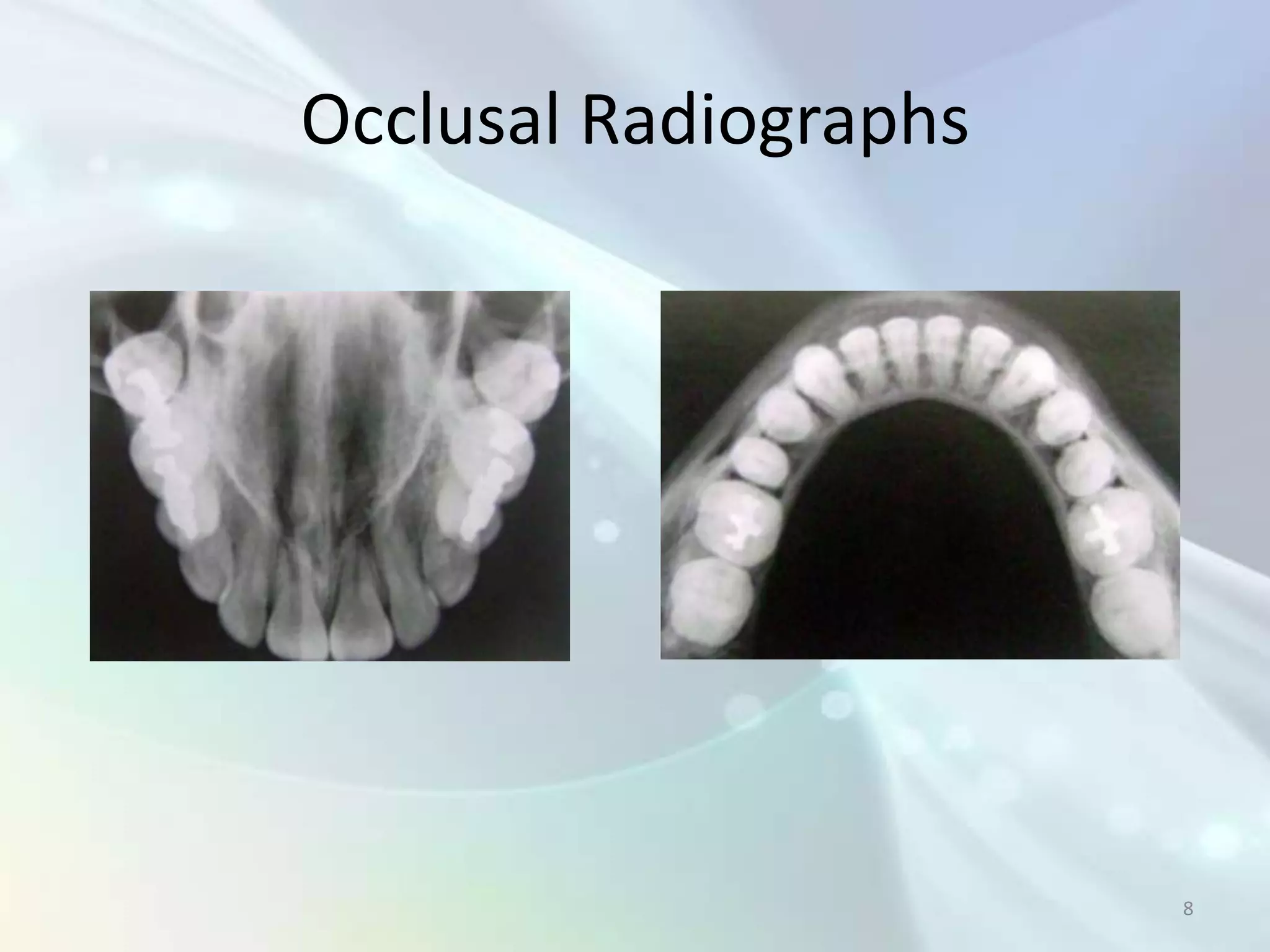
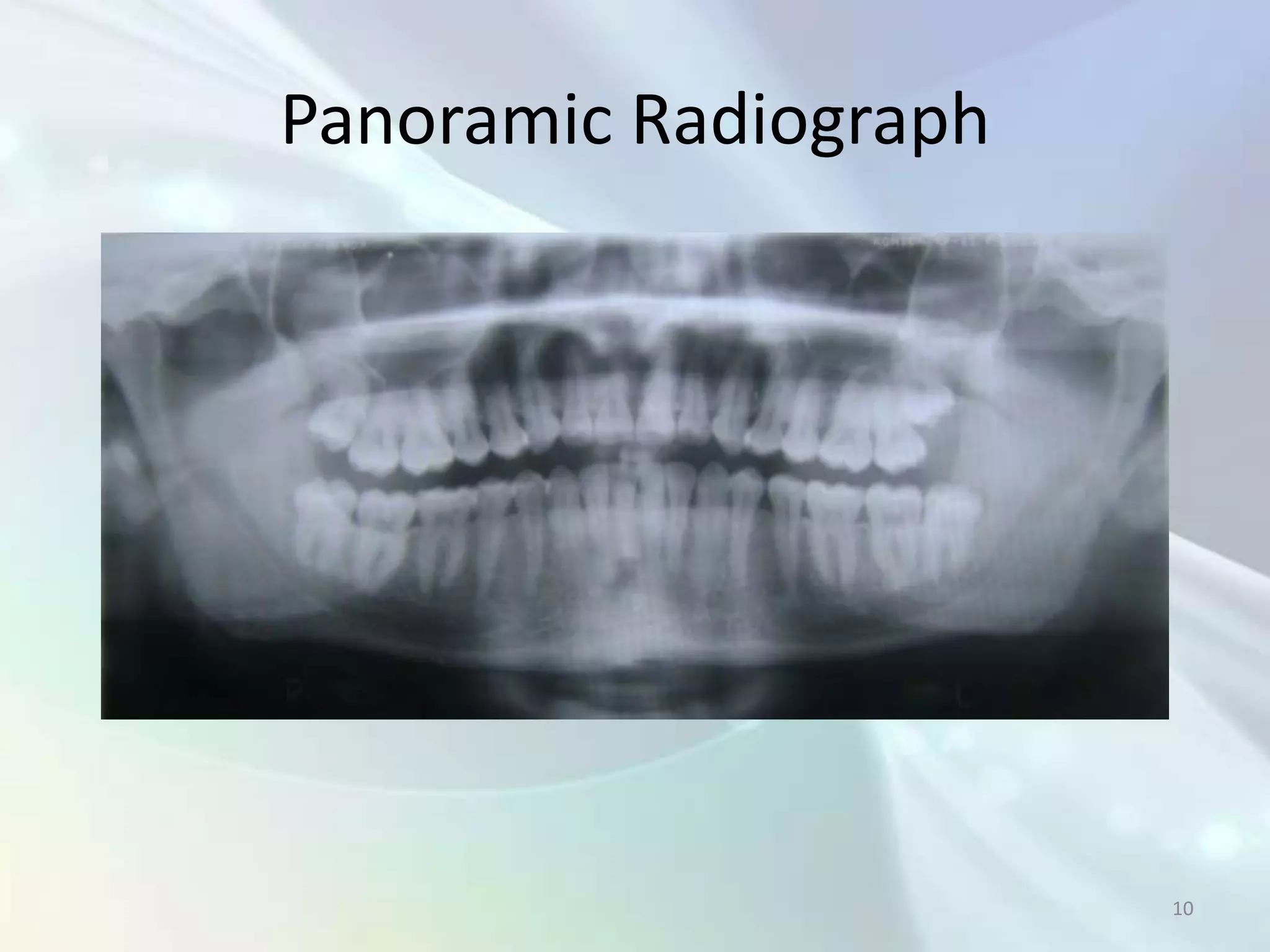
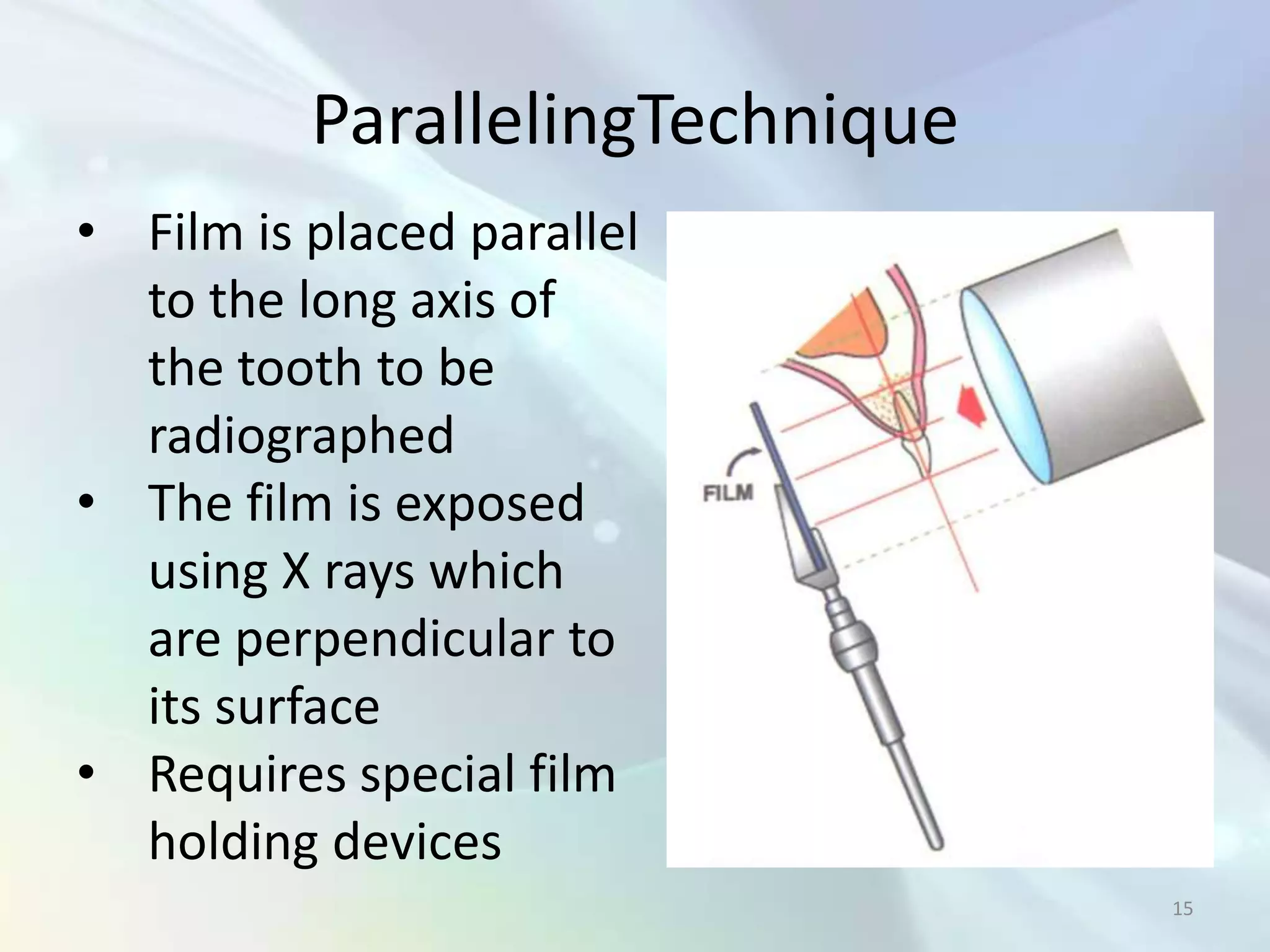
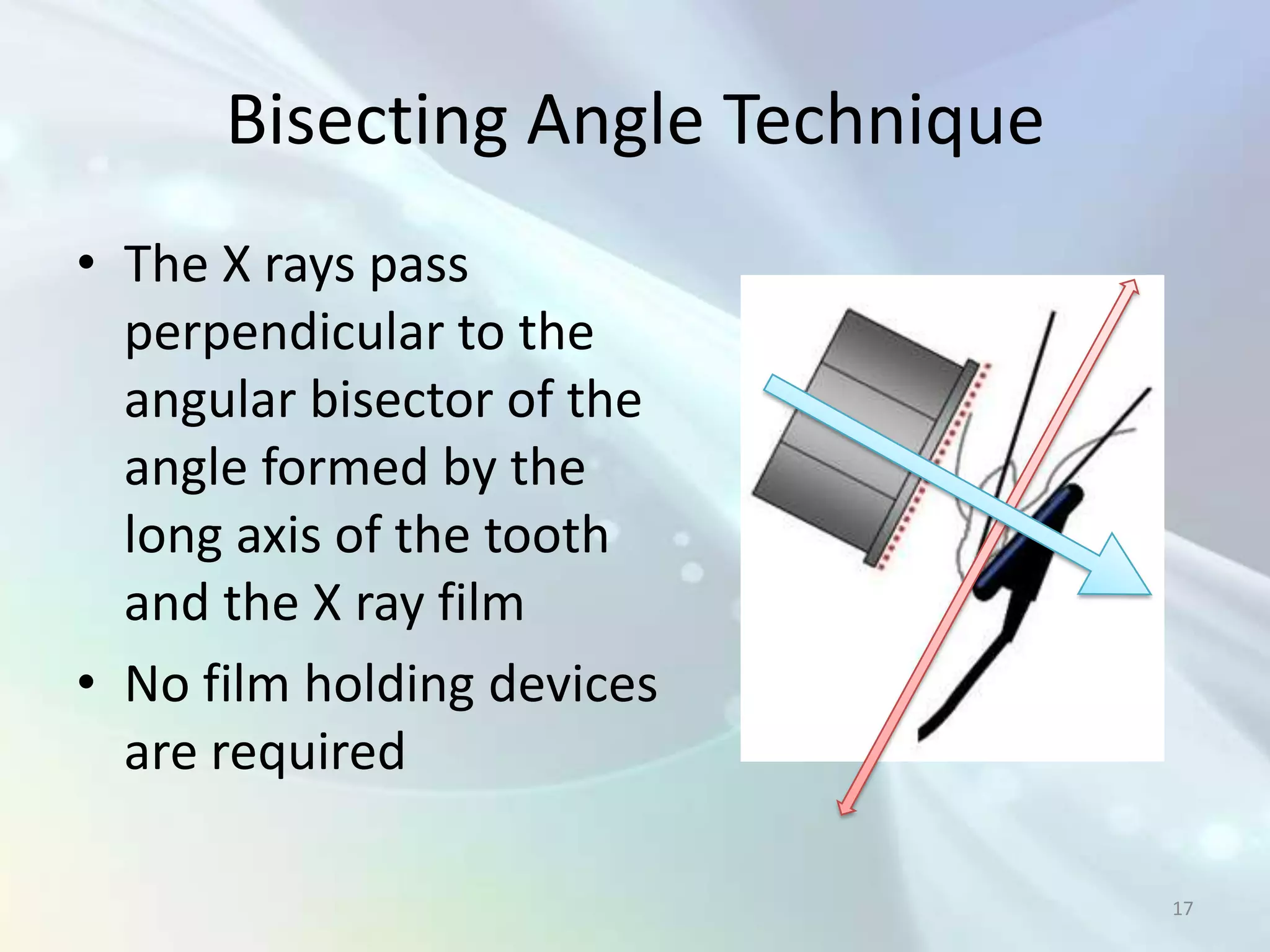
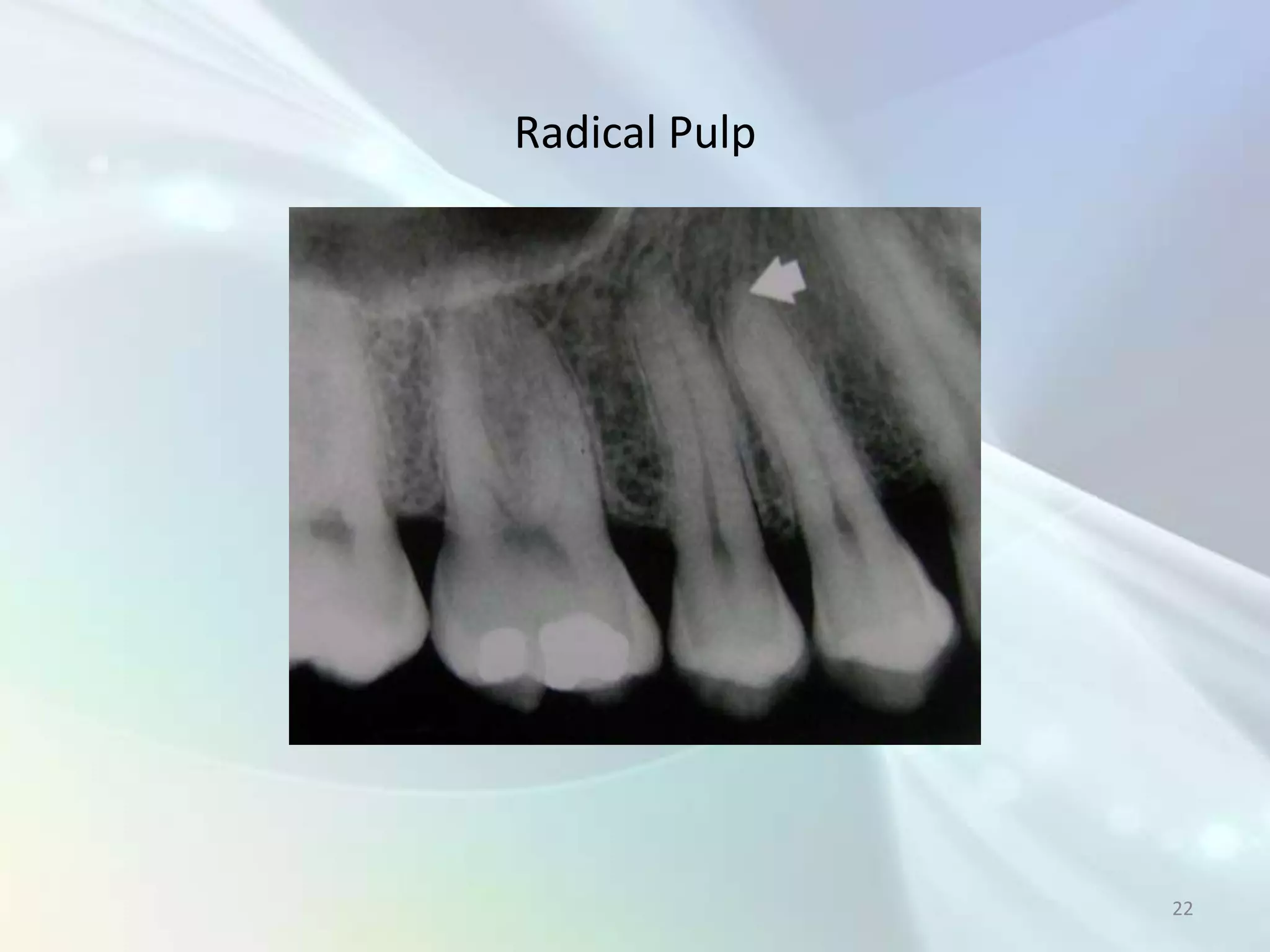
