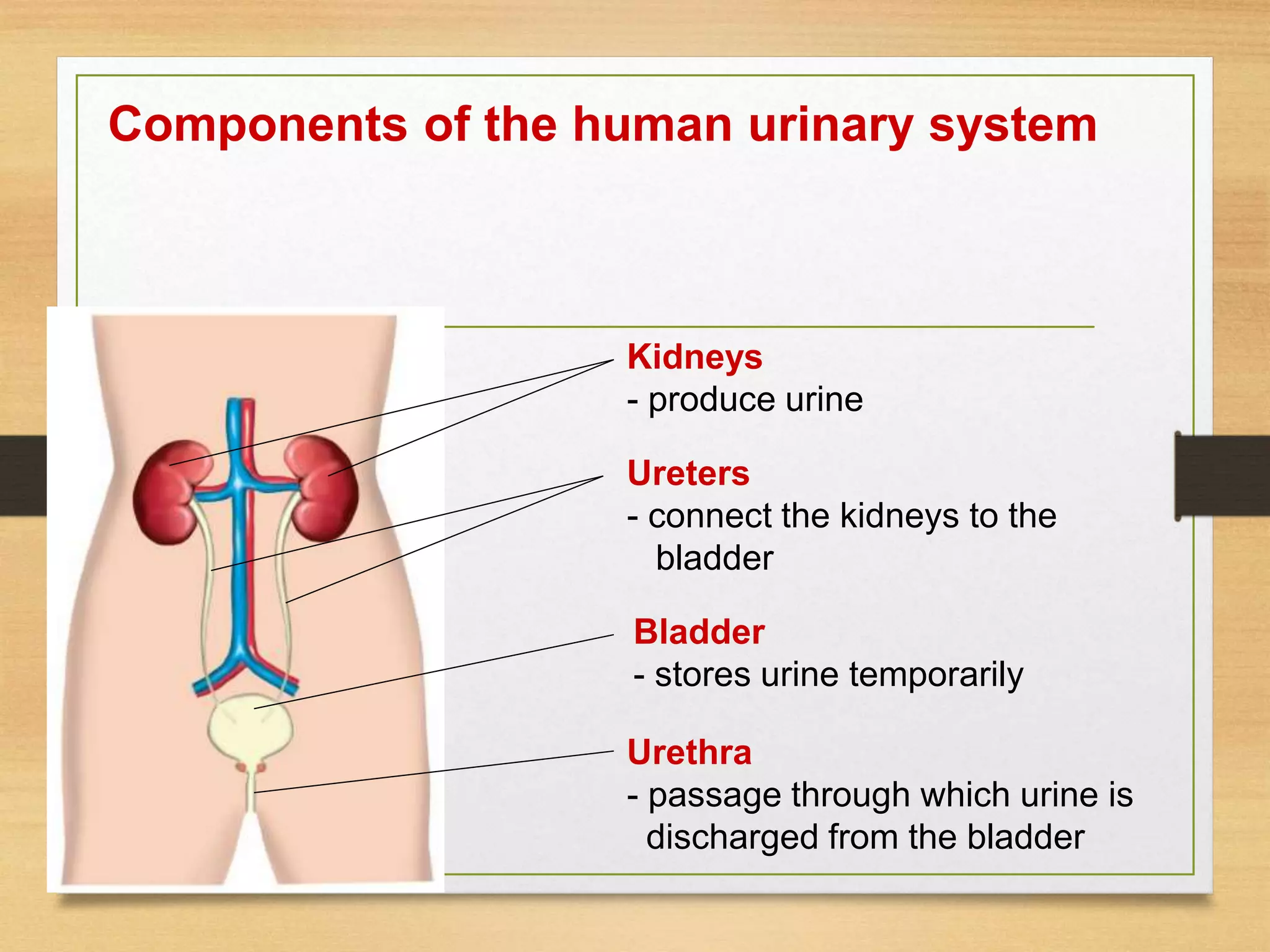
