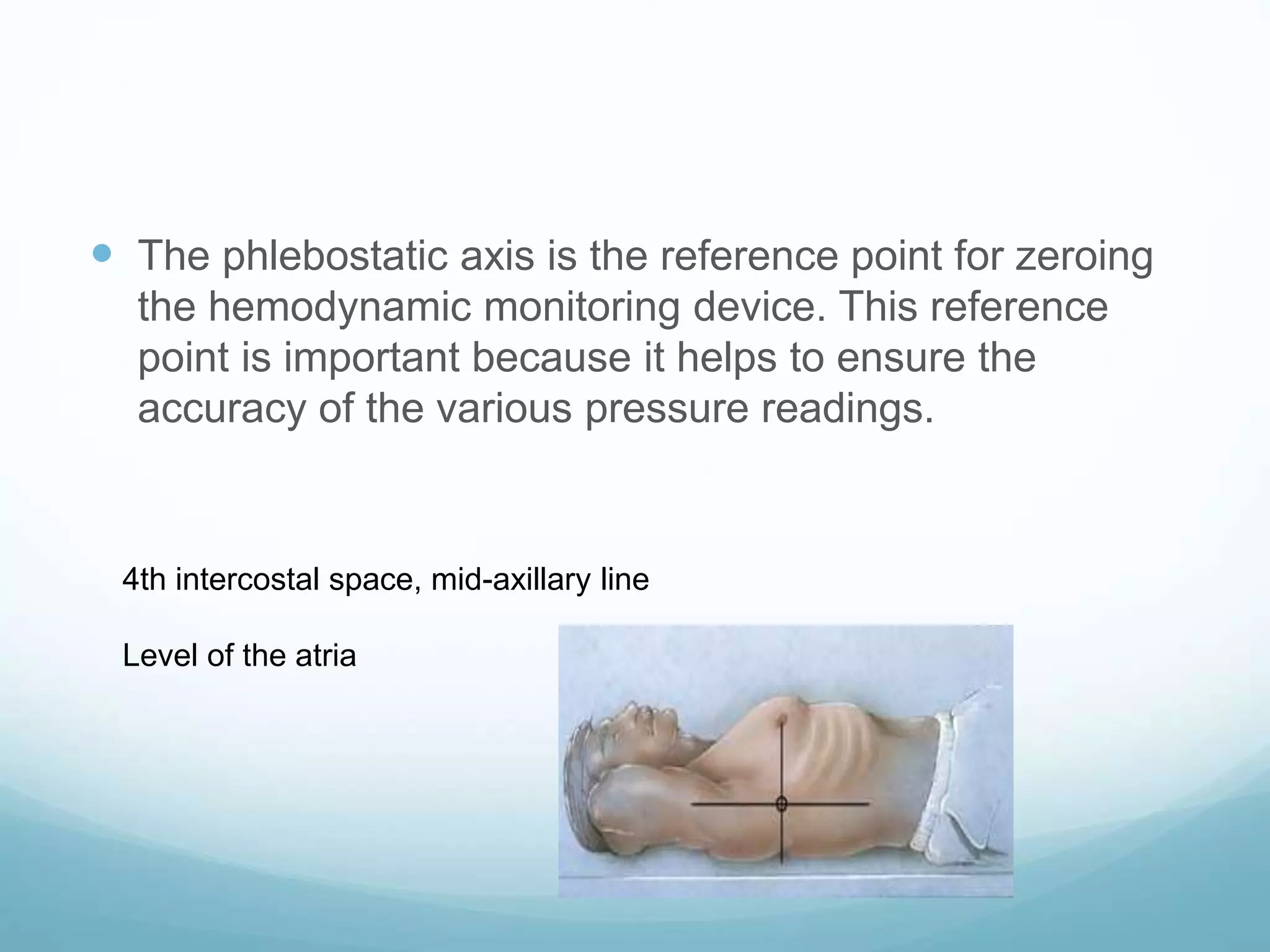
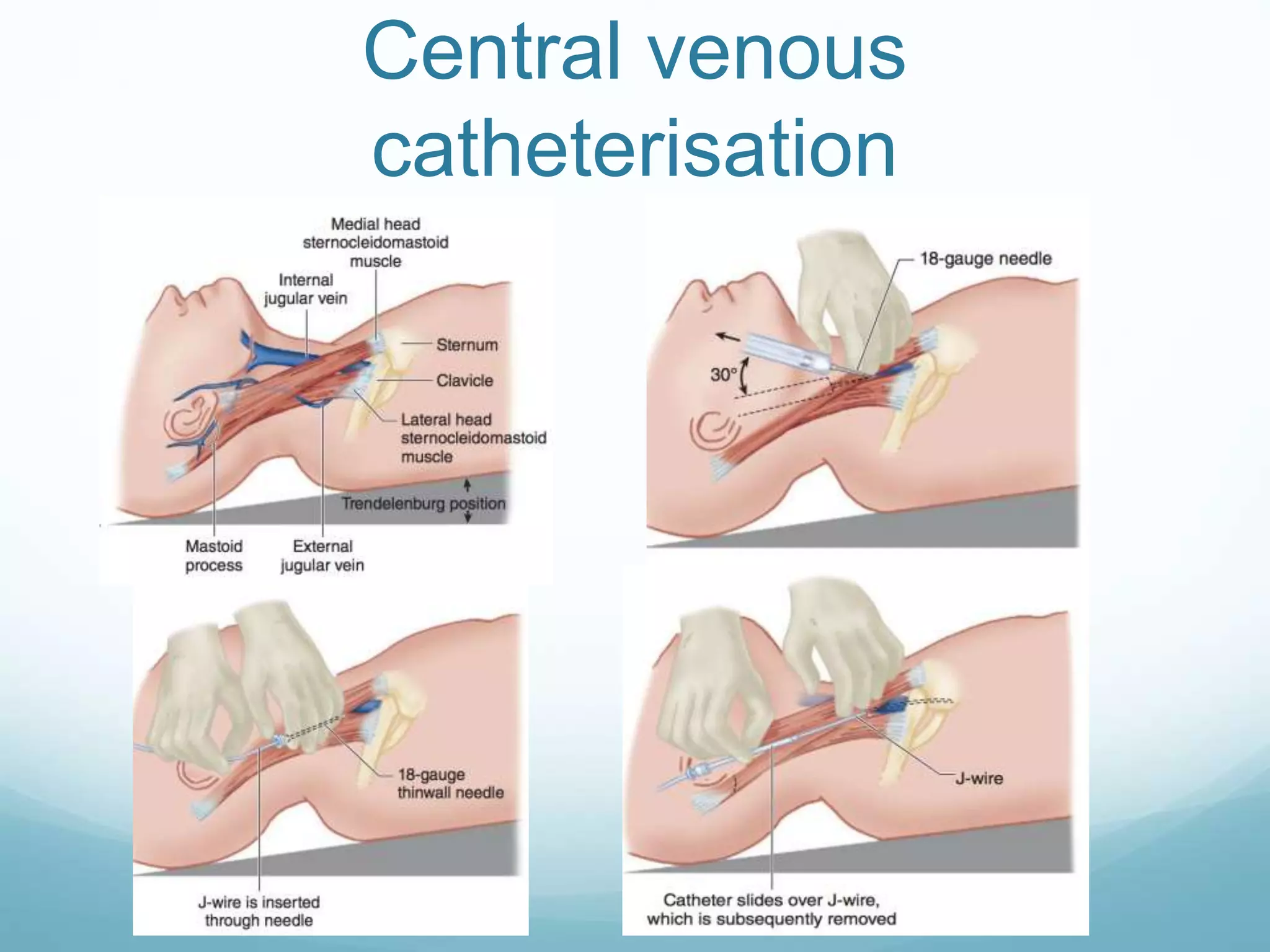
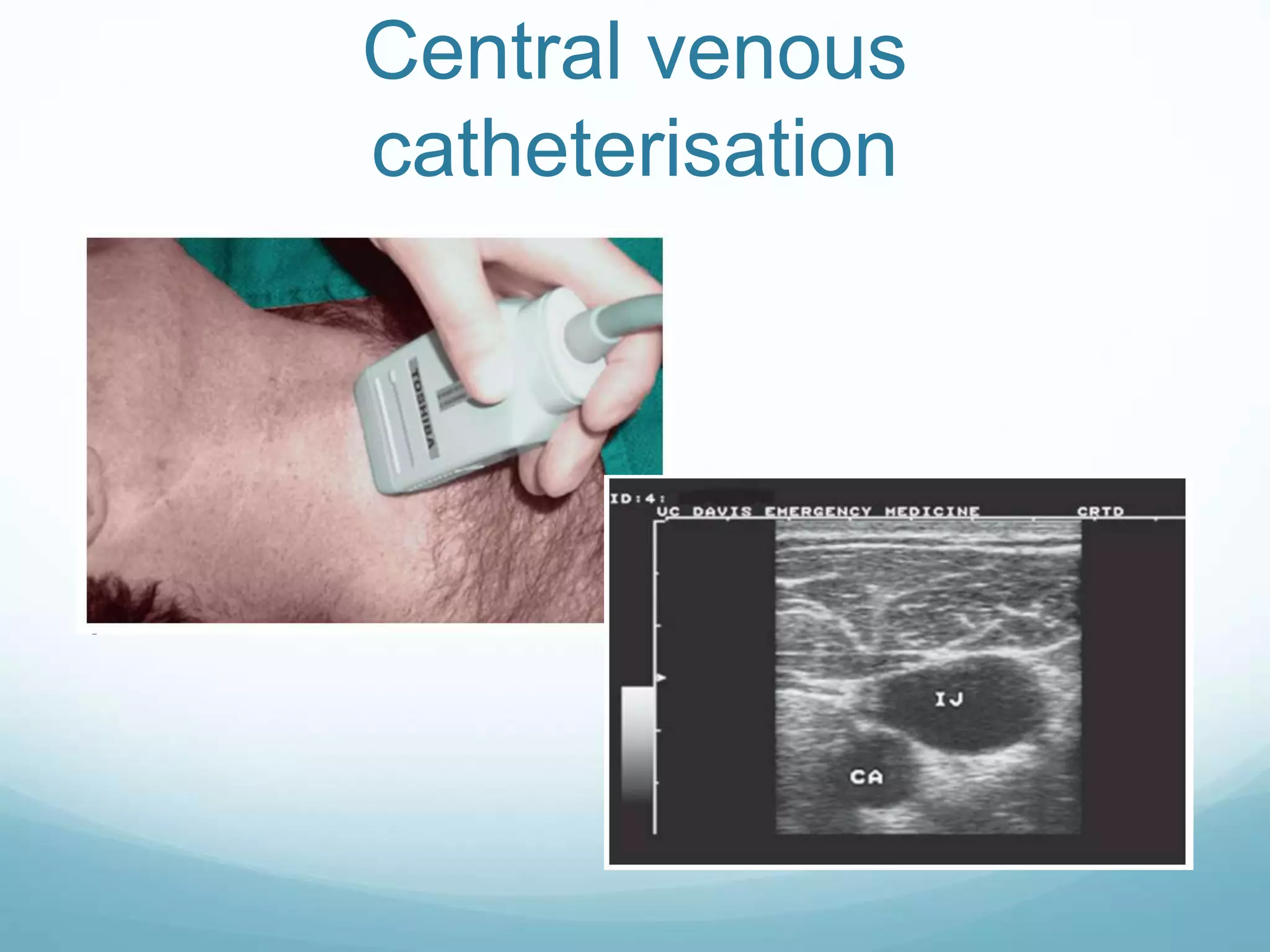