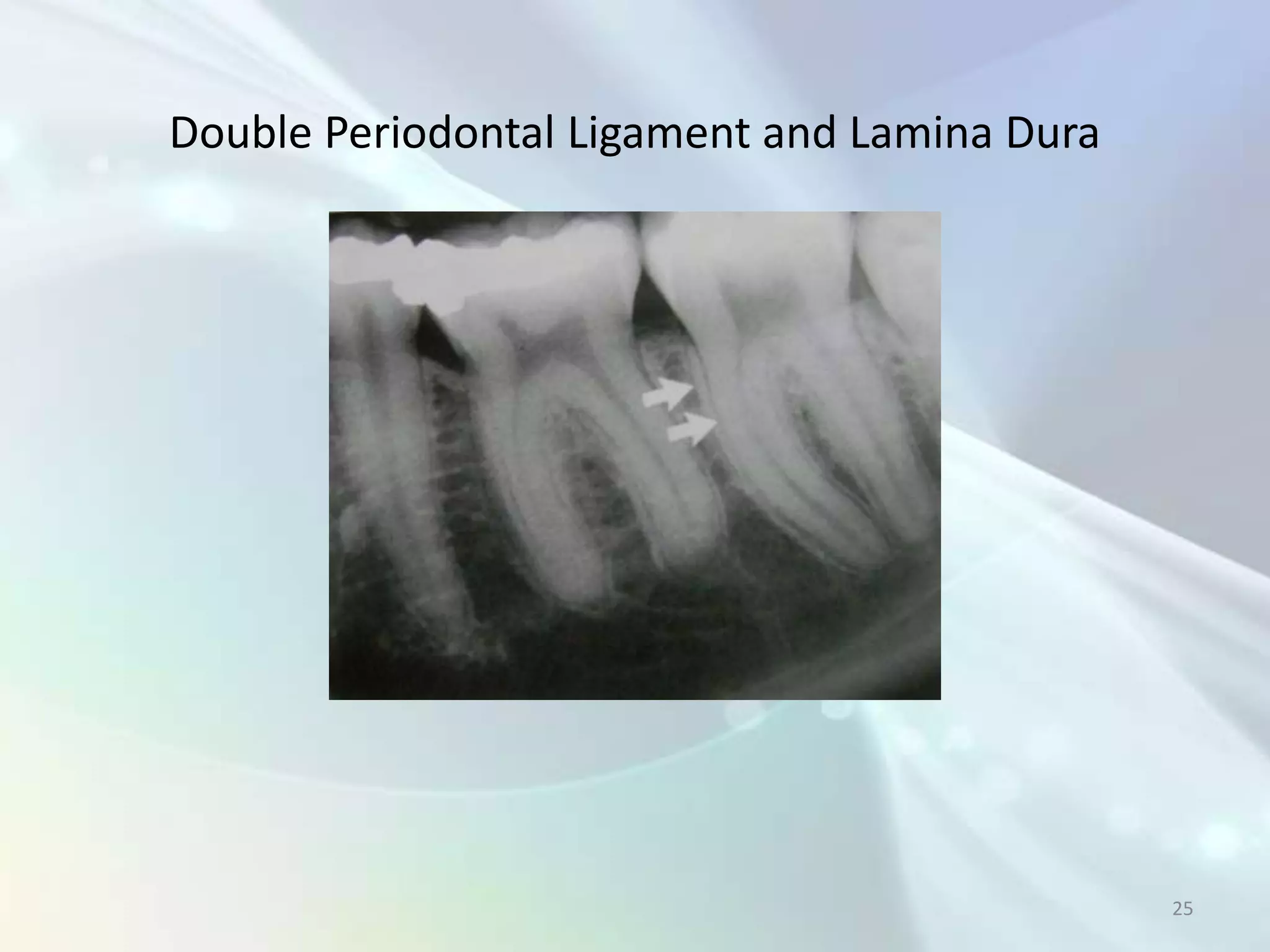
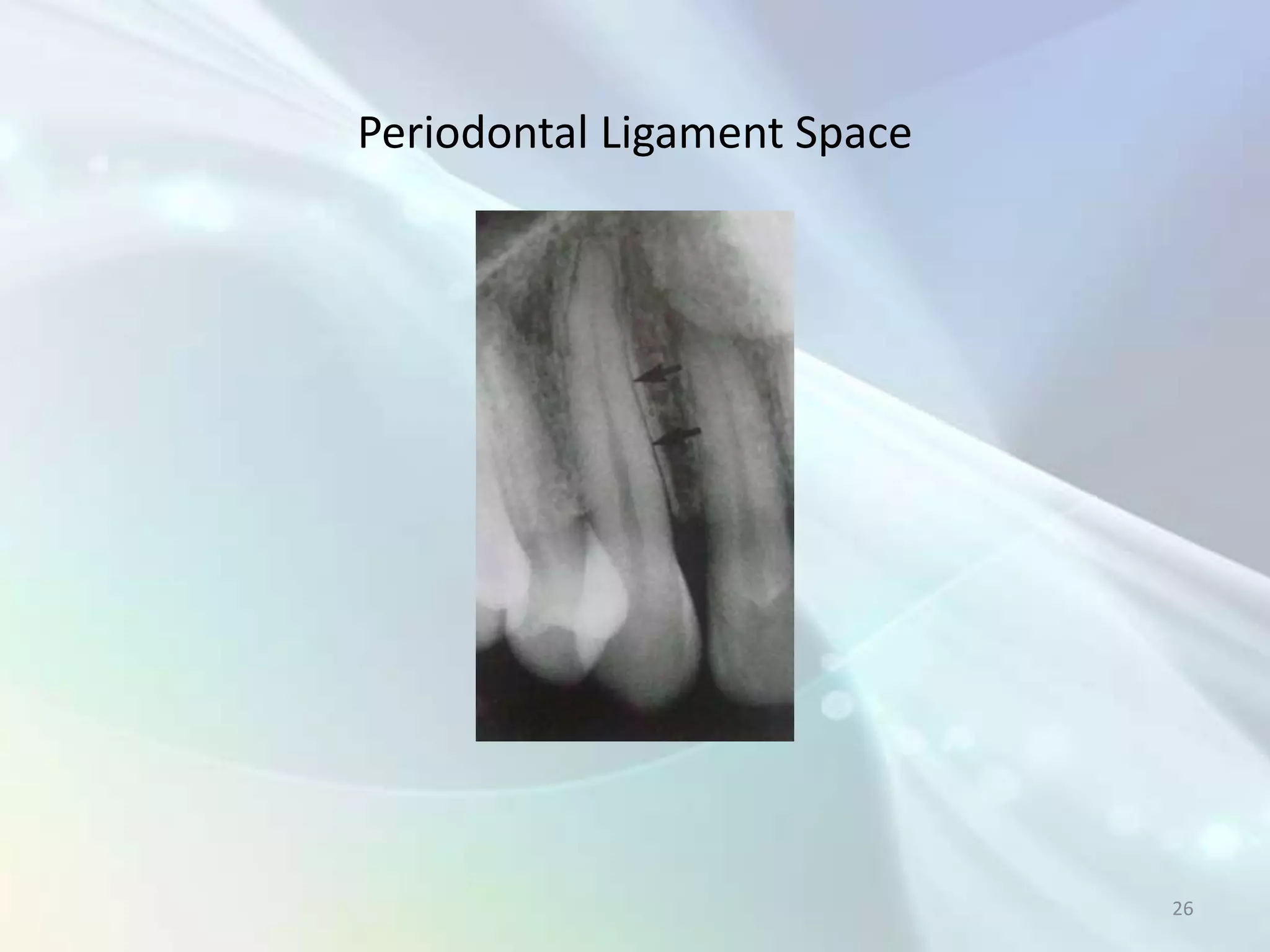
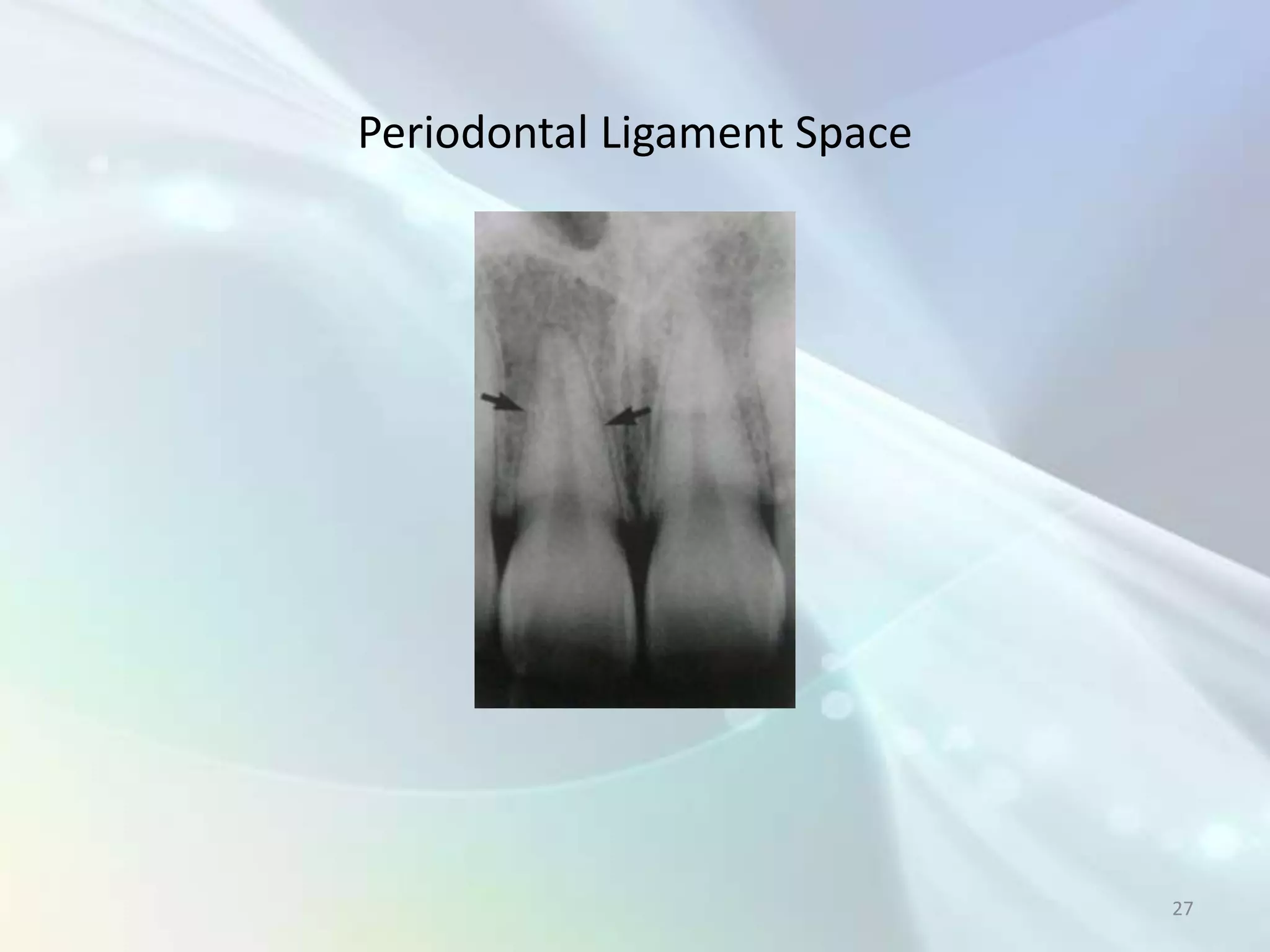
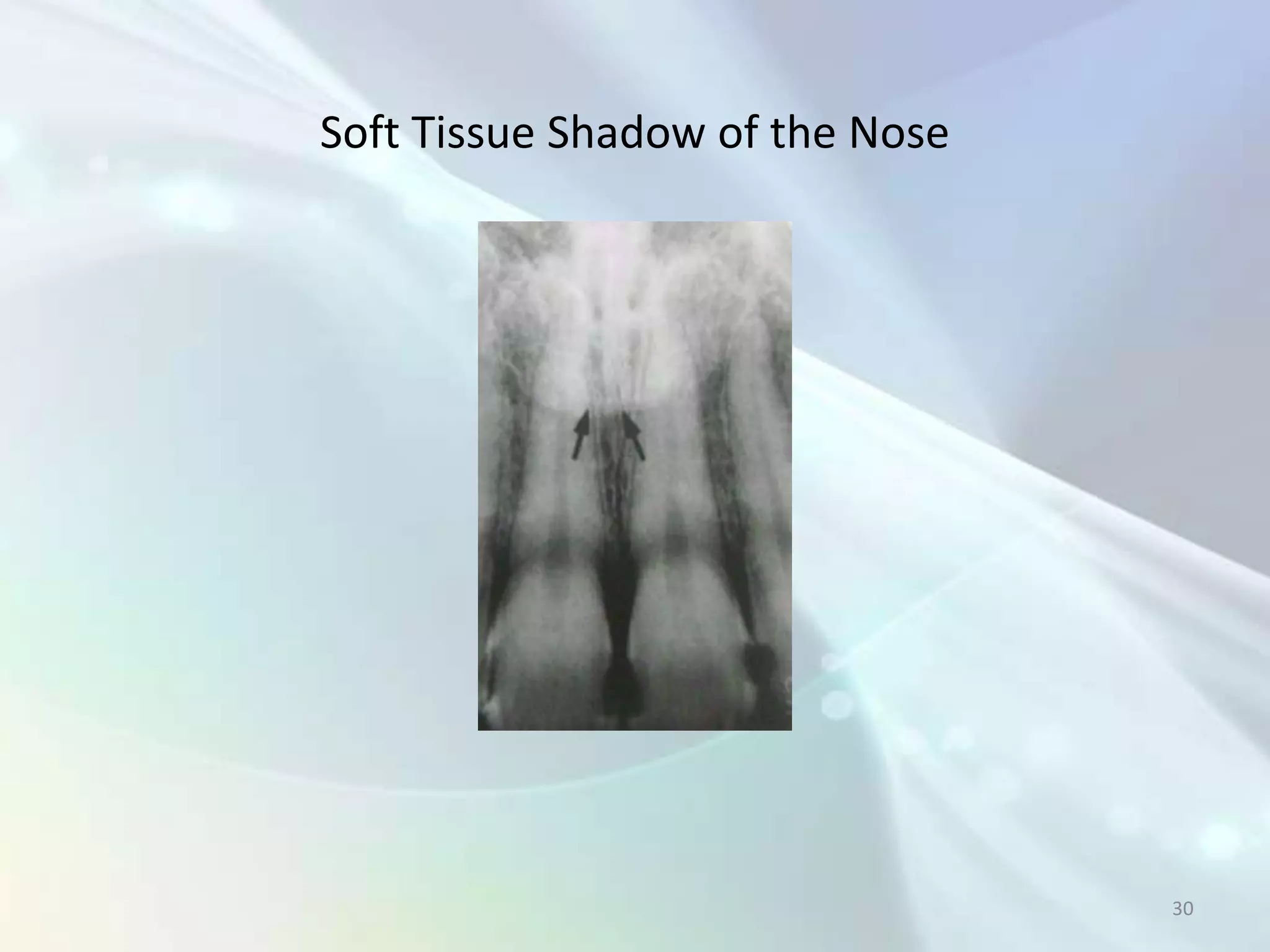
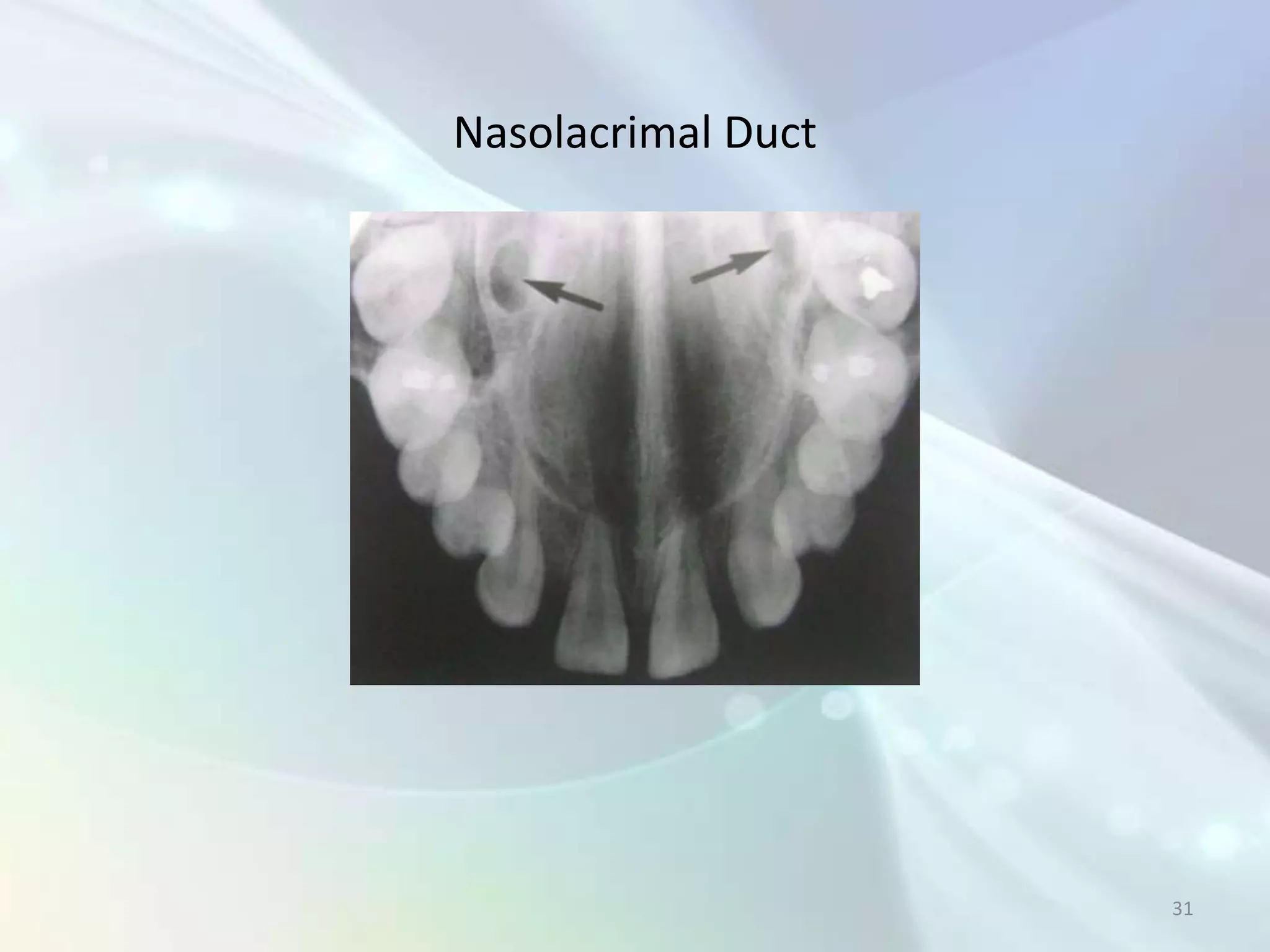
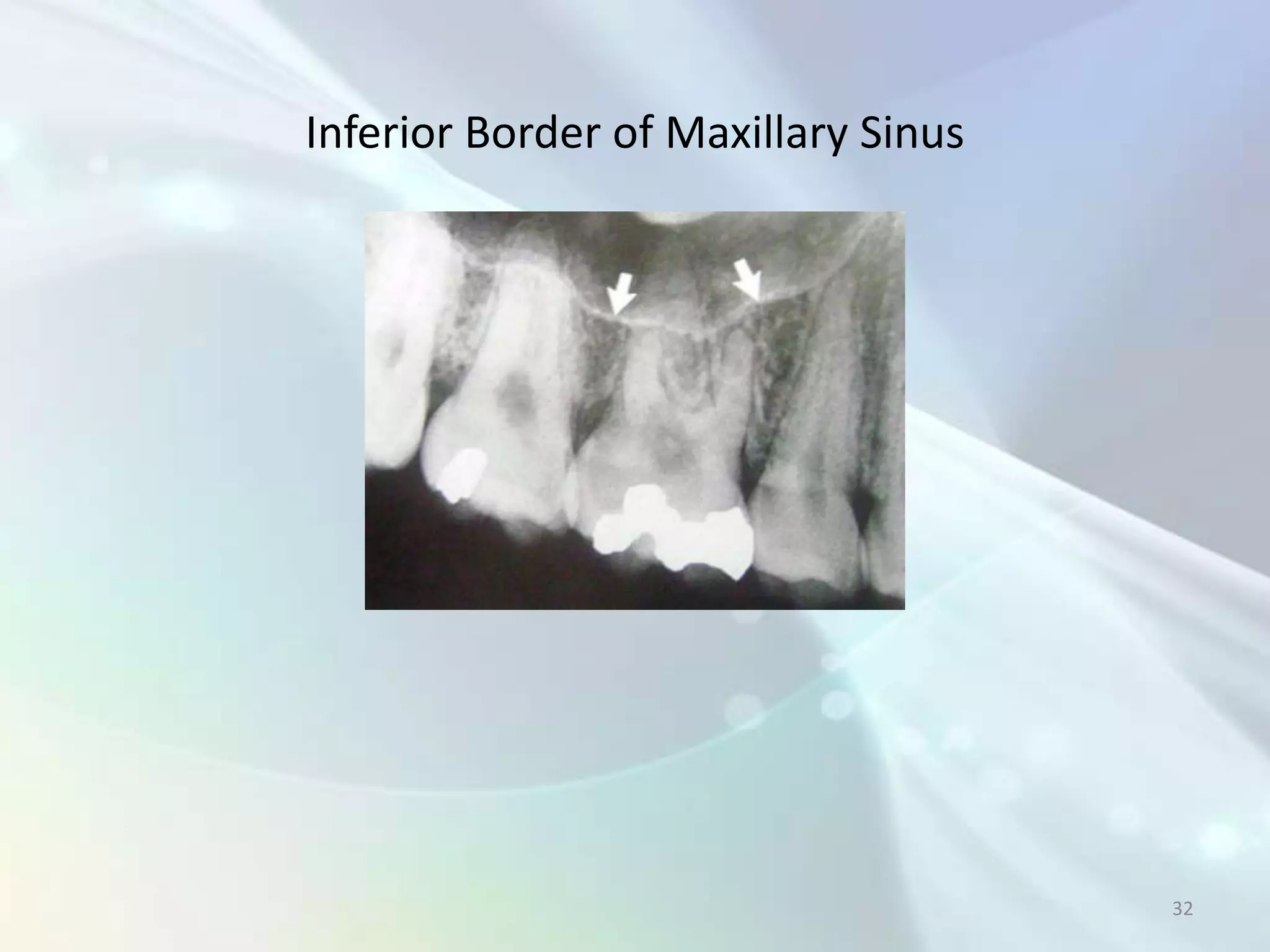
