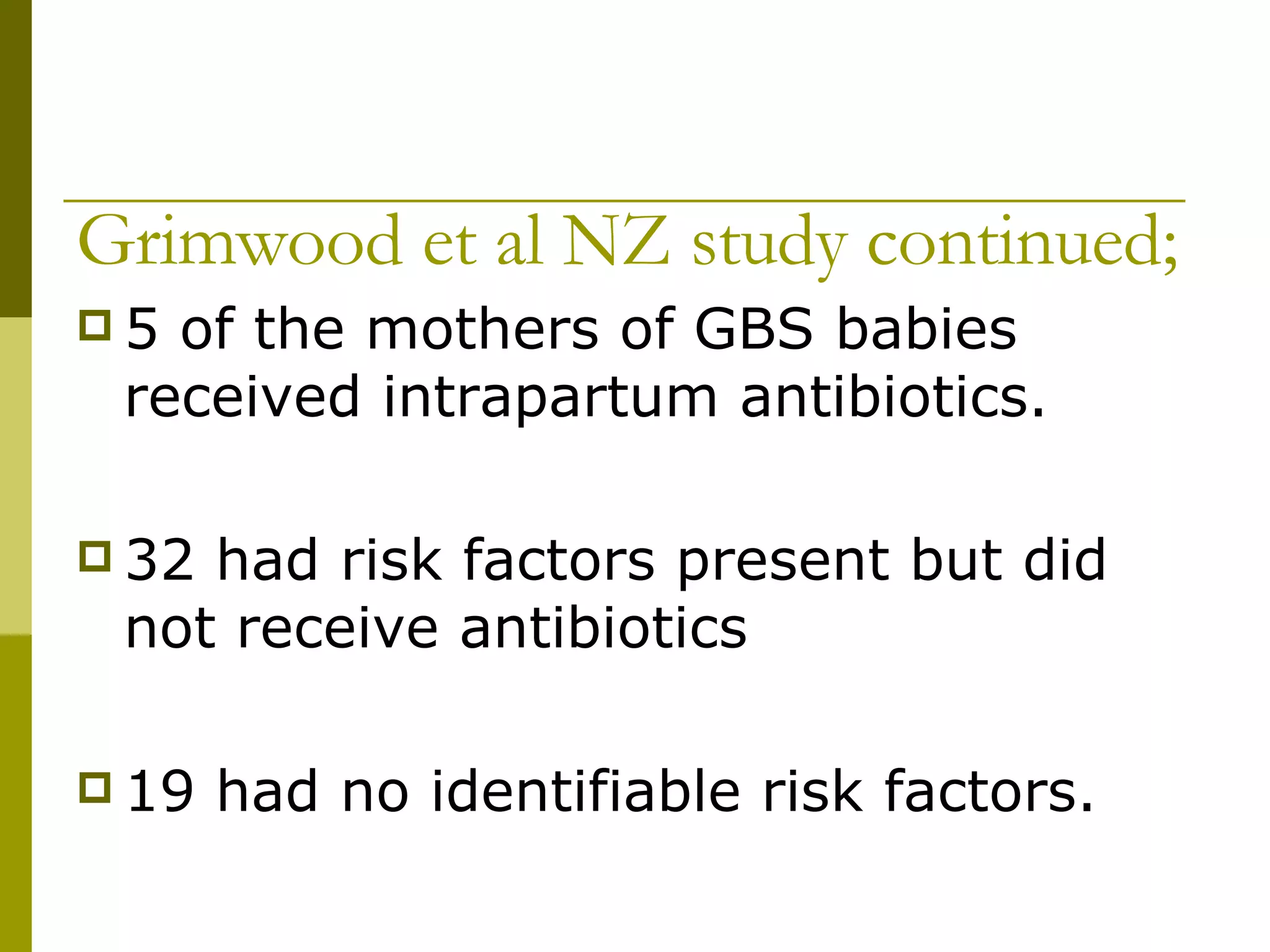
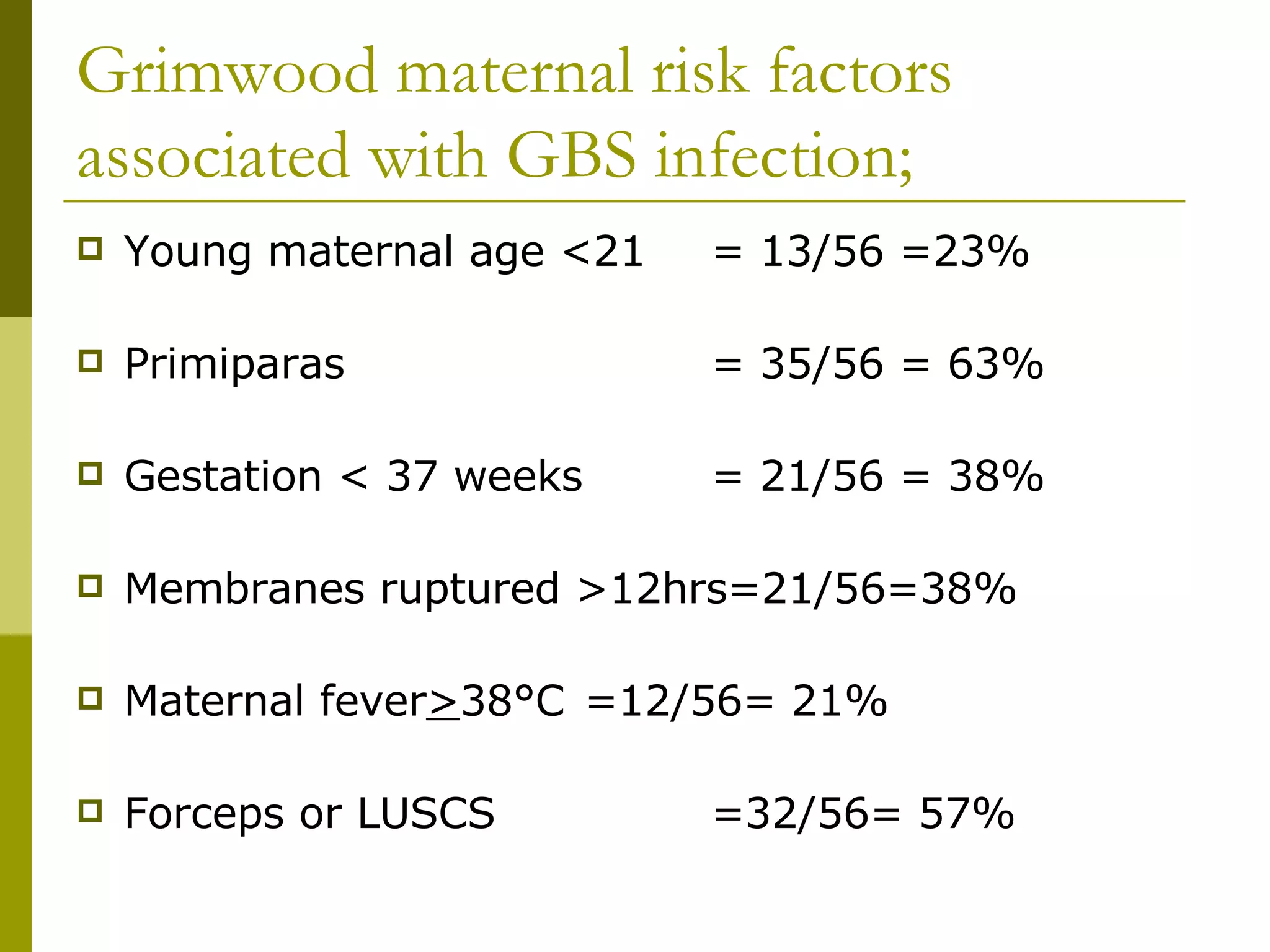
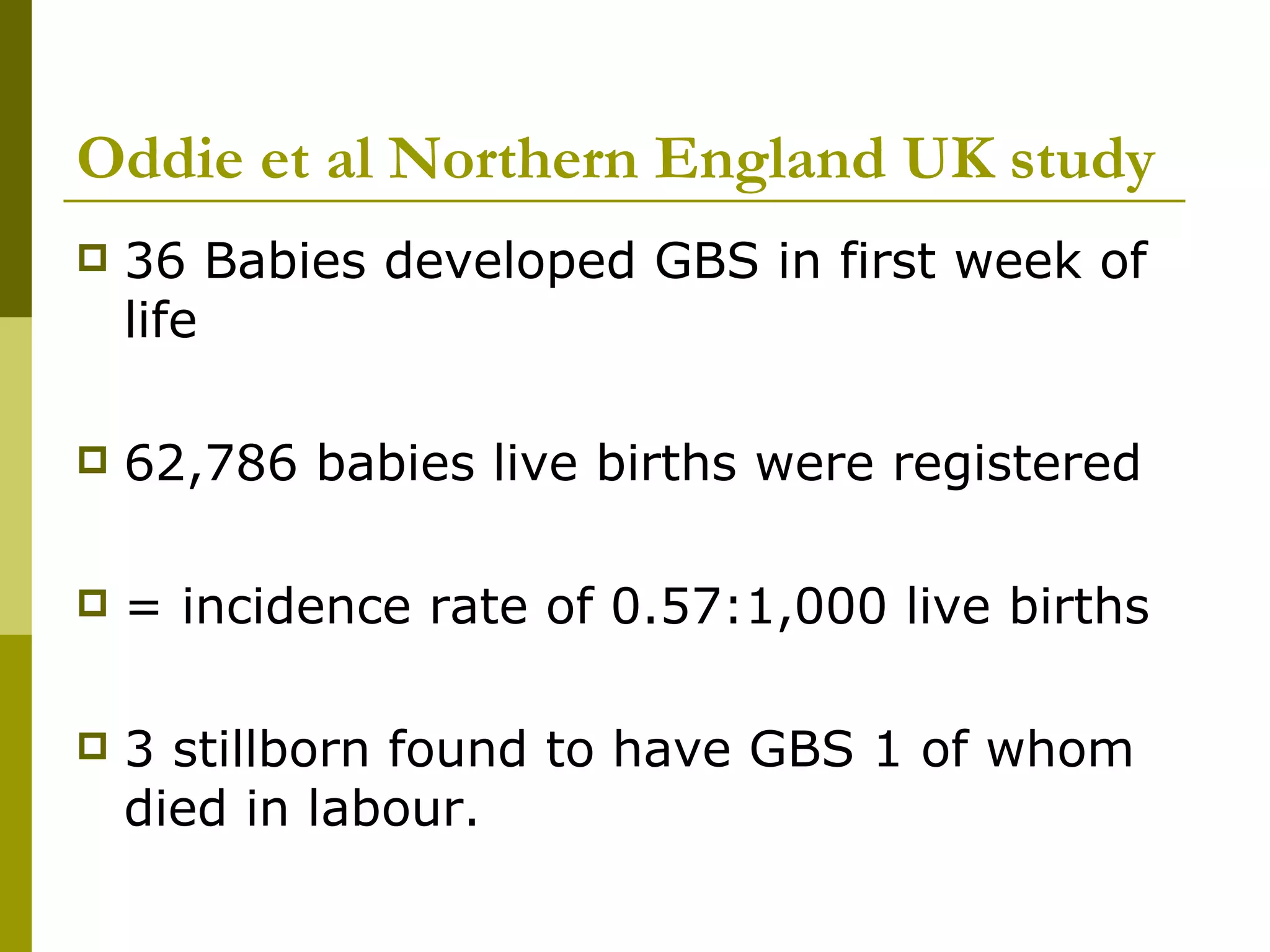
Group B Streptococcus (GBS) is a bacteria that can cause neonatal infections. Studies show the rate of early onset GBS in newborns has declined with the introduction of antibiotic prophylaxis during labor for women with risk factors. Risk factors include premature rupture of membranes, fever, previous GBS-infected baby. Guidelines recommend antibiotics for women in labor with risk factors to prevent transmission of GBS to the newborn around birth.