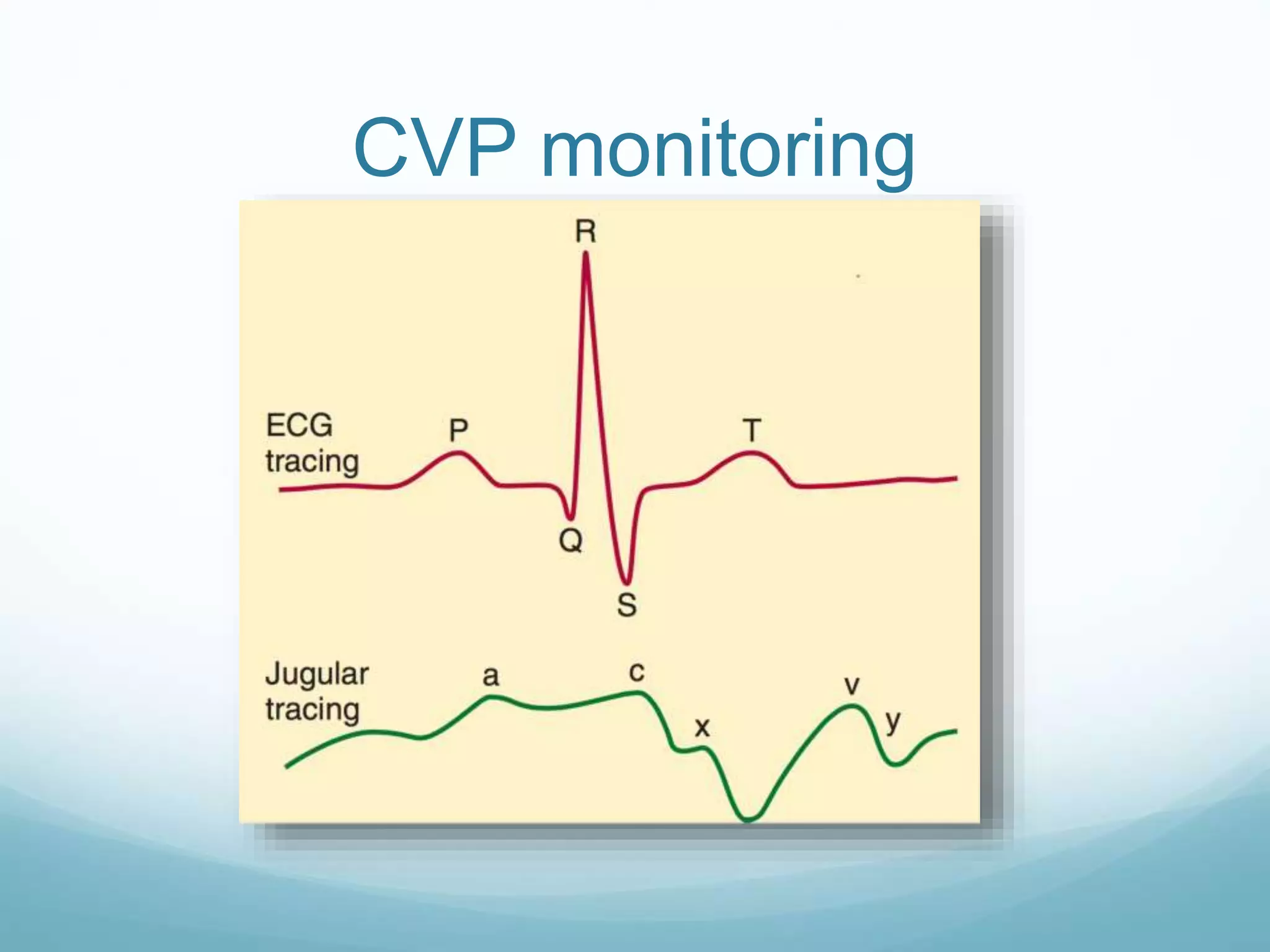
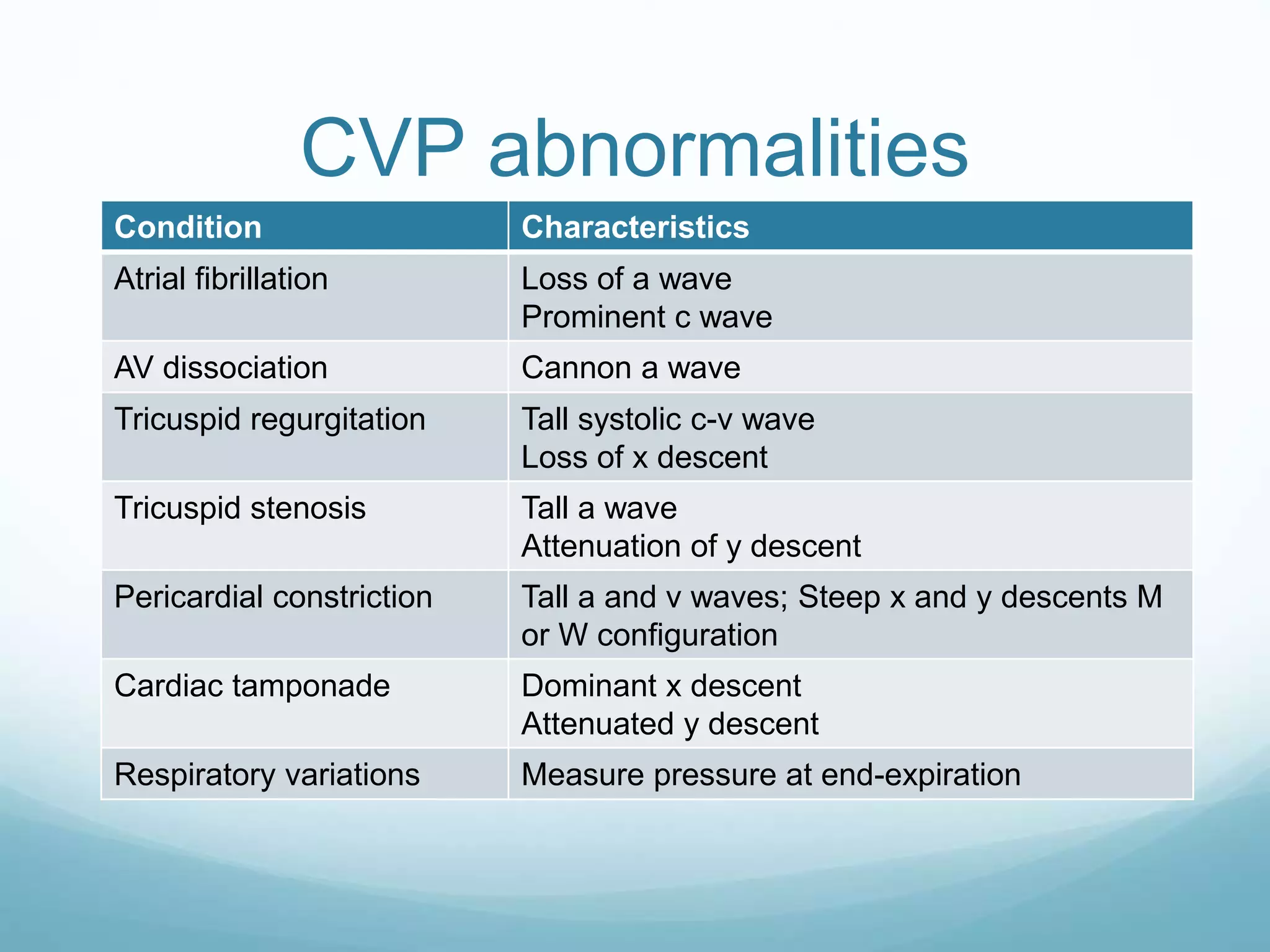
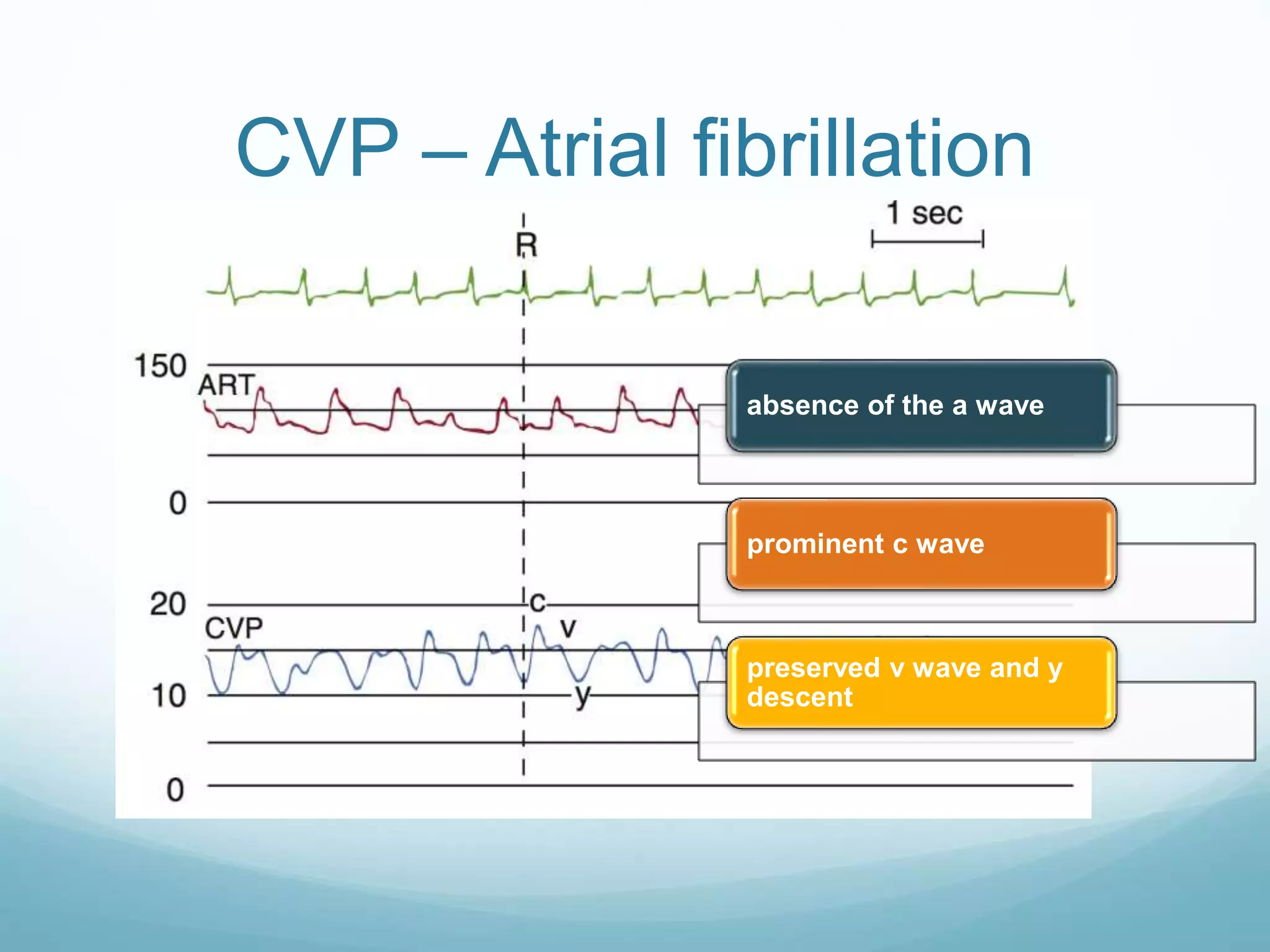