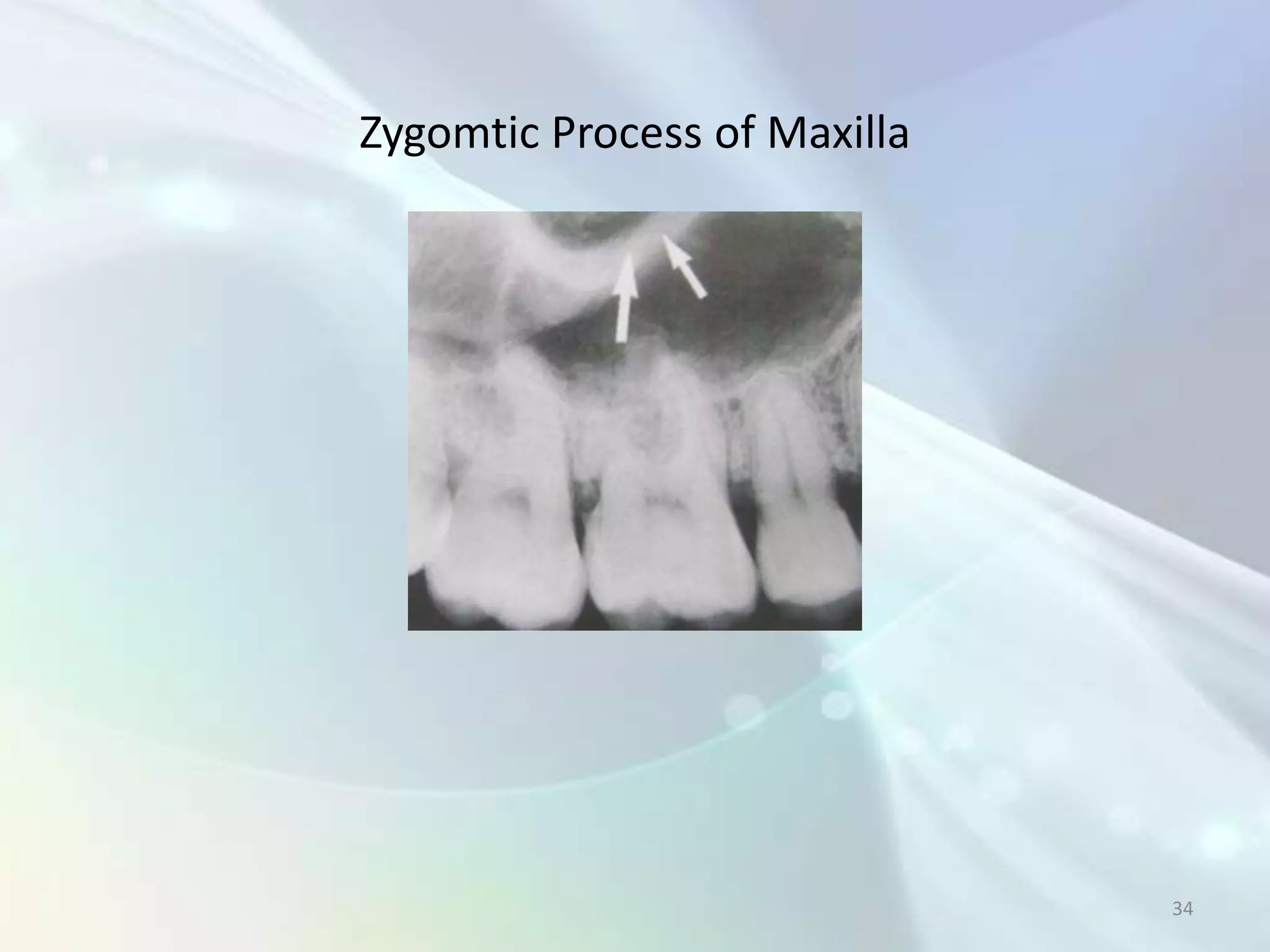
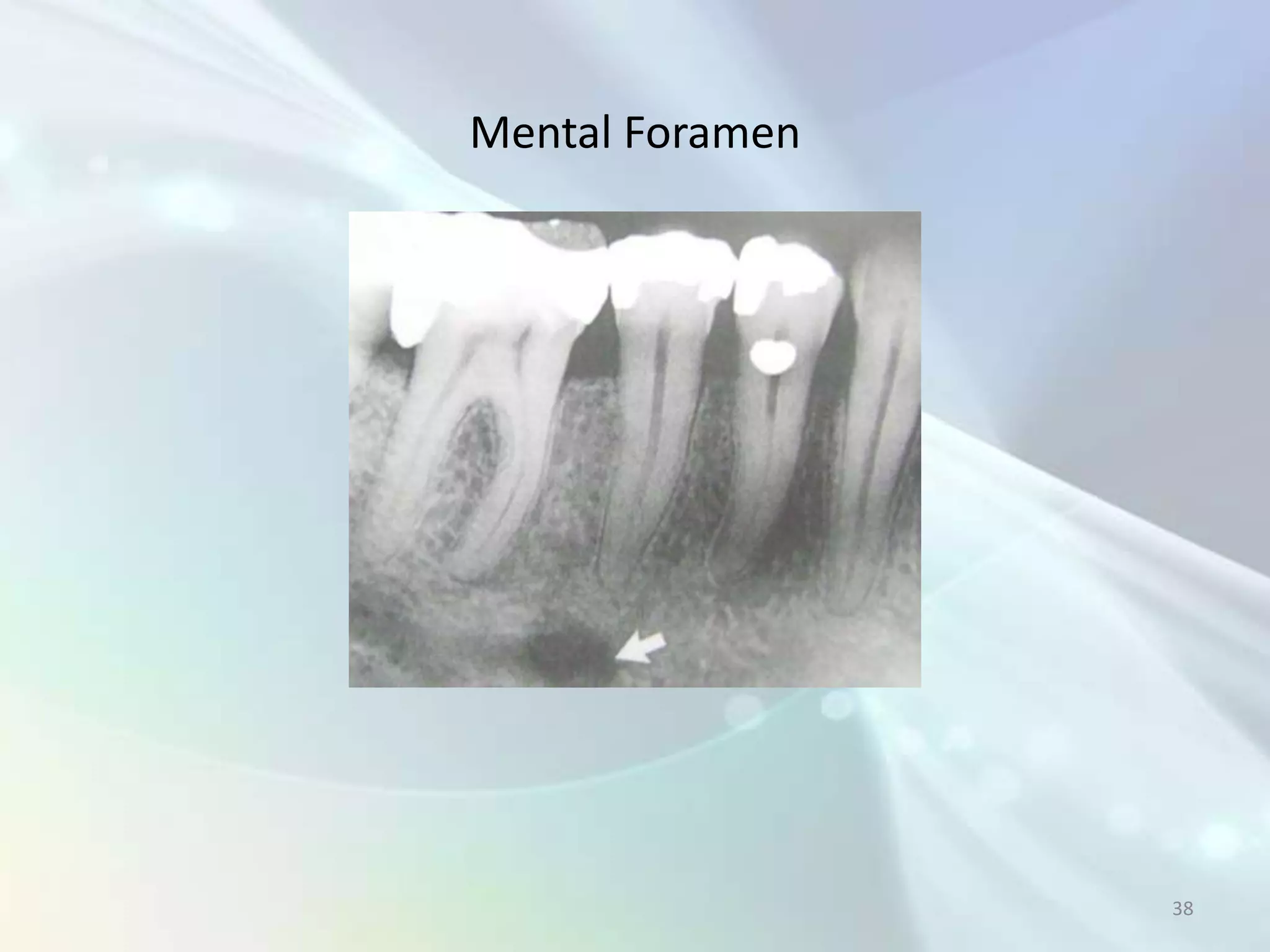
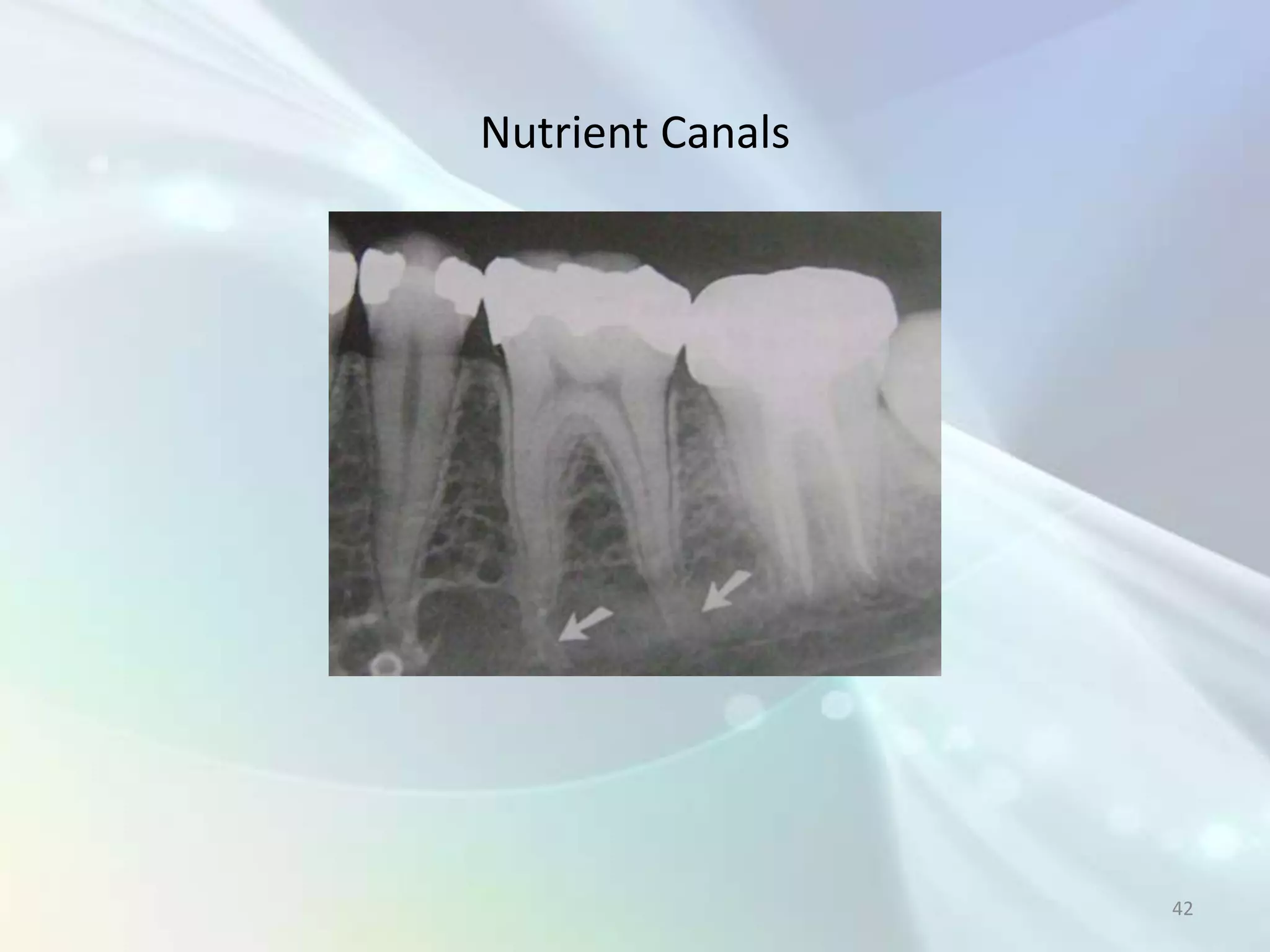
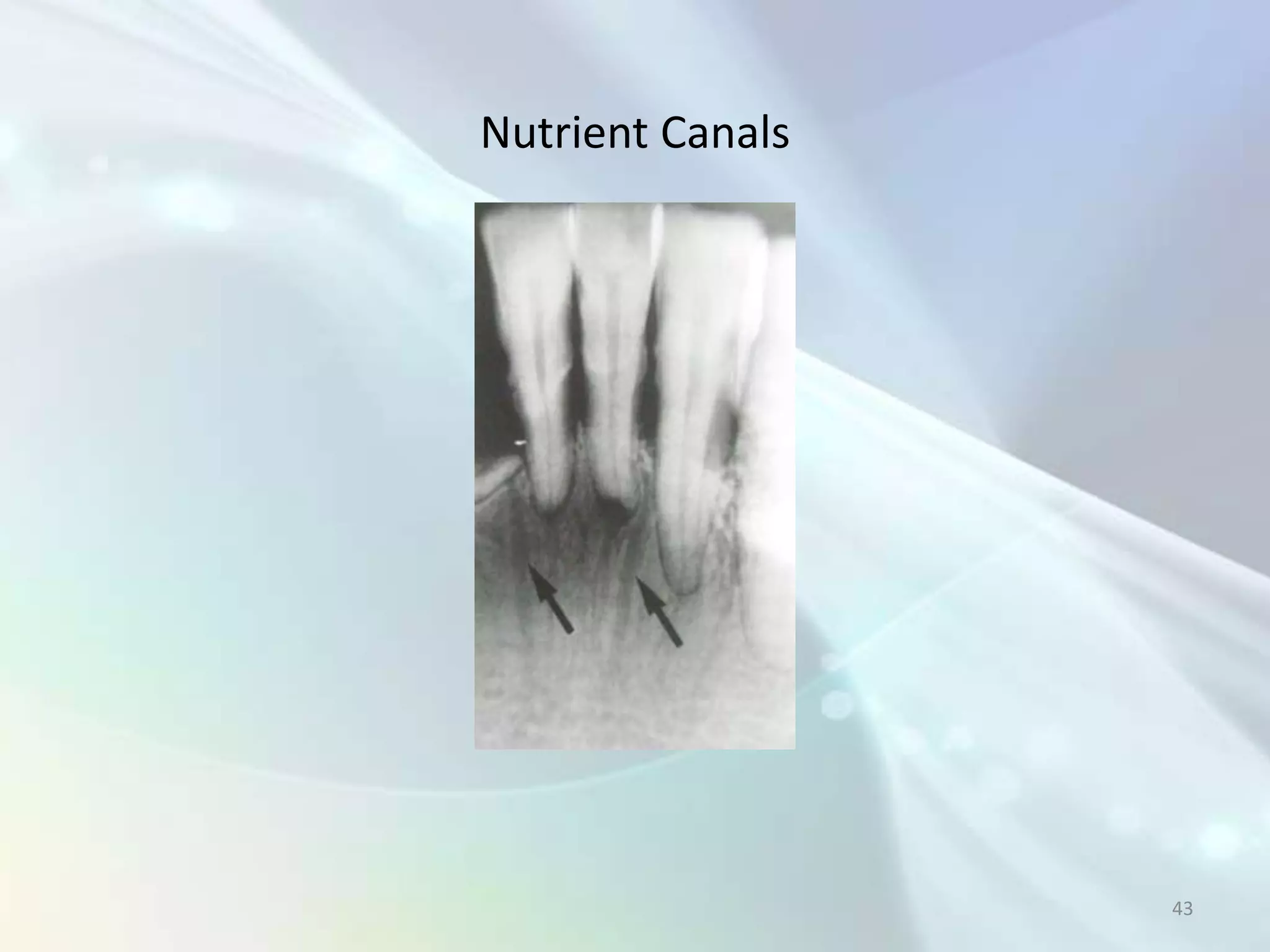
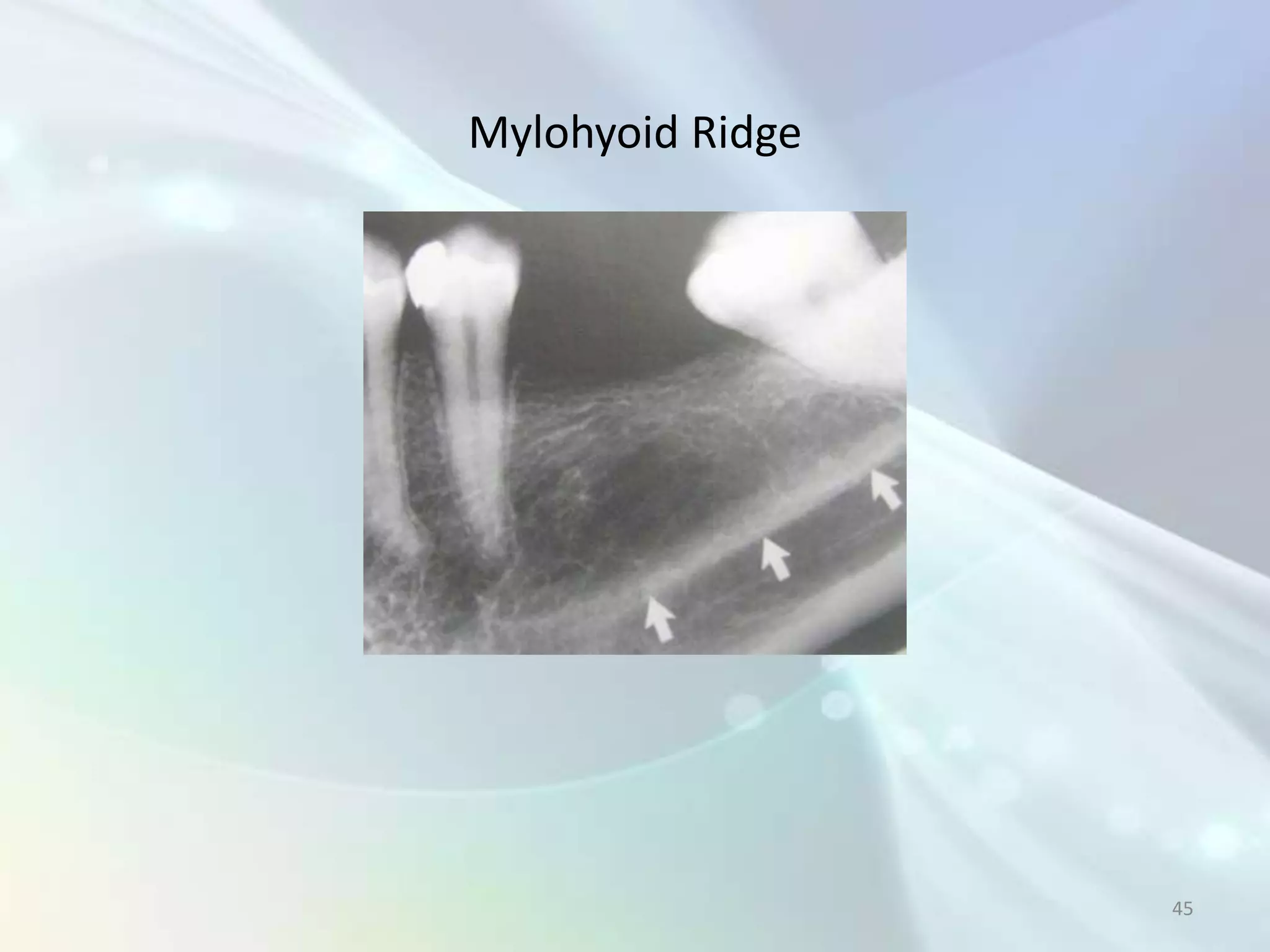
