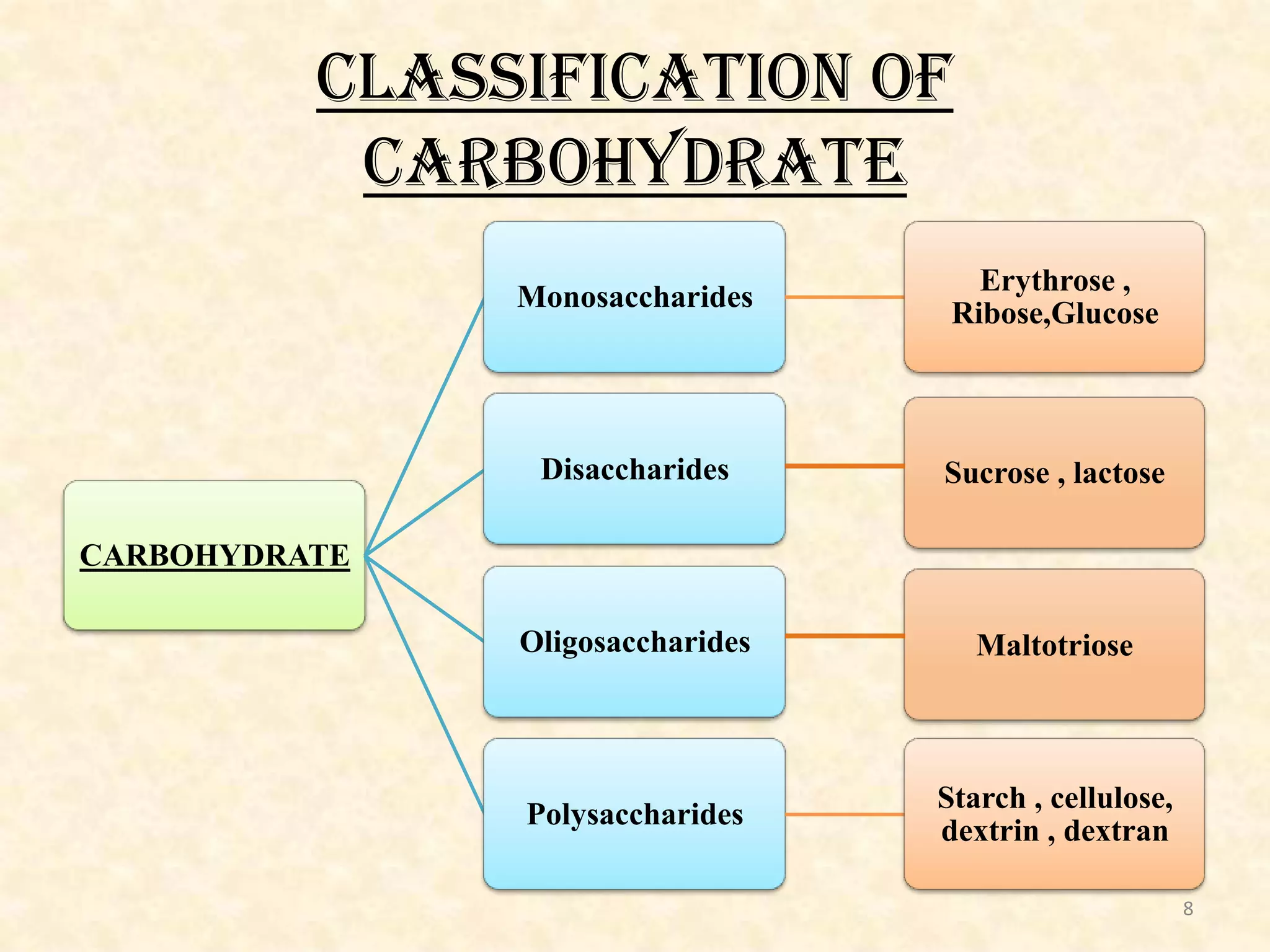
This document provides an overview of carbohydrate metabolism. It begins with an introduction to nutrition and carbohydrates, discussing the classification and functions of carbohydrates. It then describes the major metabolic pathways involved in carbohydrate metabolism, including glycolysis, the citric acid cycle, gluconeogenesis, and others. For each pathway, it provides details on the reactions, enzymes involved, energy production, and some clinical aspects. It also discusses the role of hormones in carbohydrate metabolism and dental aspects. The document concludes with a summary and references section.






![CARBOHYDRATE:
Most abundant organic molecule on earth.
Carbohydrates are defined as aldehyde or keto derivatives
of polyhydric alcohols.
For example: Glycerol on oxidation is converted to
D-glyceraldehyde, which is a carbohydrate derived from the
trihydric alcohol (glycerol).
All carbohydrates have the general formula CnH2nOn [or it
can be re-written as Cn(H2O)n ] .
7](https://image.slidesharecdn.com/carbohydratemetabolism-140214034339-phpapp01/75/Carbohydrate-metabolism-7-2048.jpg)










![• Glucose is phosphorylated to glucose-6-phosphate by hexokinase (or) glucokinase.
Energy
Investment
Phase
• Glucose-6-phosphate undergoes isomerization to give fructose -6- phosphate in the presense of
phospho-hexose isomerase and Mg2+
• Fructose-6-phosphate is phoshorylated to fructose 1,6-bisphosphate by phosphofructokinase.
• Fructose 1,6-bisphosphate glyceraldehyde 3-phosphate + dihydroxyacetone
phosphate.(aldolase enzyme)
Splitting
Phase
• 2 molecules of glyceraldehyde 3-phosphate are obtained from 1 molecule of glucose
• Glyceraldehyde 3-phosphate 1,3-bisphosphoglycerate(glyceraldehyde 3-phosphate hydrogenase )
• 1,3-bisphosphoglycerate 3-phosphoglycerate (phosphoglycerate kinase)
• 3-phosphoglycerate 2-phosphoglycerate (phosphoglycerate mutase)
Energy
Generation
Phase
• 2-phosphoglycerate phosphoenol pyruvate (enolase + Mg2+ & Mn2+)
• Phosphoenol pyruvate pyruvate [enol] (pyruvate kinase ) pyruvate [keto] L-Lactate
(lactate dehydrogenase)
19](https://image.slidesharecdn.com/carbohydratemetabolism-140214034339-phpapp01/75/Carbohydrate-metabolism-19-2048.jpg)

































![Clinical Aspects
• Glucose-6-Phosphate dehydrogenase
deficiency :
- Inherited sex-linked trait
- Red blood cells
- Impaired synthesis of NADPH
- hemolysis , developing hemolytic anemia
Resistance towards malaria [Africans]
53](https://image.slidesharecdn.com/carbohydratemetabolism-140214034339-phpapp01/75/Carbohydrate-metabolism-53-2048.jpg)







