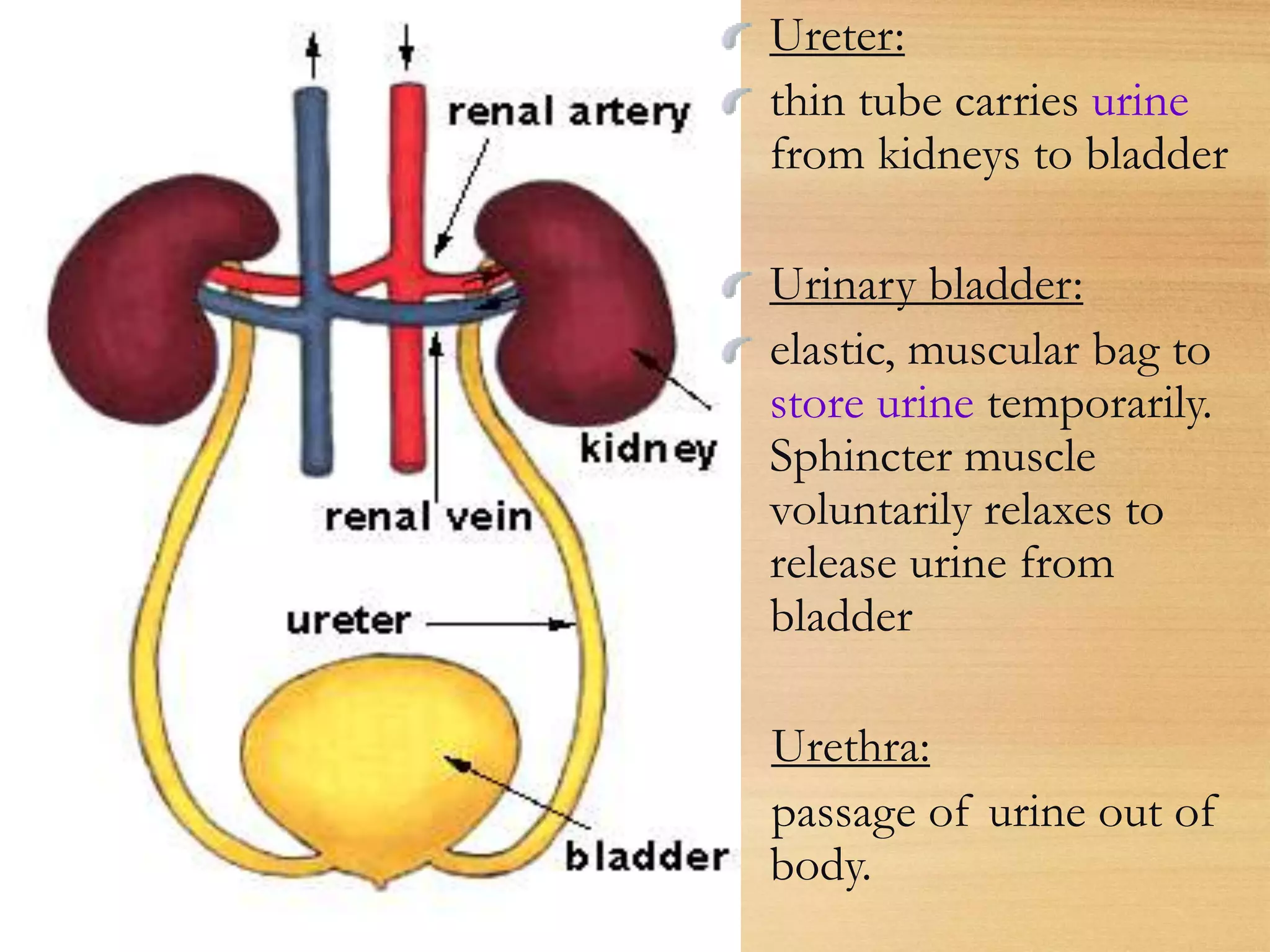