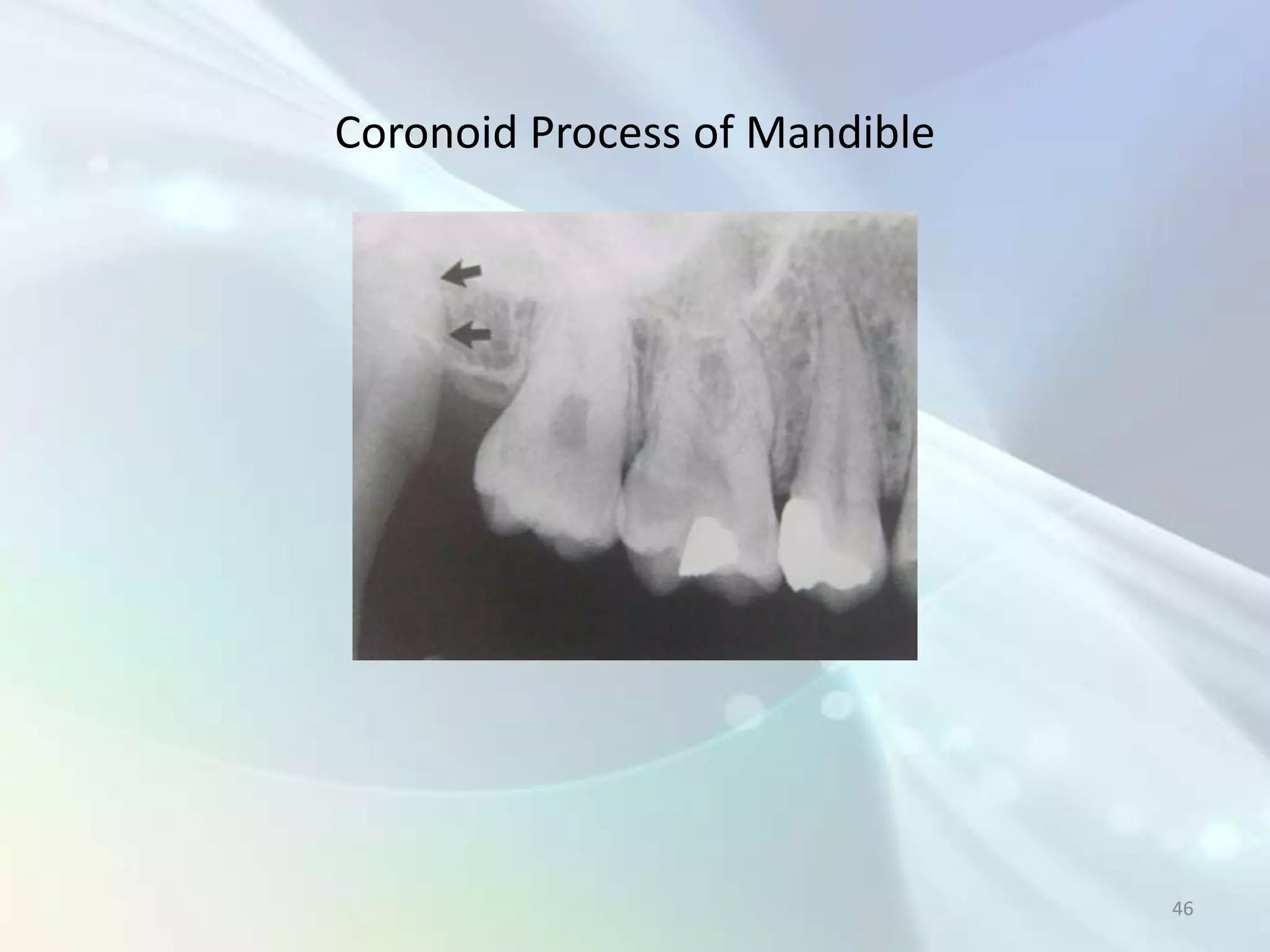
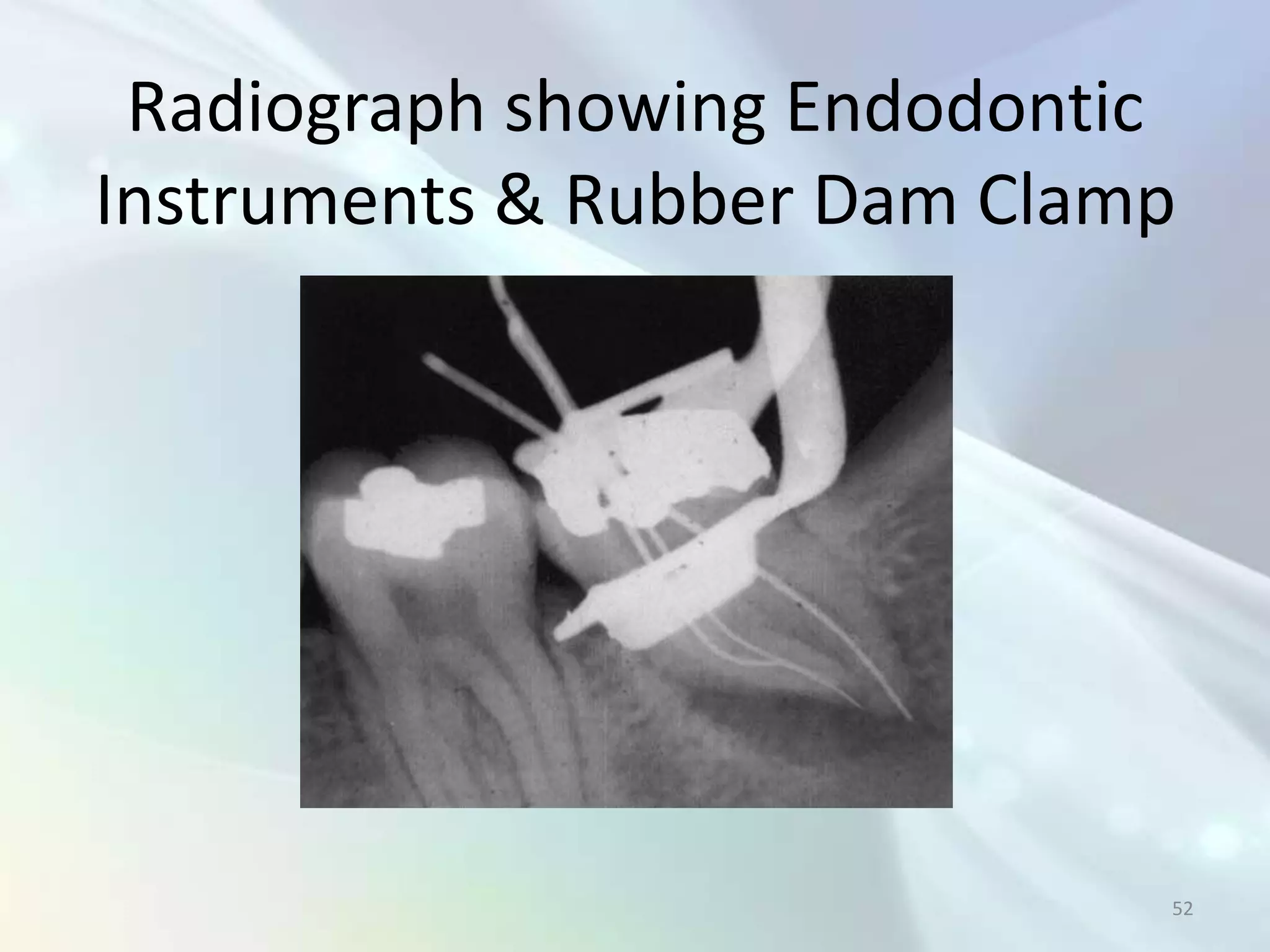
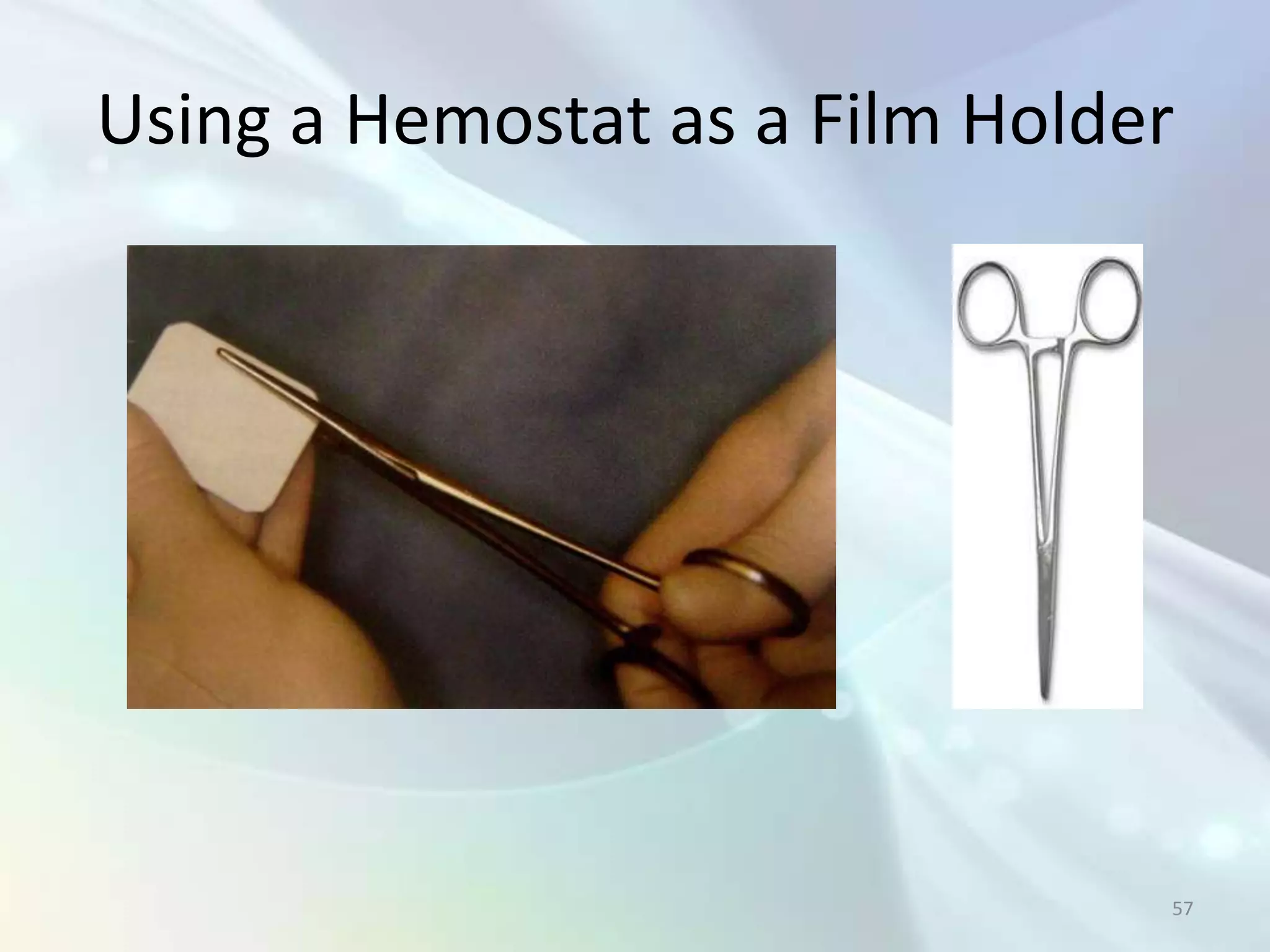
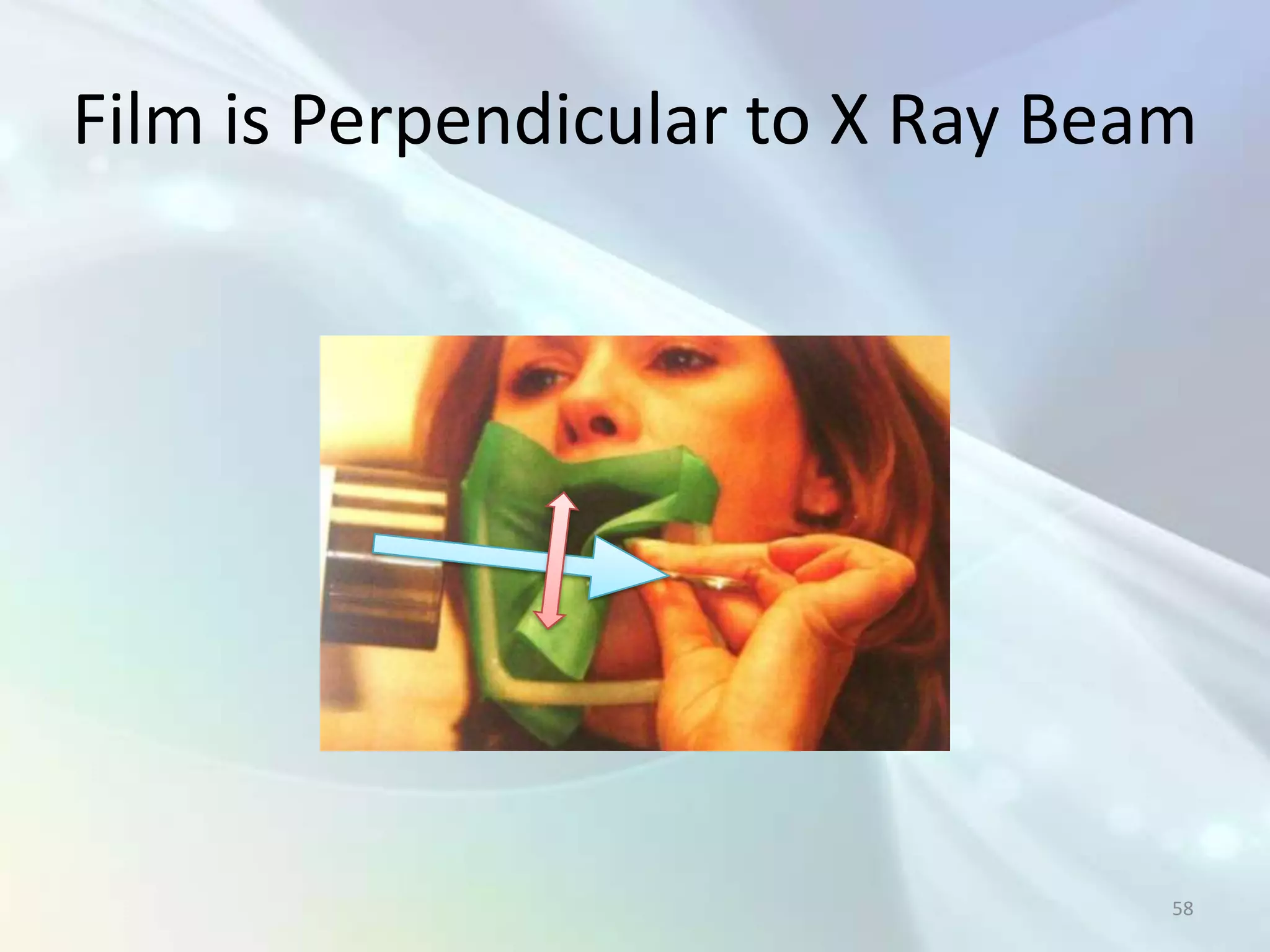
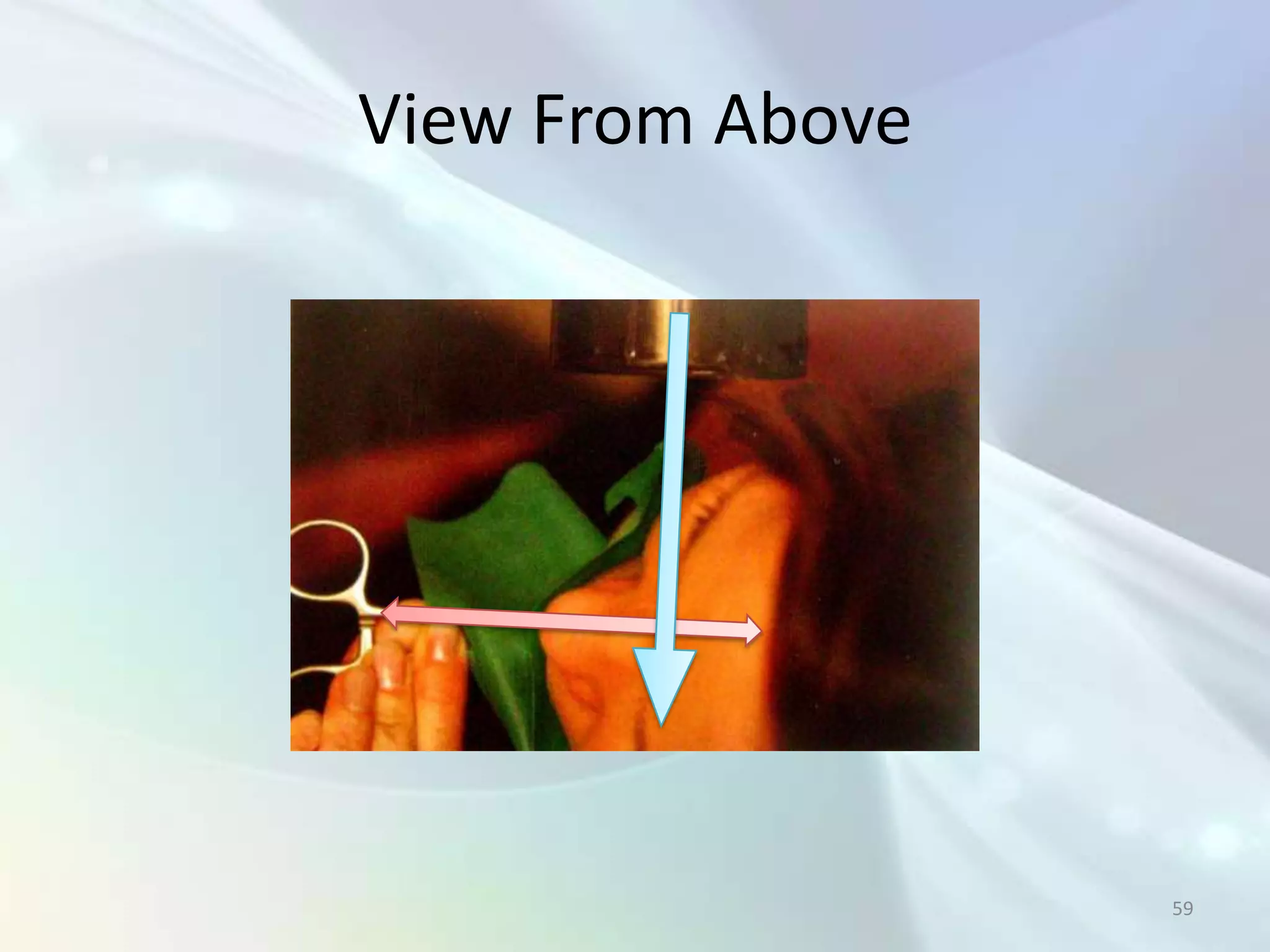
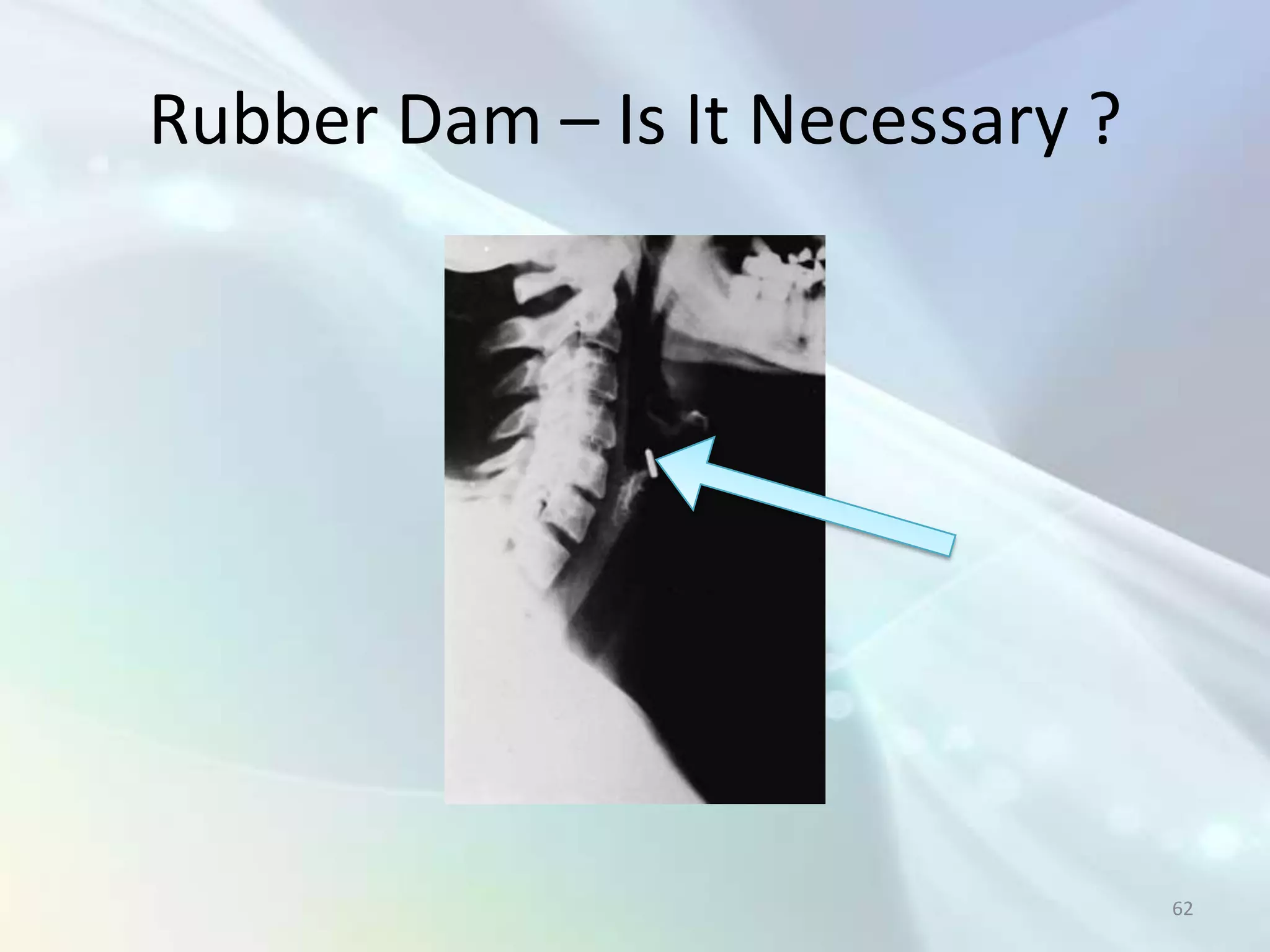