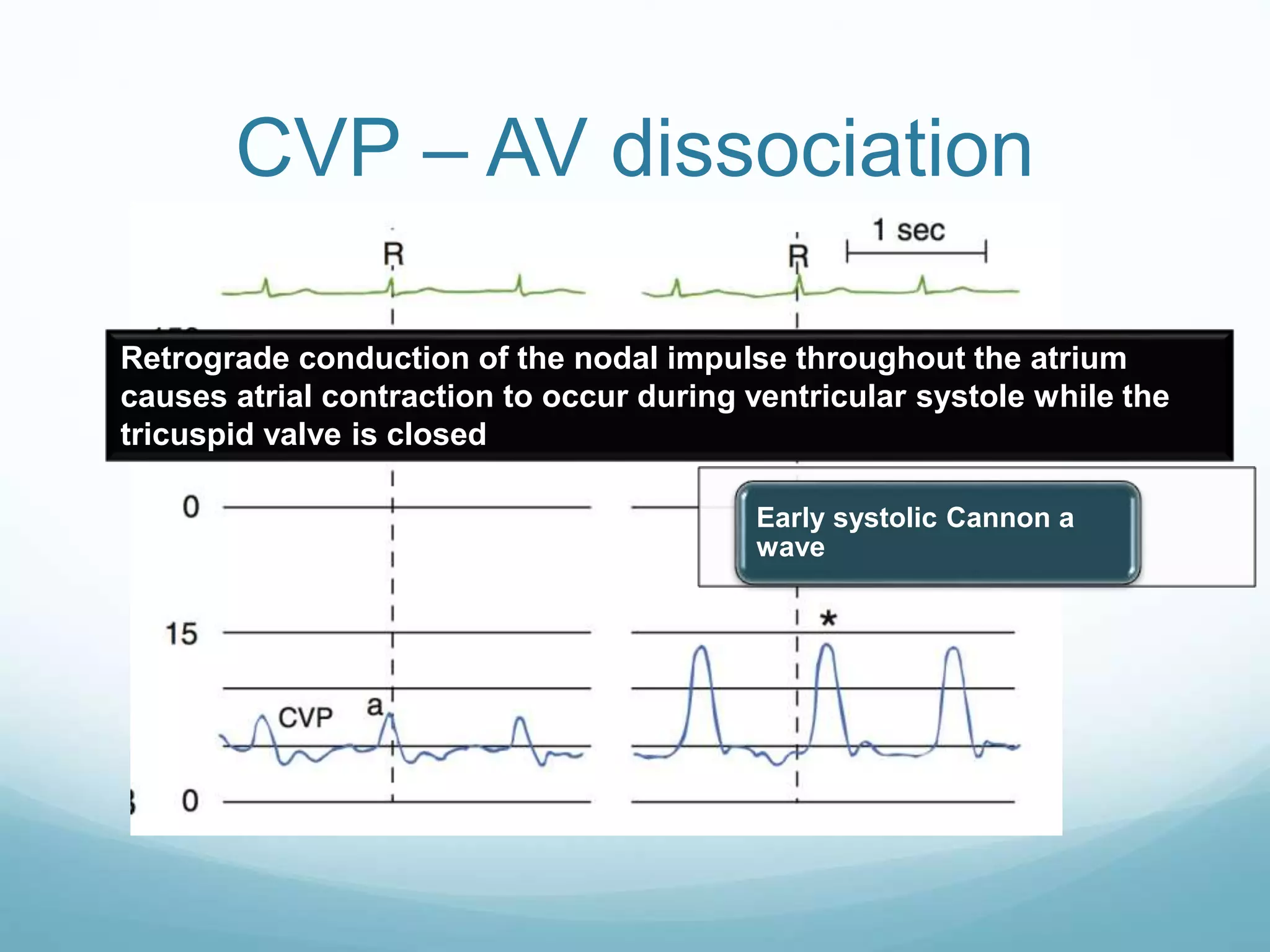
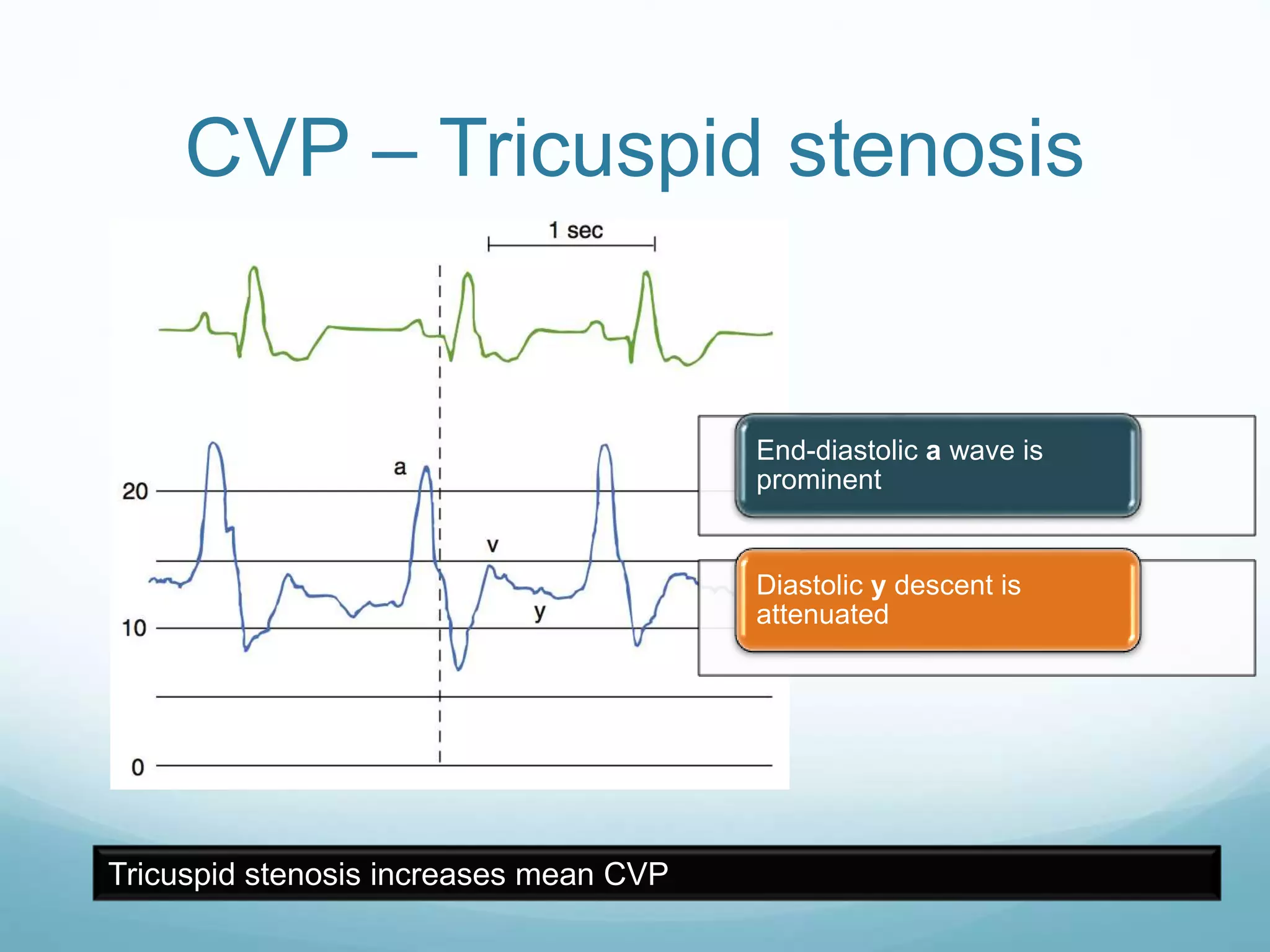
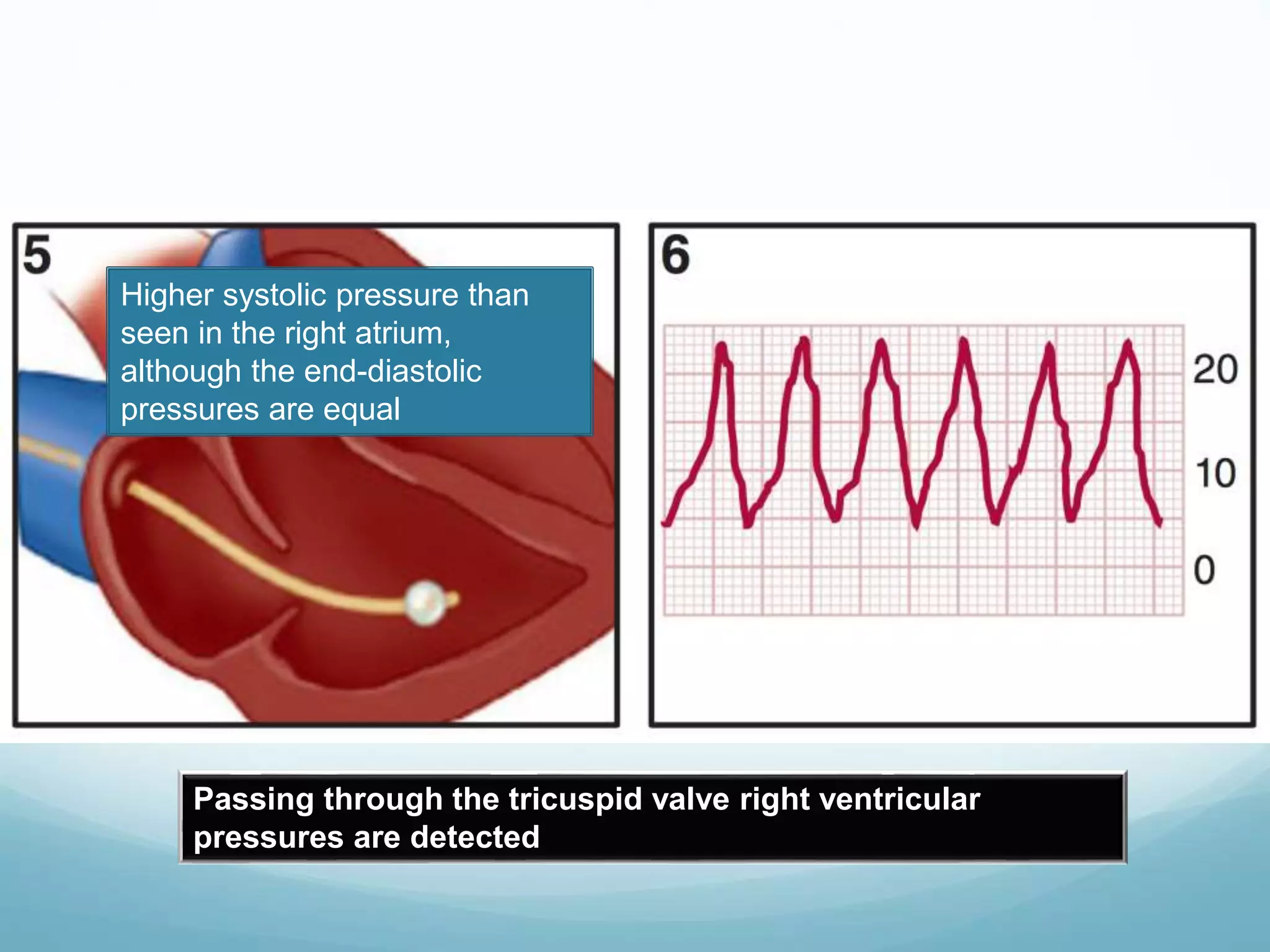