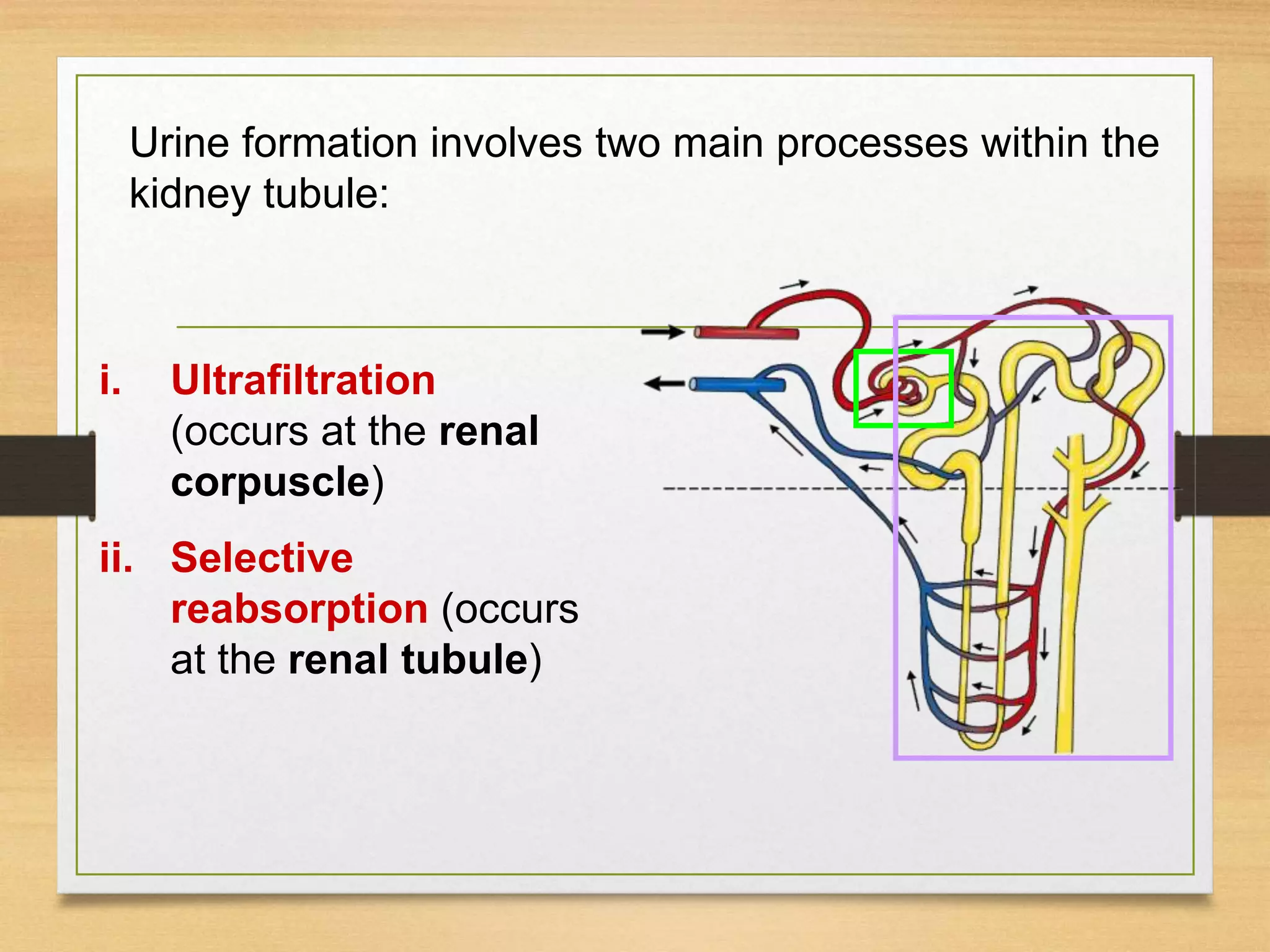
