The document discusses ketone bodies, ketogenesis, and ketolysis. It provides details on:
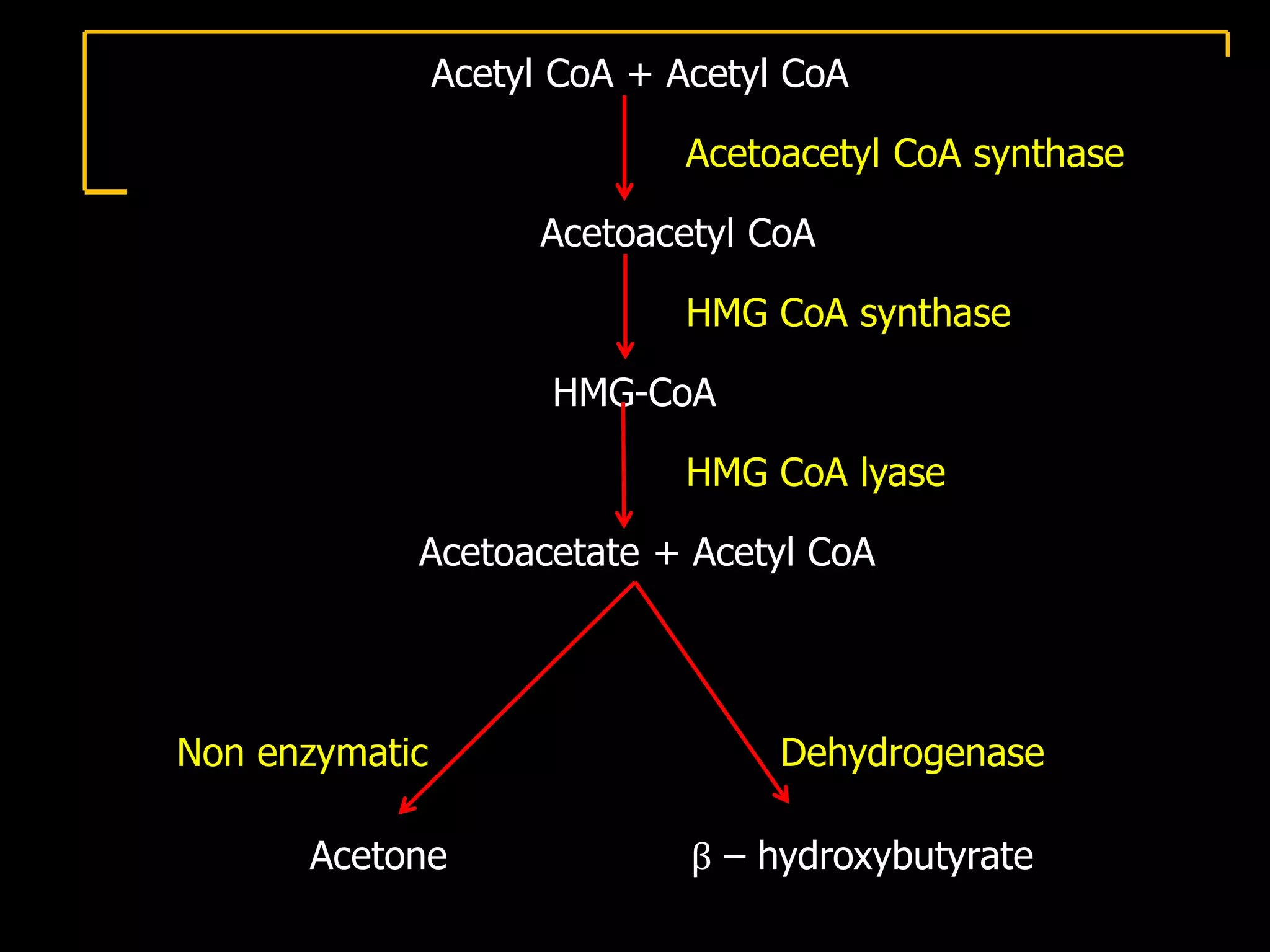
- Ketone bodies are produced when fats are broken down in the liver and include acetone, acetoacetate, and beta-hydroxybutyrate.