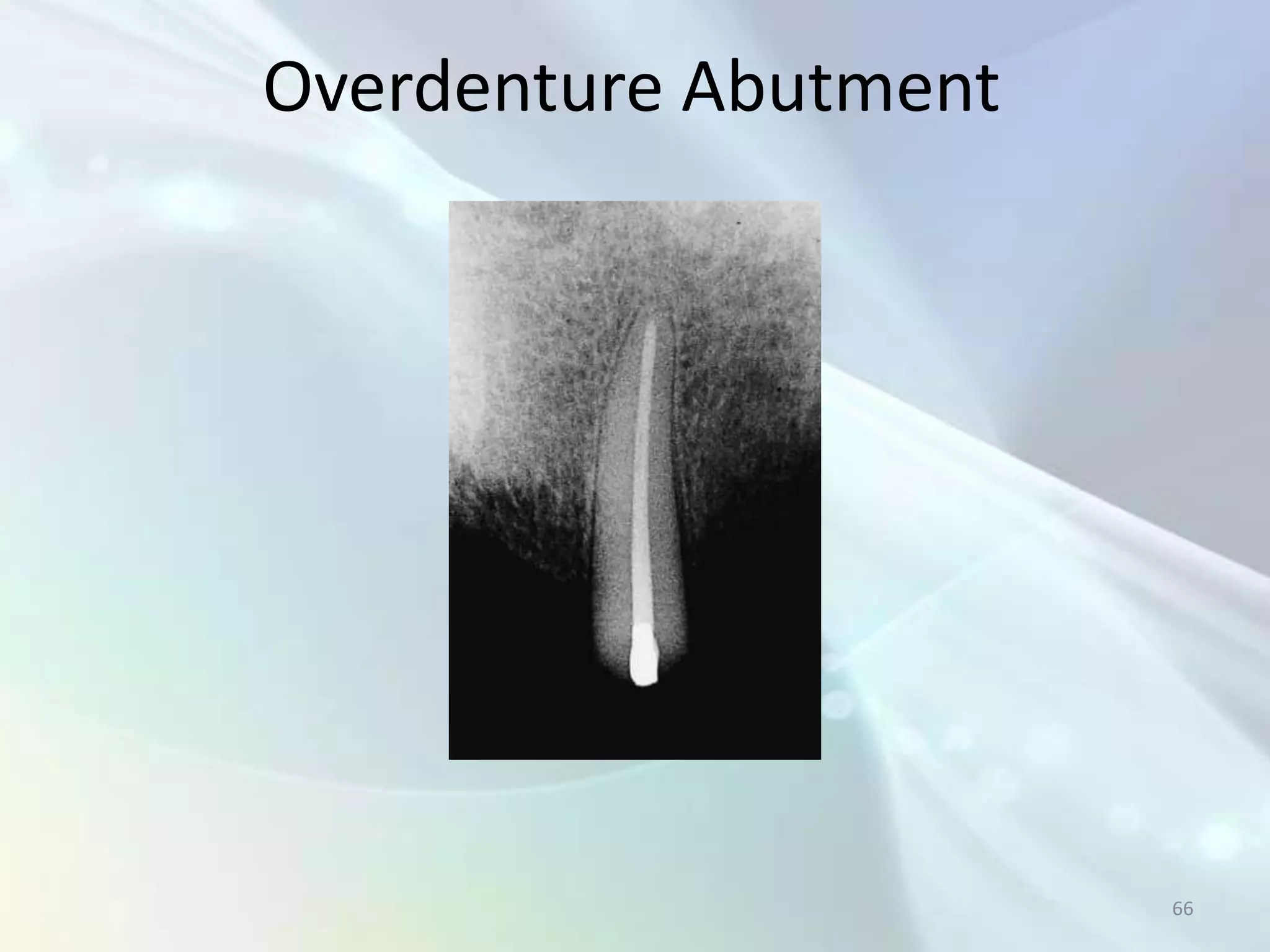
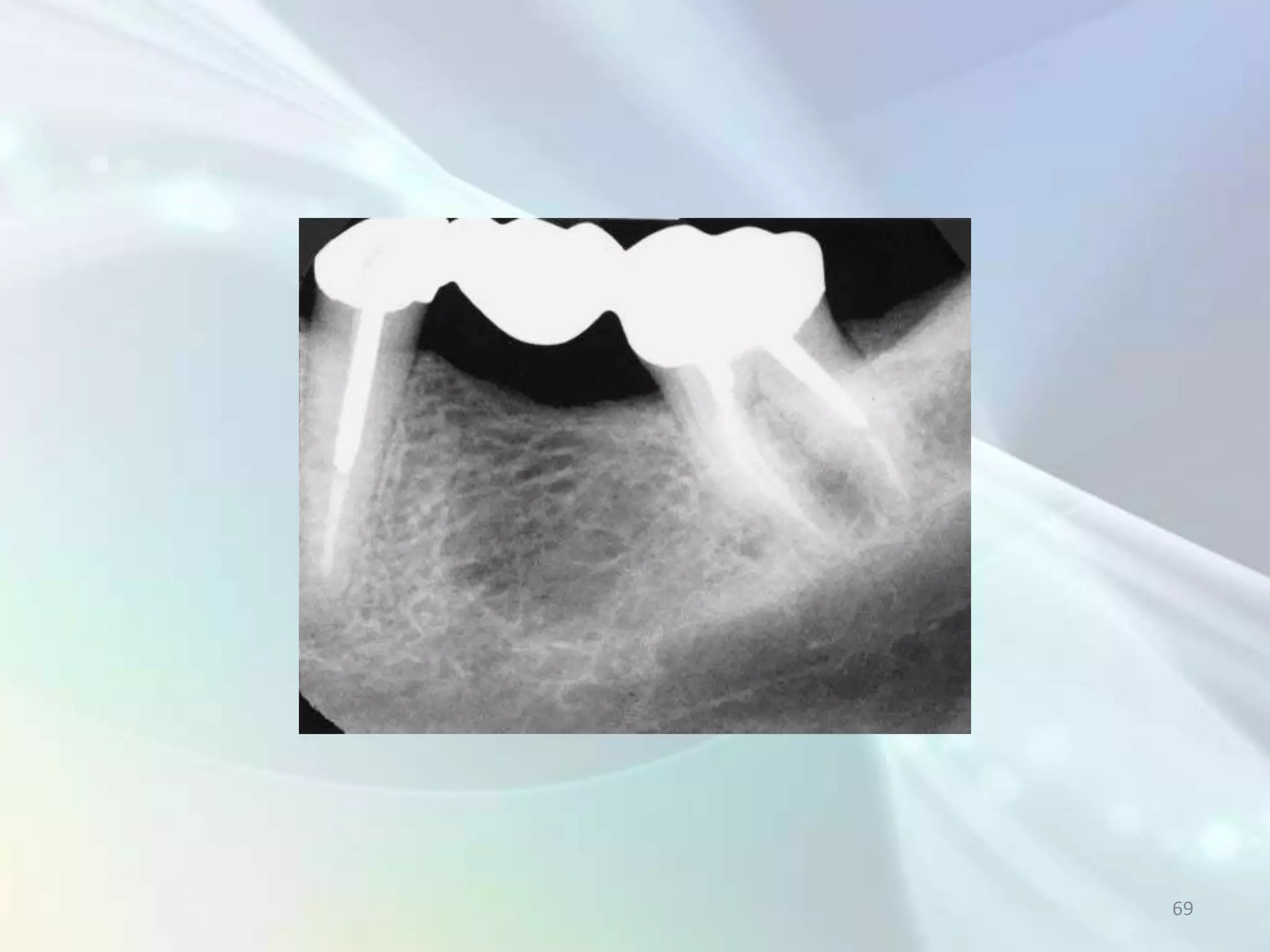
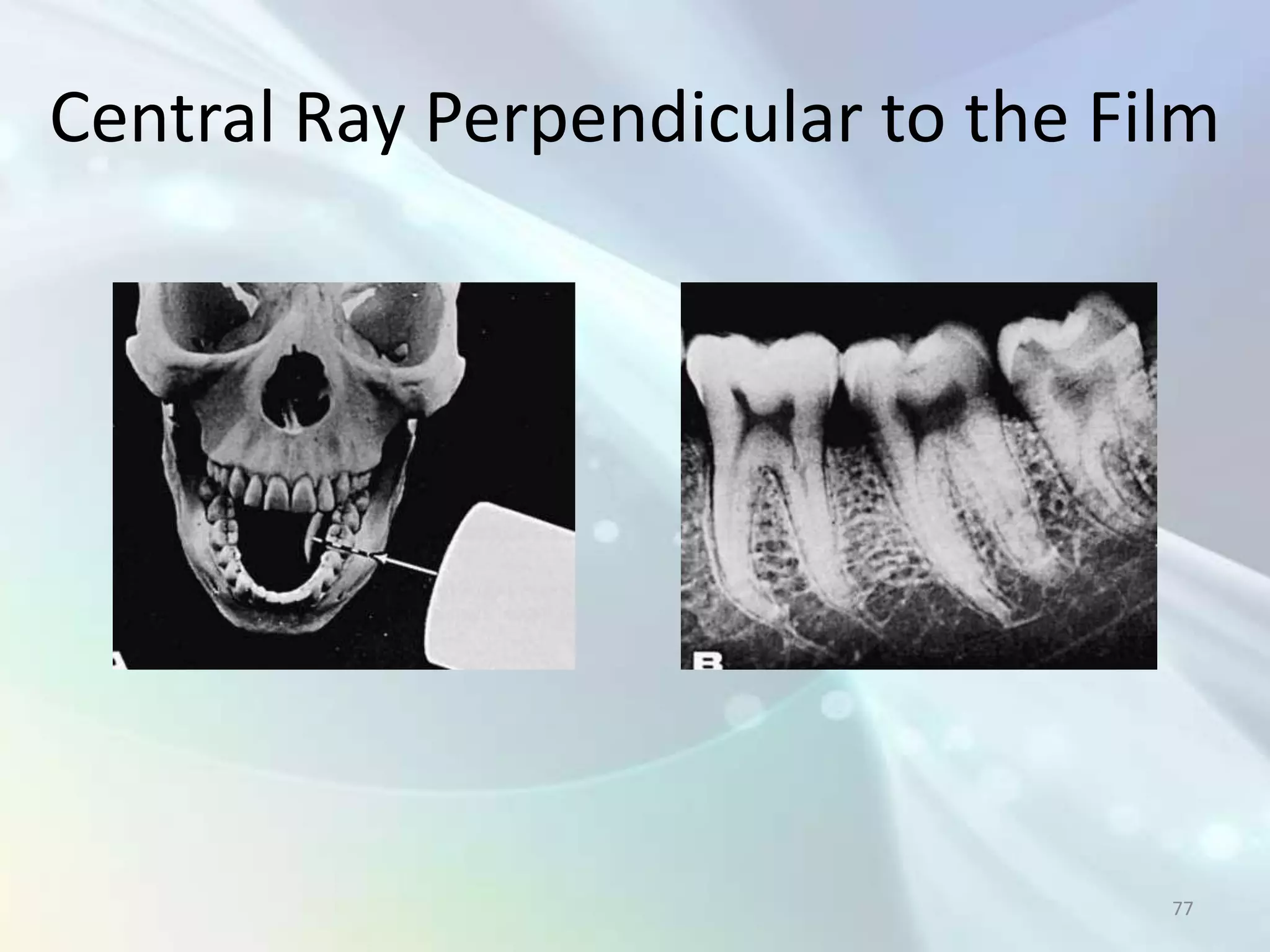
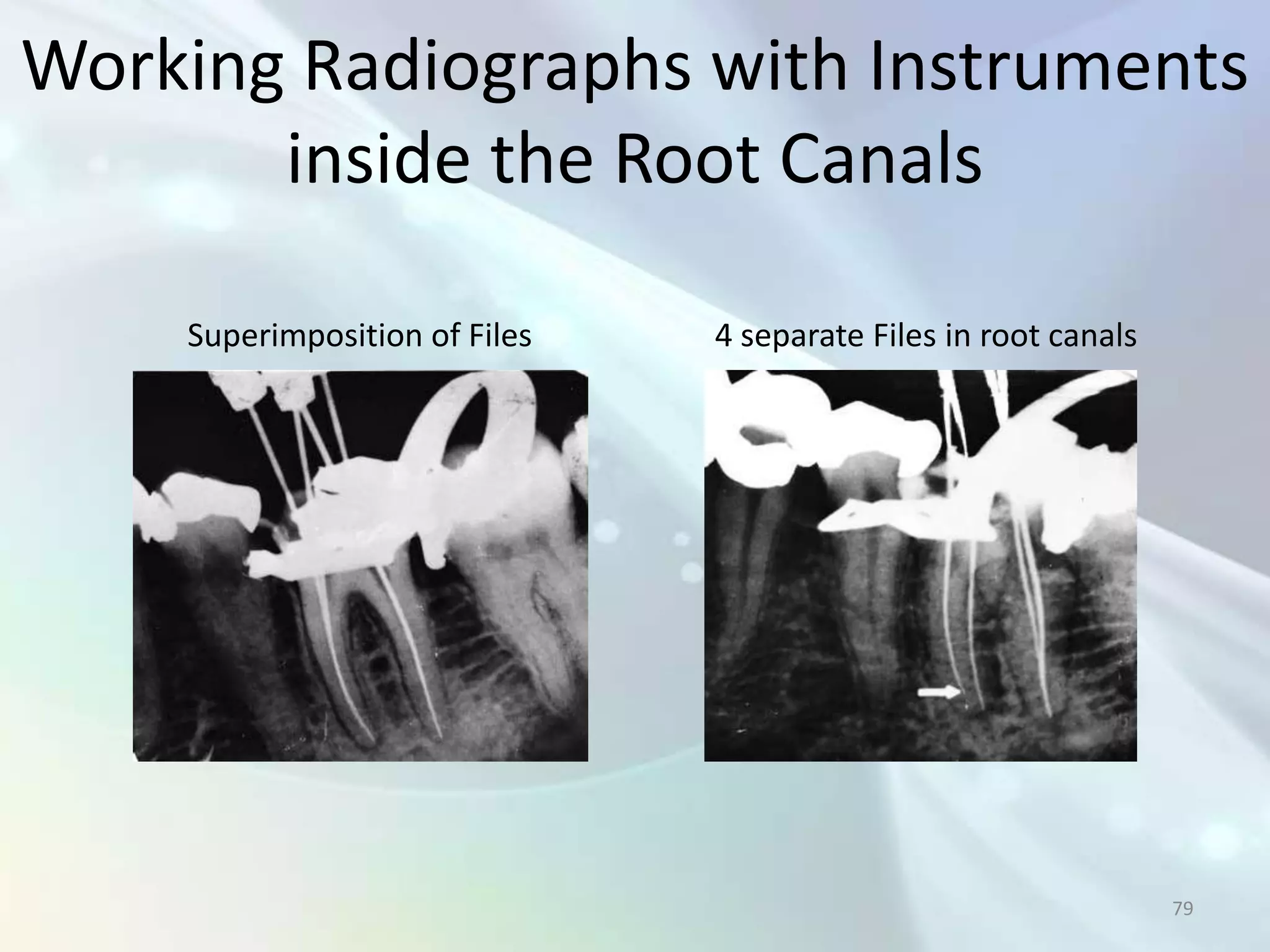
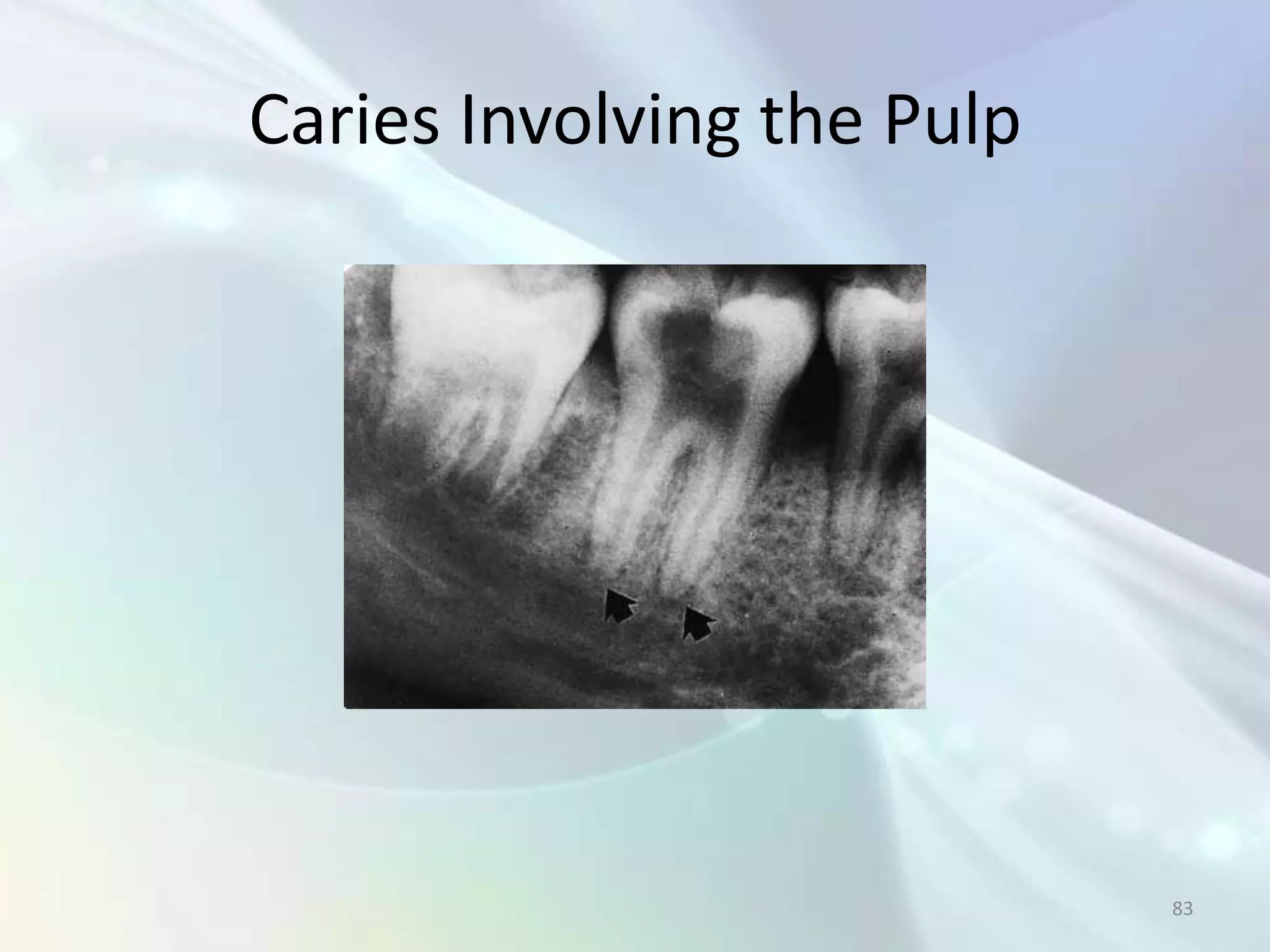