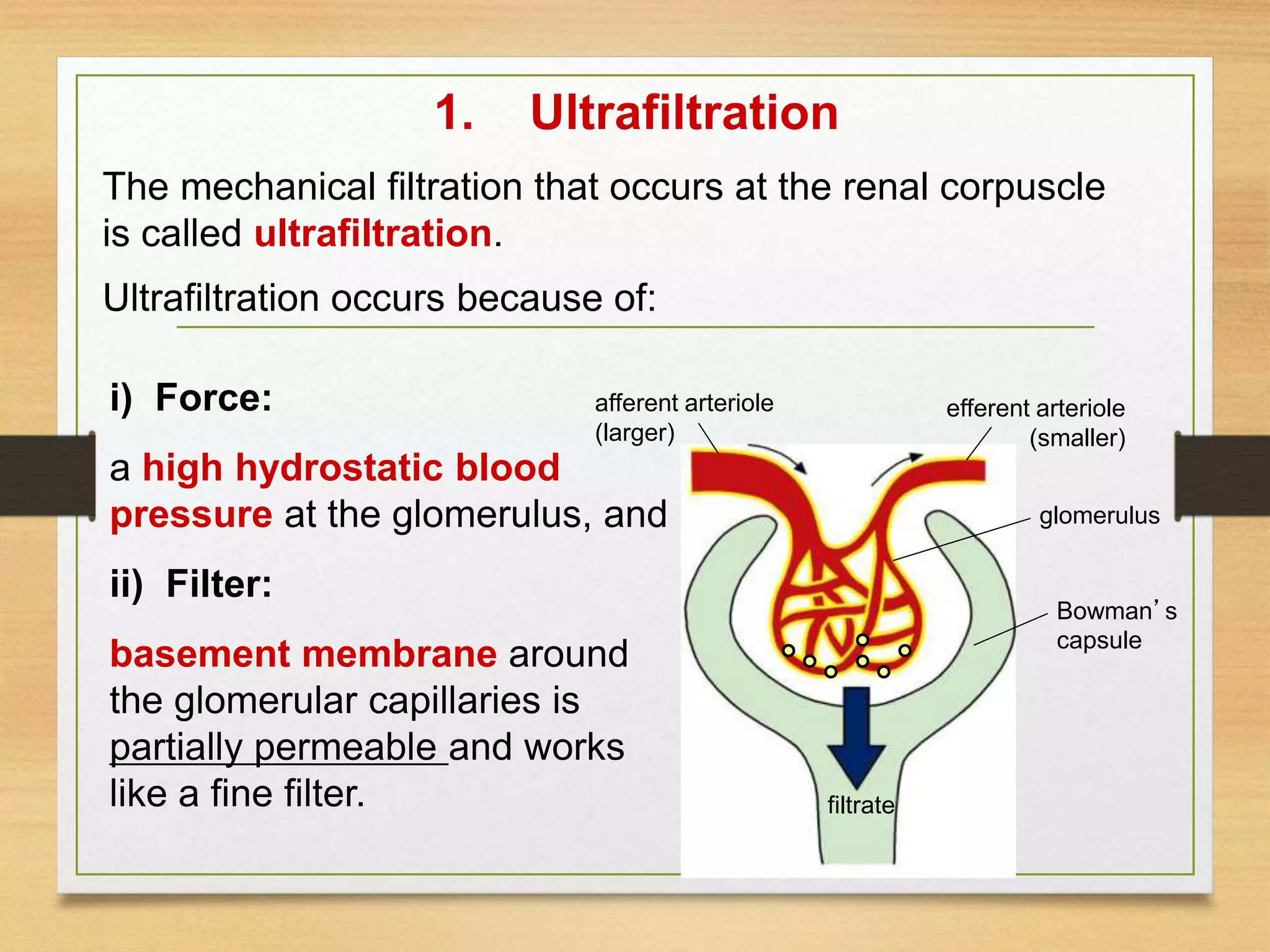