- Ketone bodies can be used as an energy source by tissues and can cross the blood brain barrier.
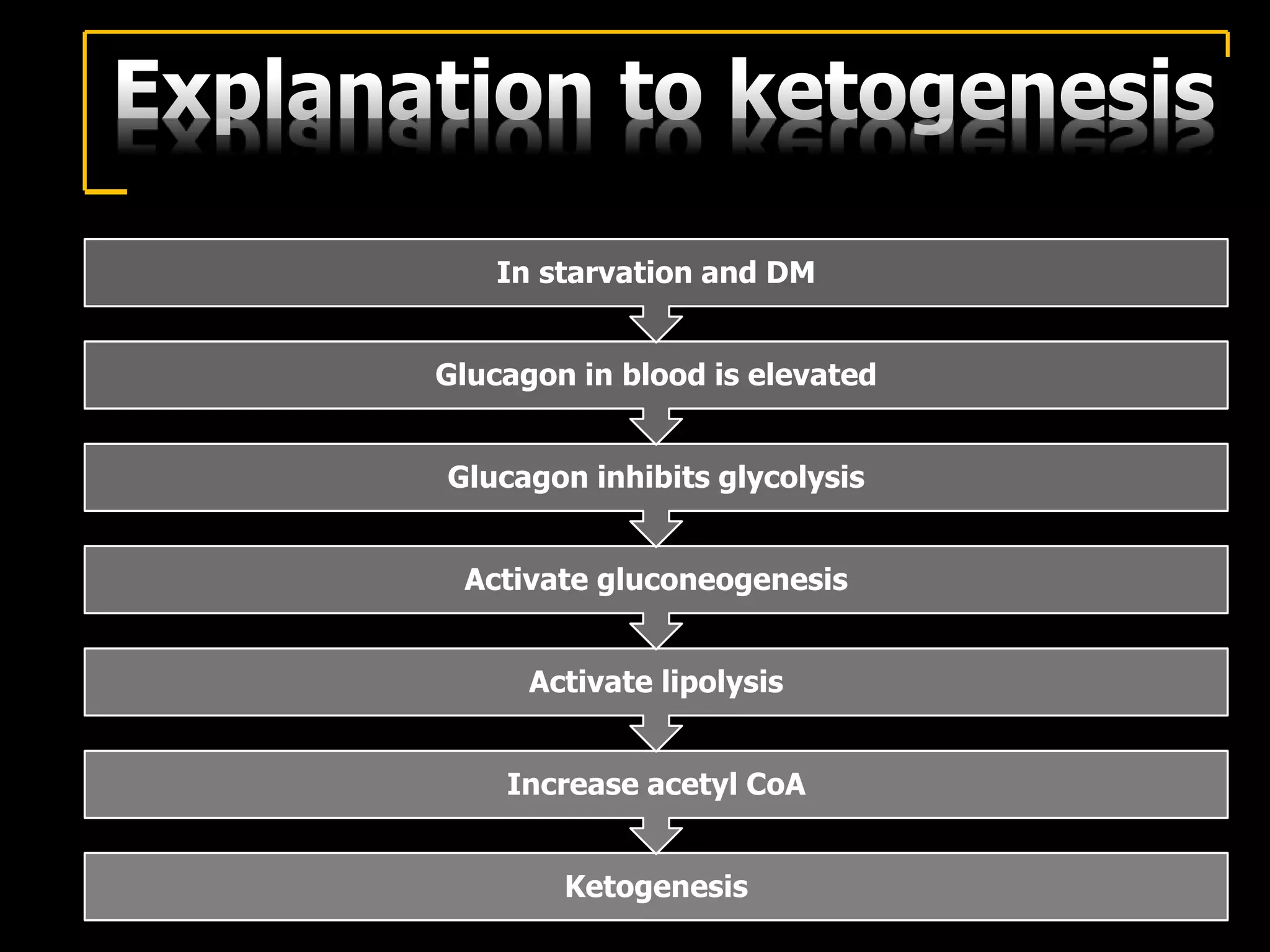
- Ketogenesis occurs in the liver mitochondria when glucose levels are low, such as during starvation or untreated diabetes. This allows fatty acids to be broken down into ketone bodies.