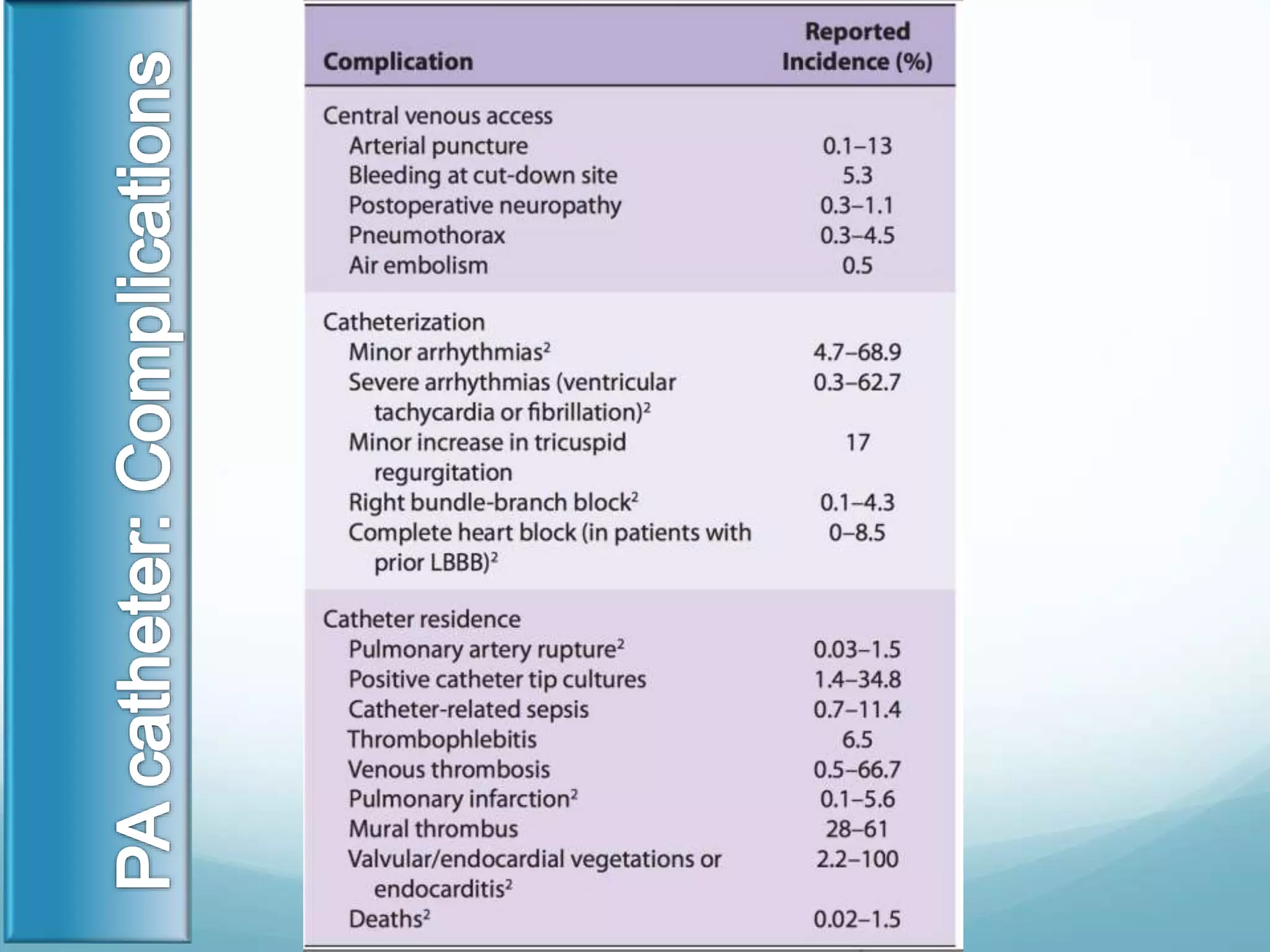
This document discusses CVP and PCWP monitoring. It begins by outlining the cardiac cycle and then defines CVP as the pressure in the thoracic vena cava near the right atrium. Factors that can increase or decrease CVP are described. CVP monitoring involves inserting a catheter into a vein to measure pressure in the right atrium. The document then discusses PCWP monitoring, which involves advancing a catheter into the pulmonary artery to measure pressure. Normal ranges for various hemodynamic parameters are provided. Contraindications for PA catheter use are also outlined.