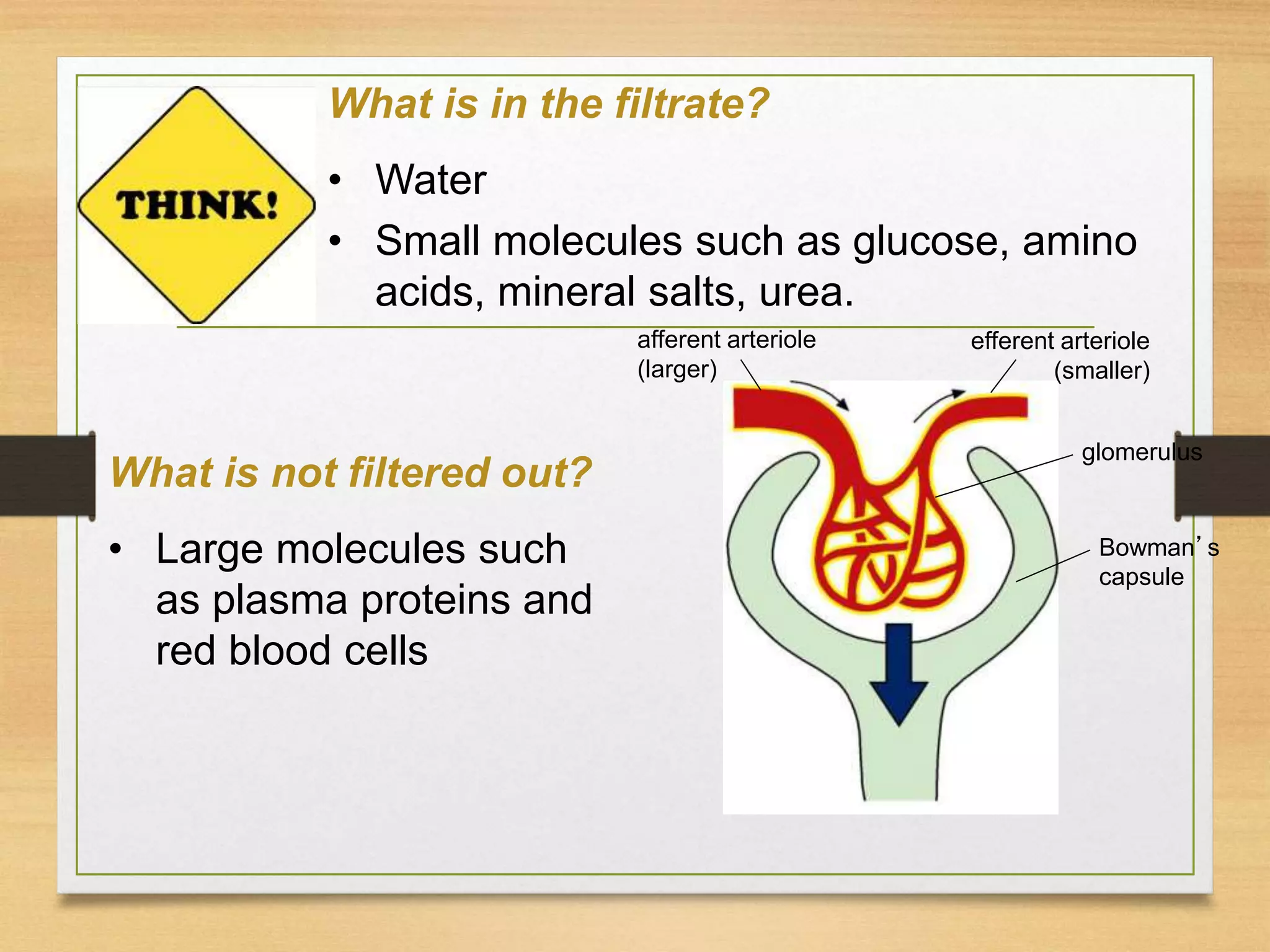