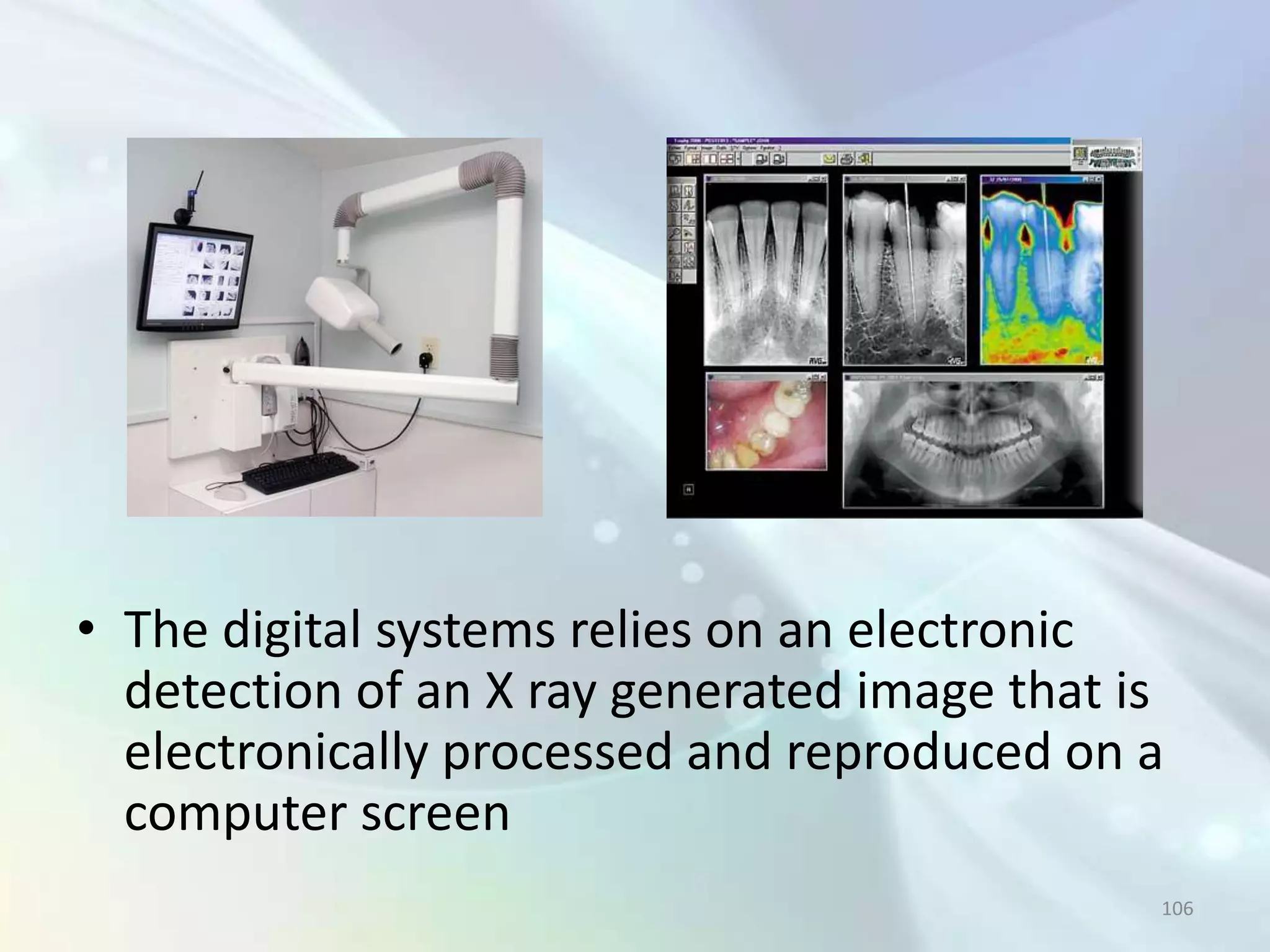
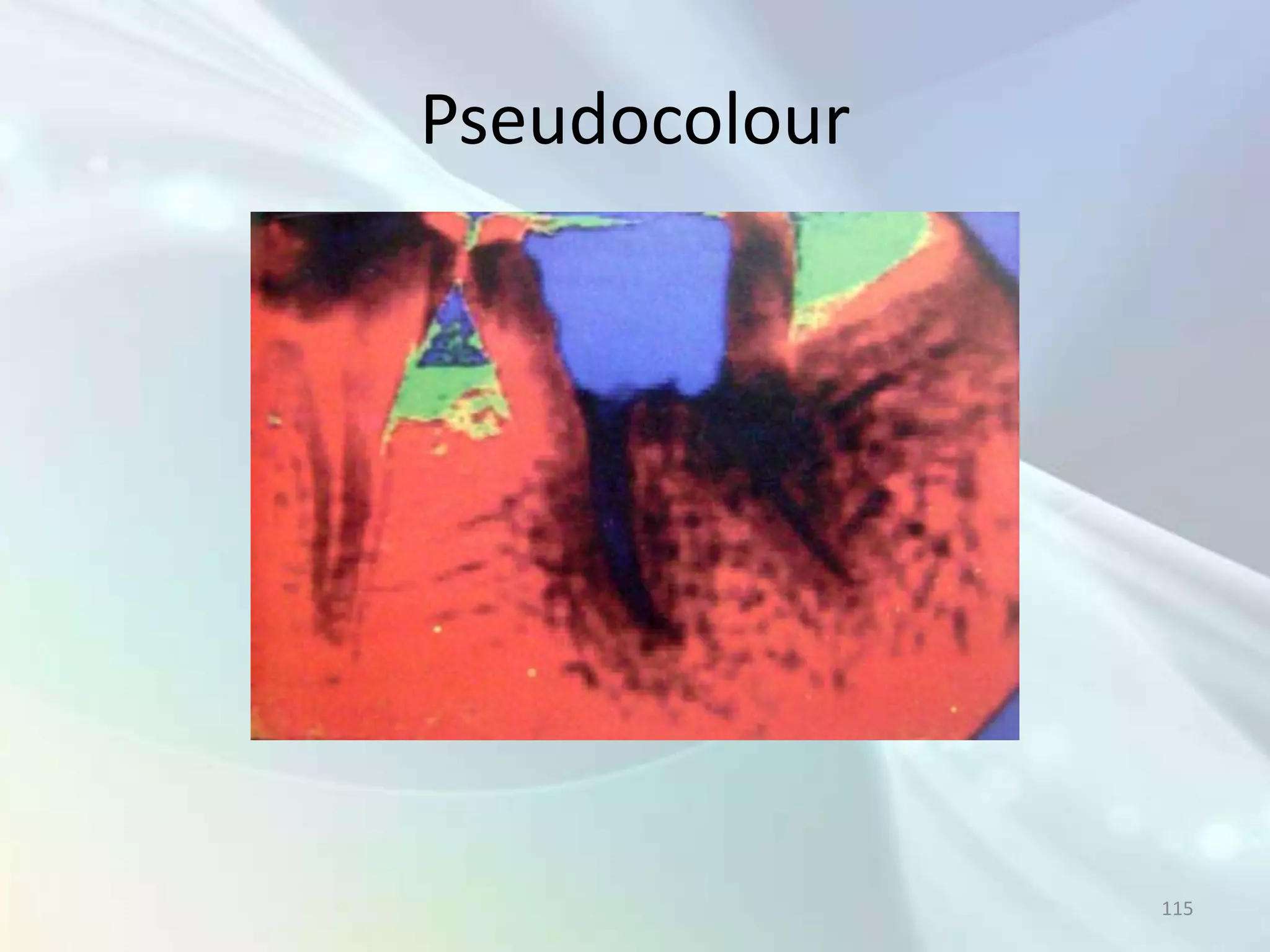
This document discusses the use of radiography in endodontics. It begins with a brief history of dental radiography and then covers topics like how to obtain good radiographs, relevant findings for endodontists, different types of radiographs used, and techniques for intraoral periapical radiographs. The document emphasizes the importance of radiographs for diagnosing issues, determining working lengths, evaluating treatment outcomes, and providing follow-up assessments. Both advantages and disadvantages of radiographs are outlined. Various anatomical landmarks are also identified on sample radiographs.