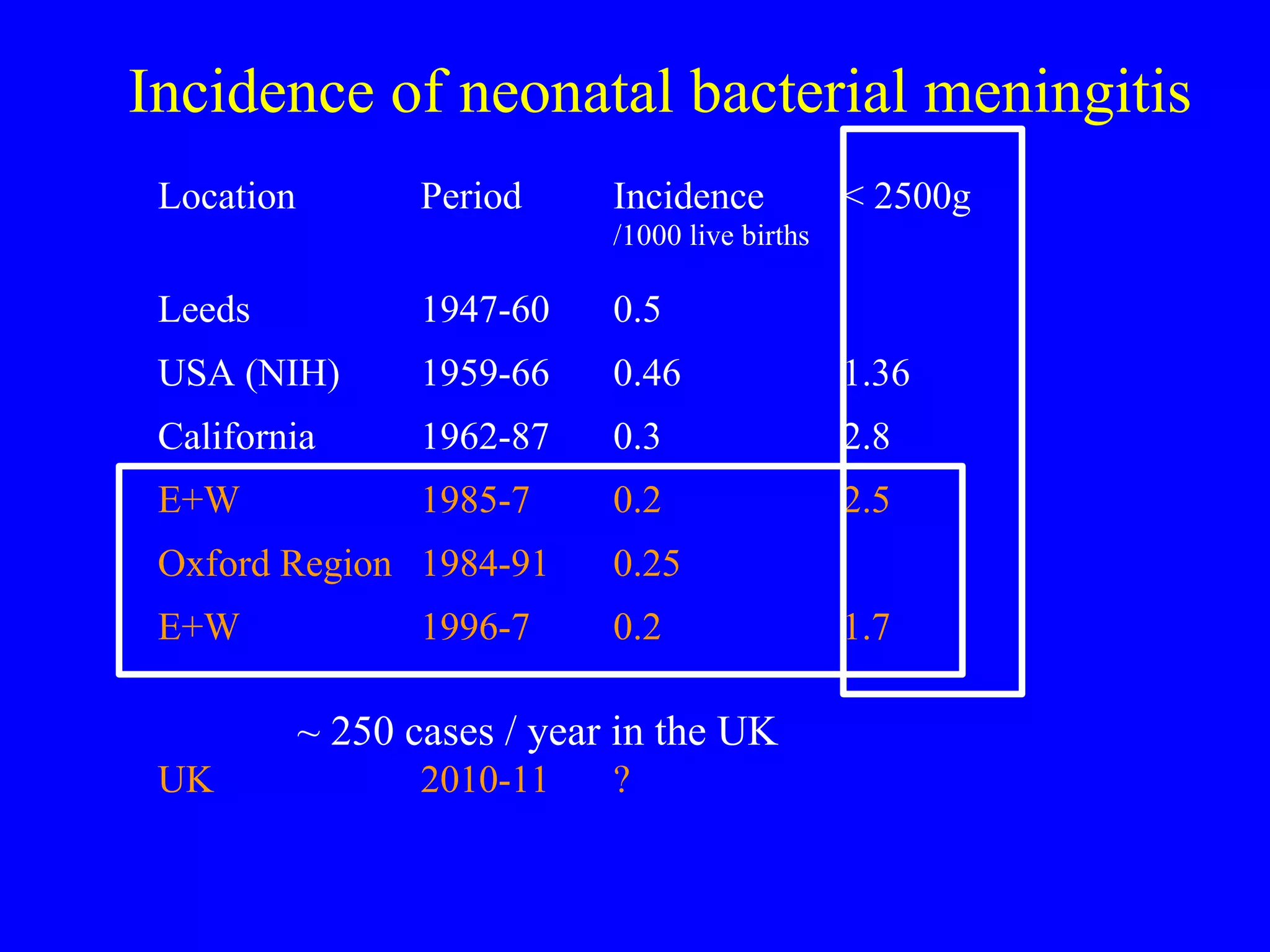
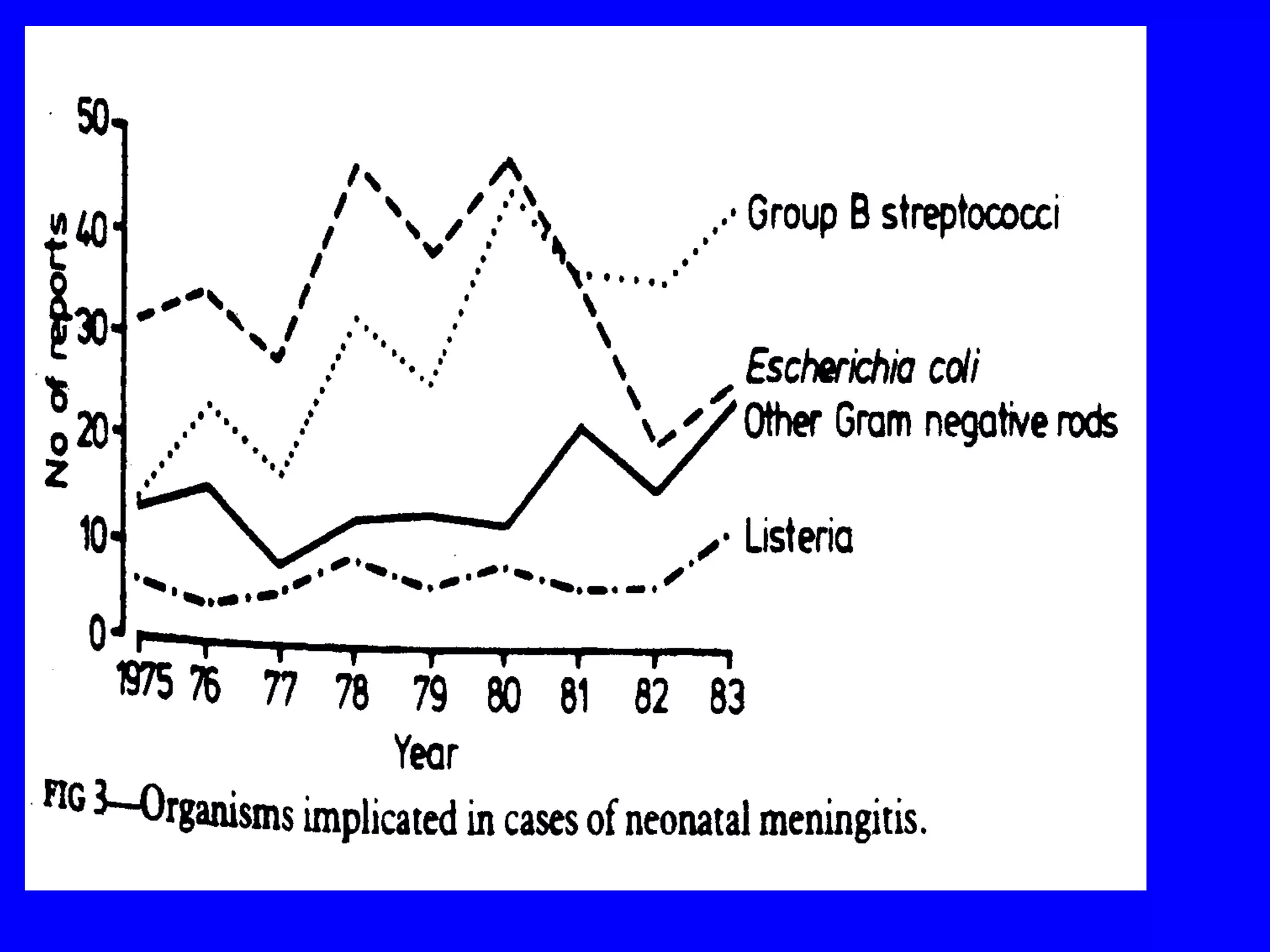
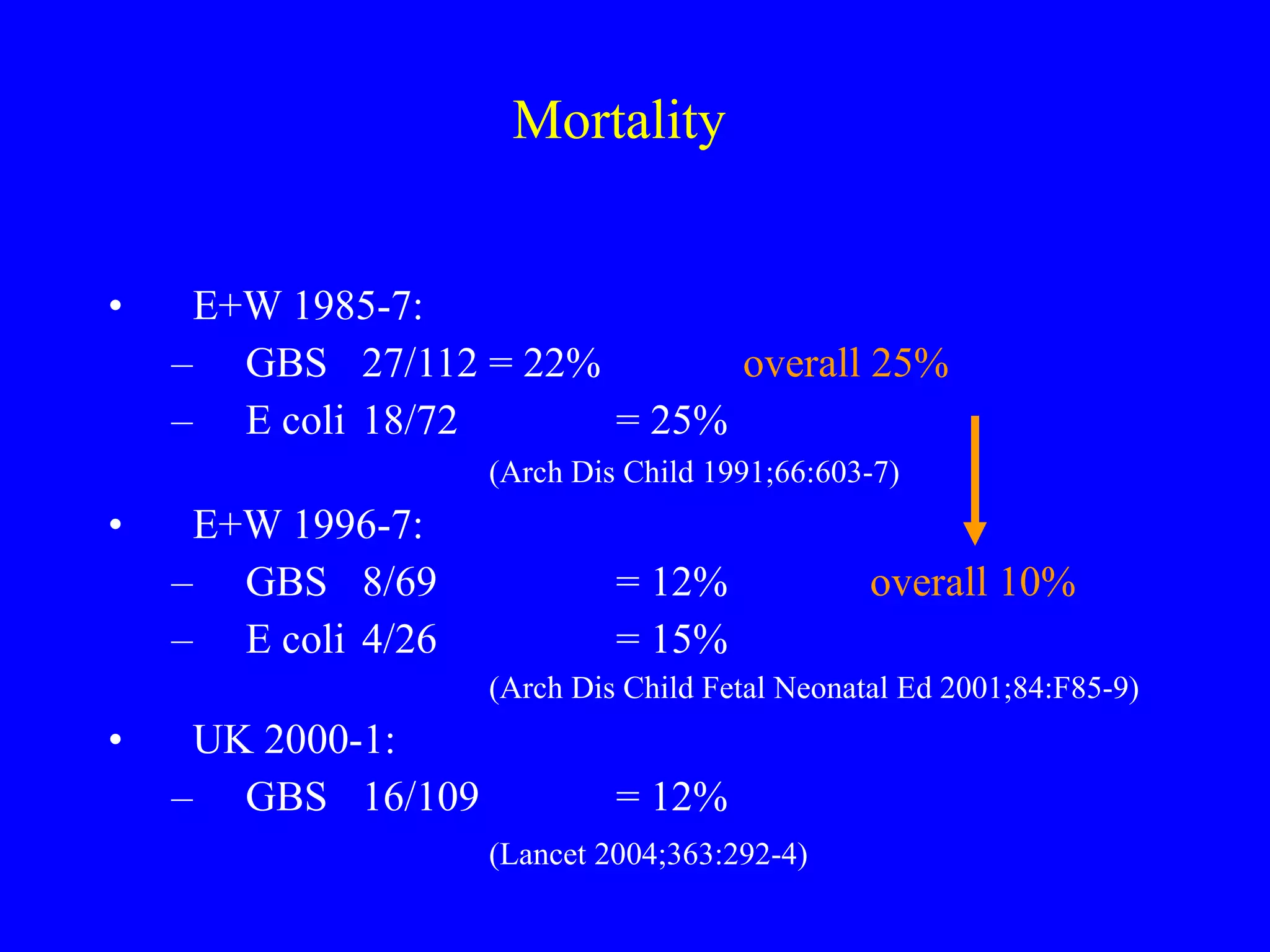