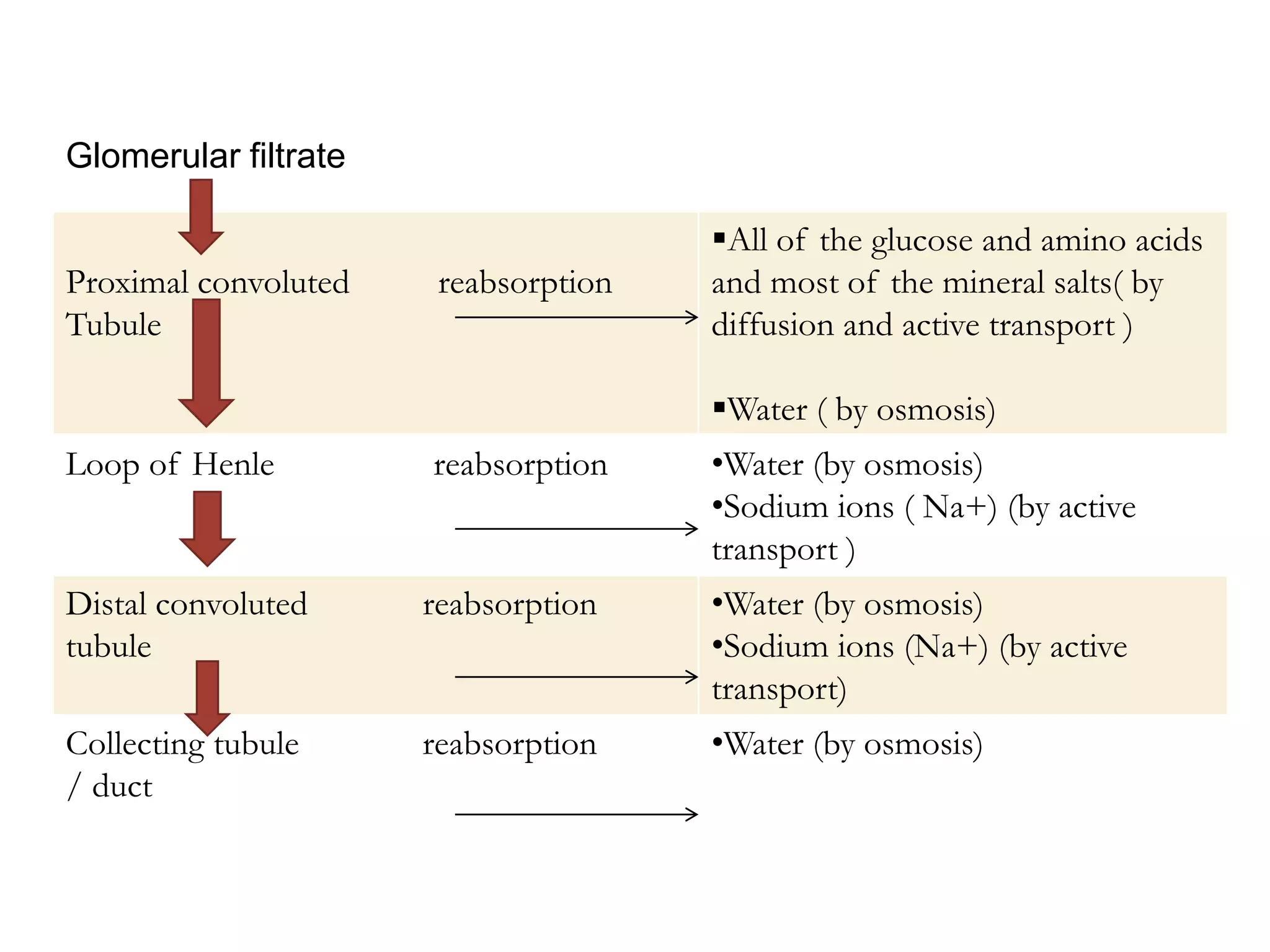