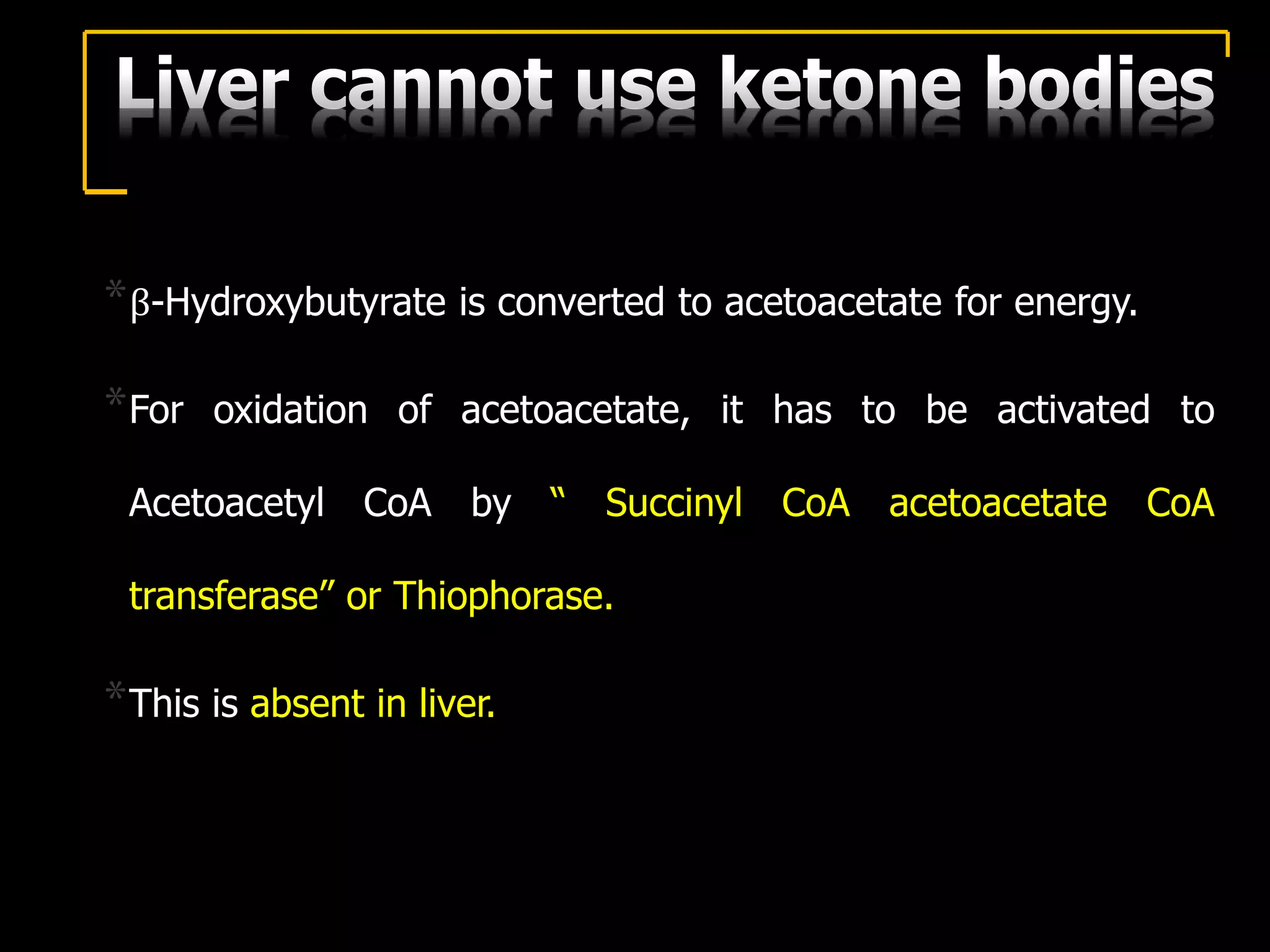
- Ketolysis is the breakdown of ketone bodies which occurs in extrahepatic tissues to produce acetyl CoA for energy production.