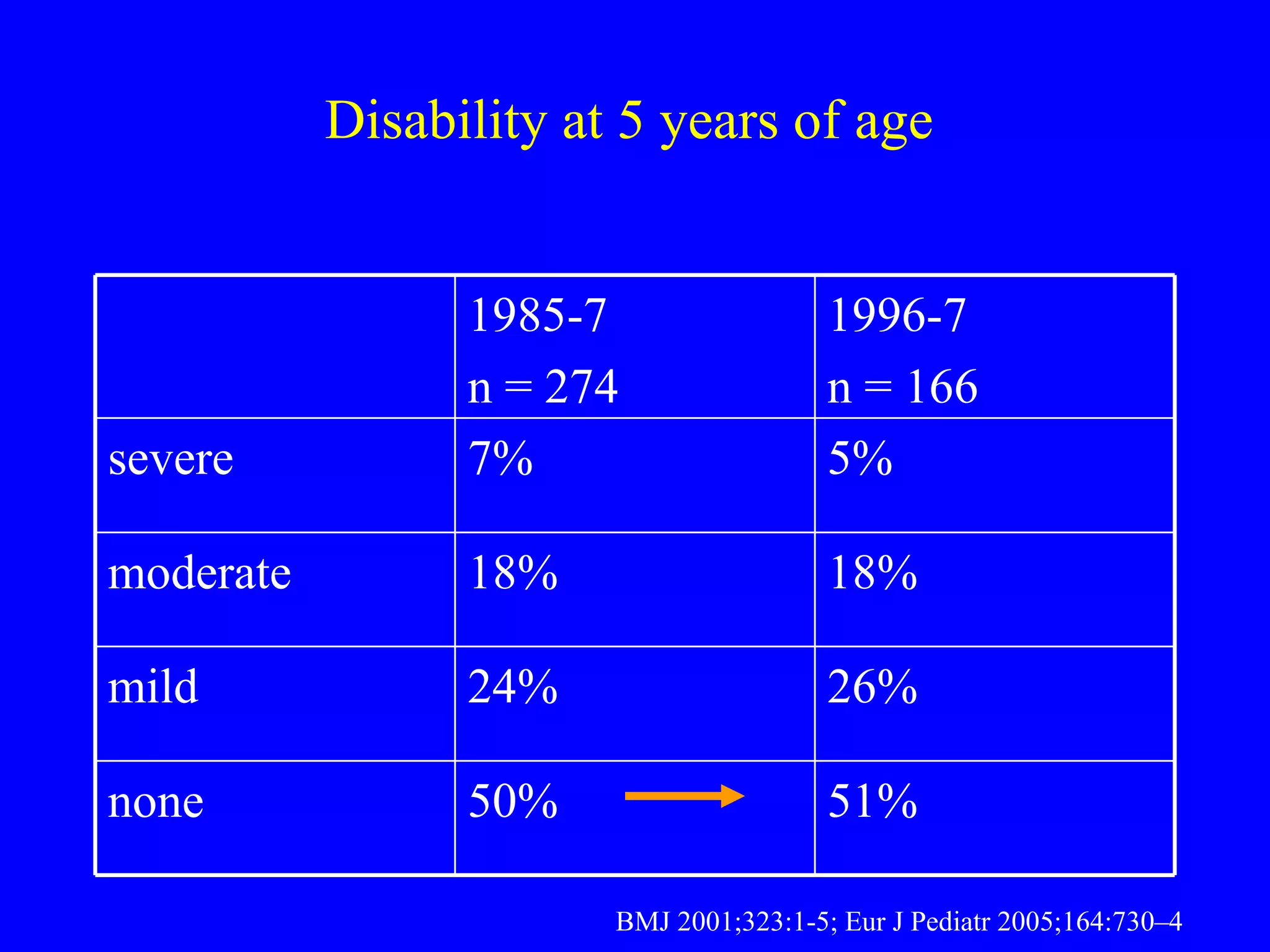
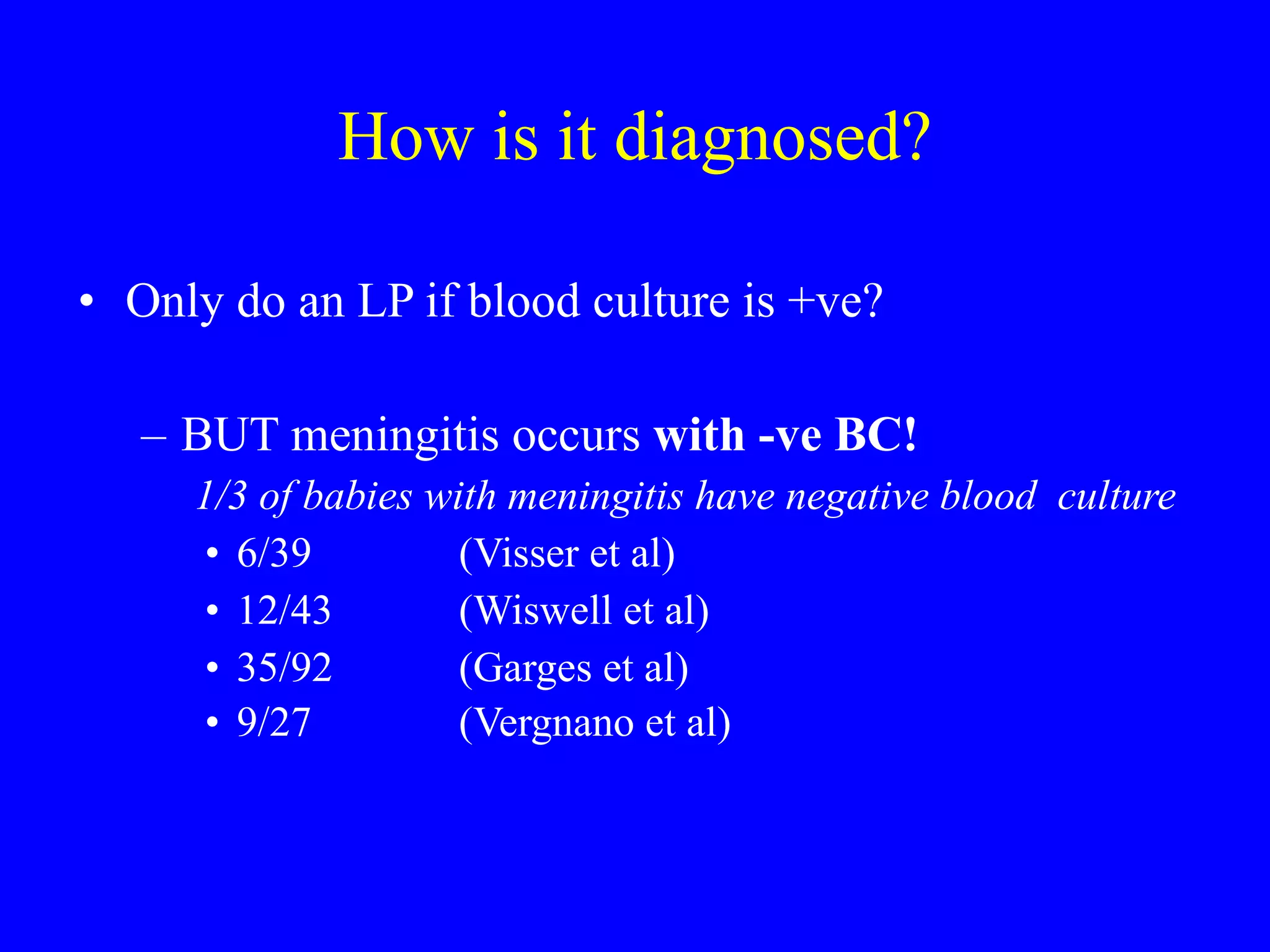
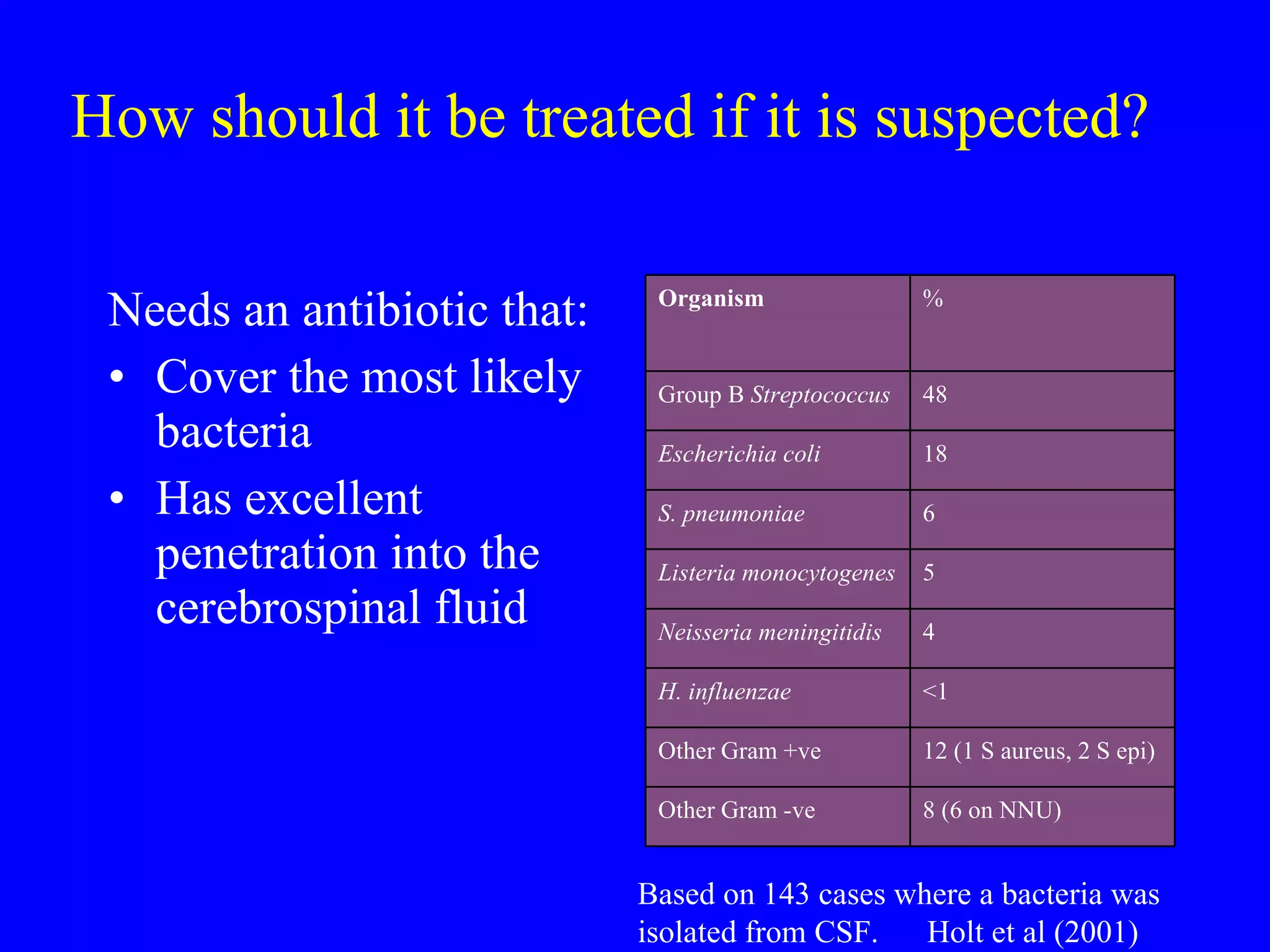
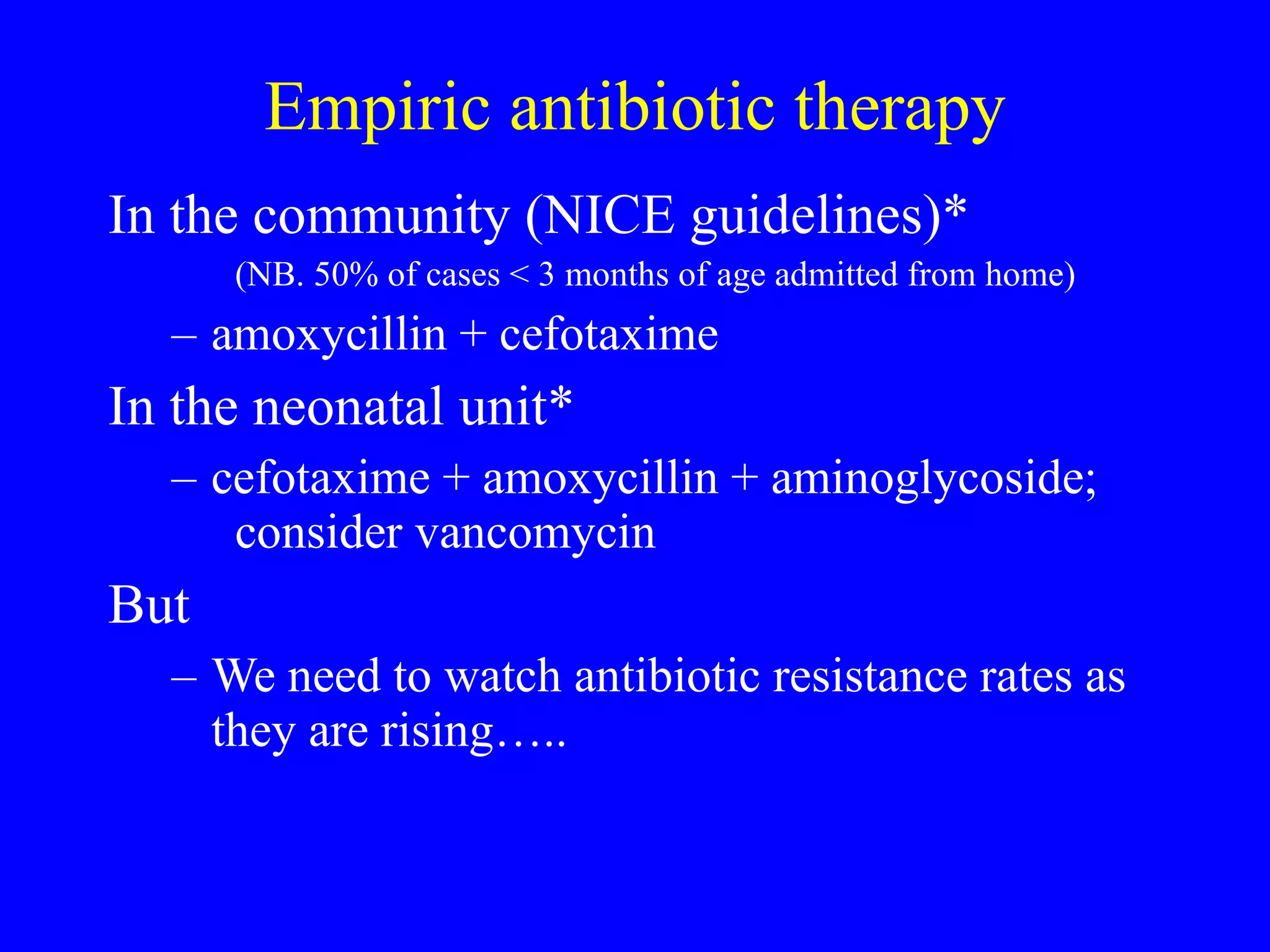
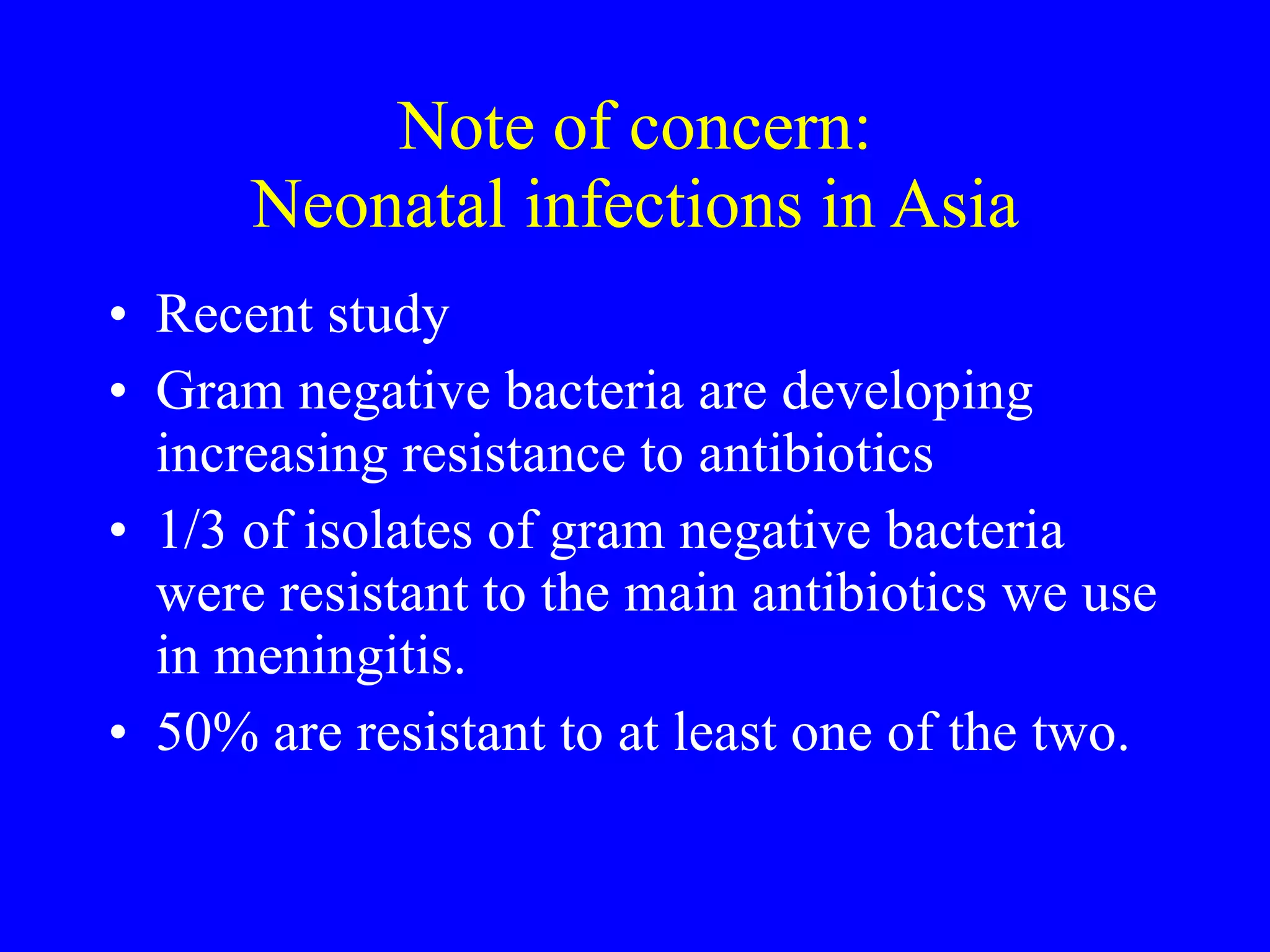
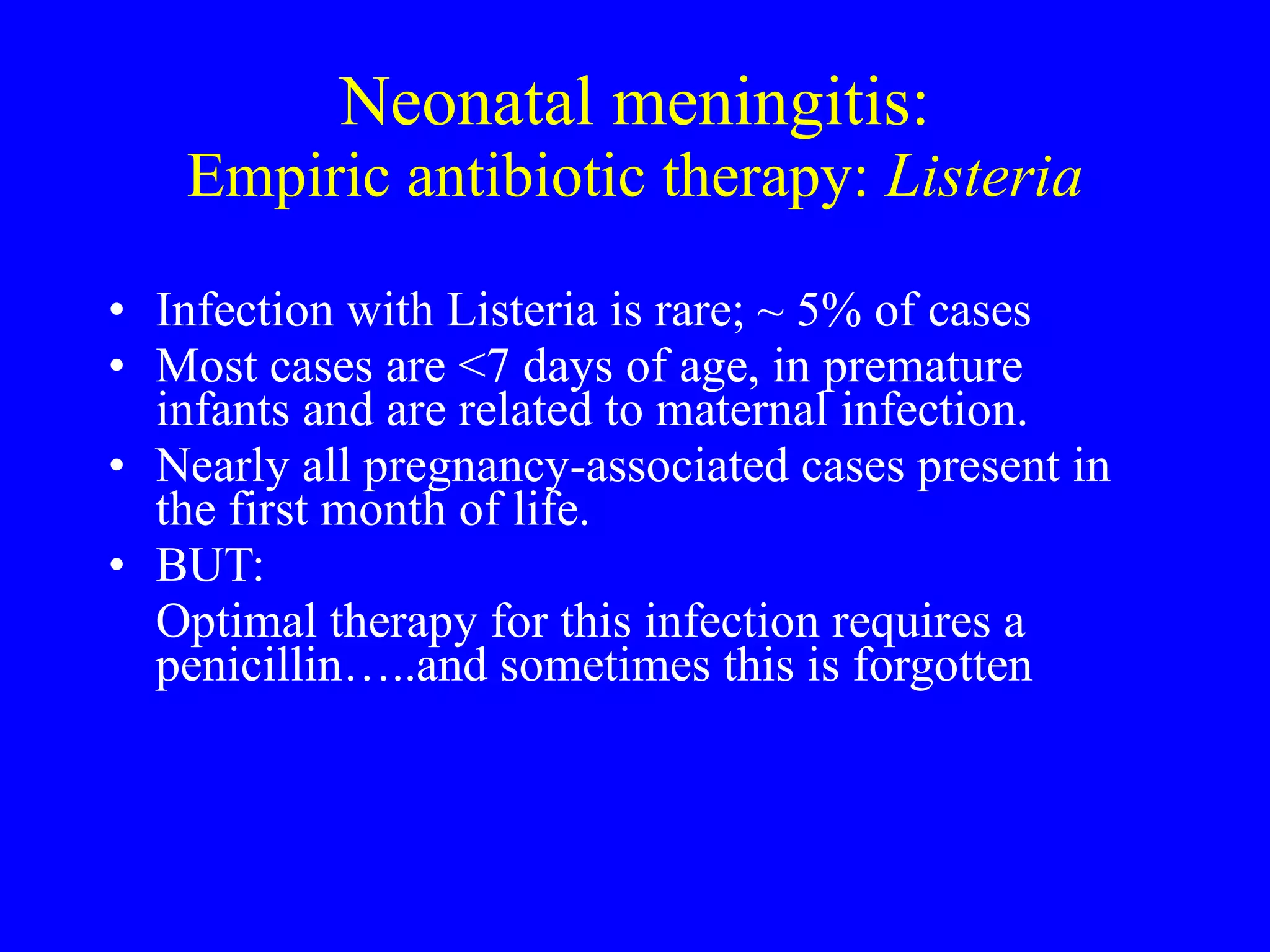
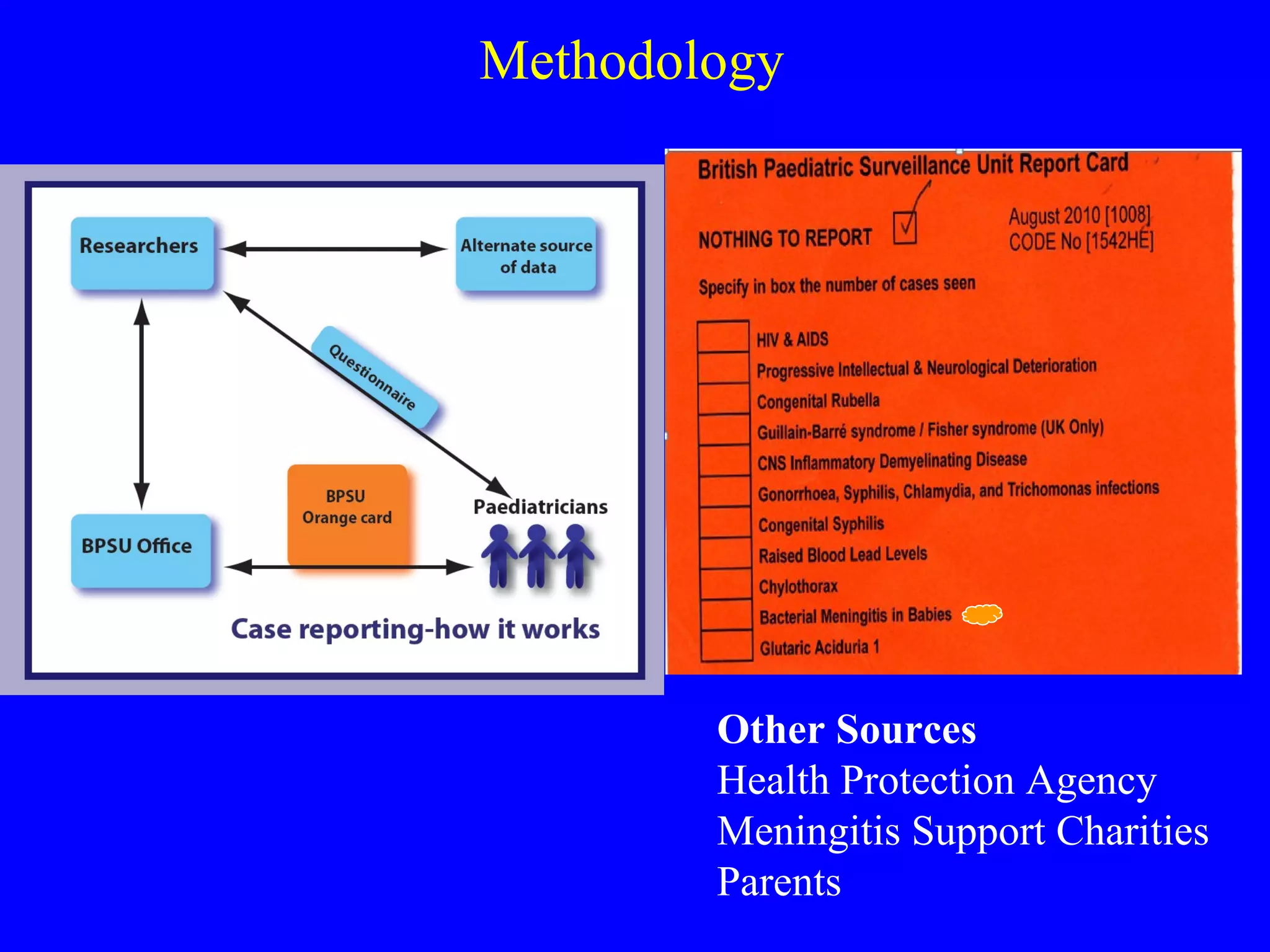
Bacterial meningitis in infants under 90 days old remains a significant burden in the UK and Ireland, with approximately 250 cases reported annually. While mortality has decreased over time to around 12%, long-term neurological complications and disabilities persist in around 20-25% of survivors. Effective diagnosis relies on lumbar puncture since clinical signs are non-specific, but many infants do not receive timely lumbar punctures. There is a lack of evidence regarding optimal antibiotic treatment duration and adjunctive therapies. Two ongoing studies aim to better define the current disease burden and identify opportunities to improve outcomes through earlier recognition, management, and prevention.