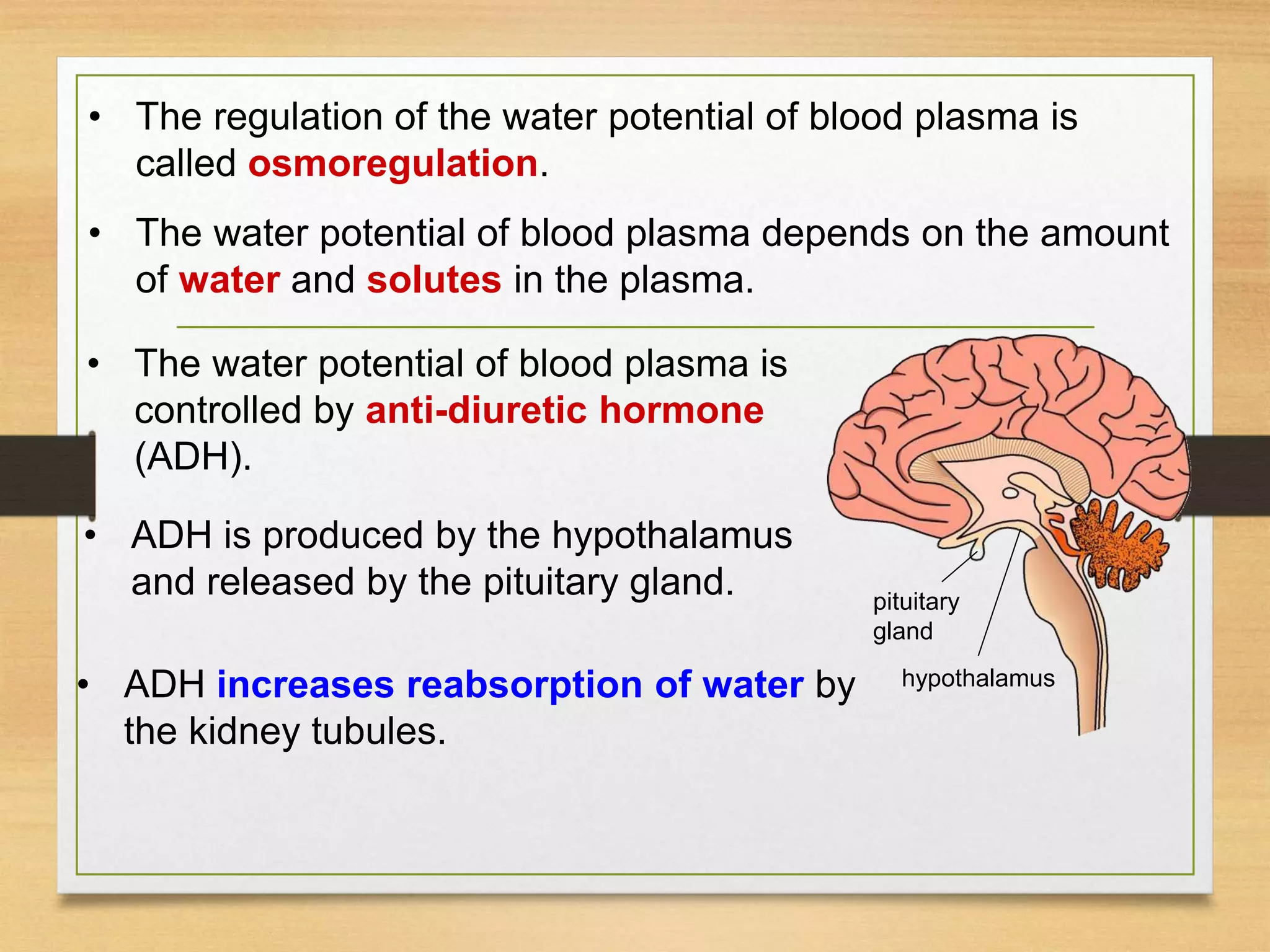
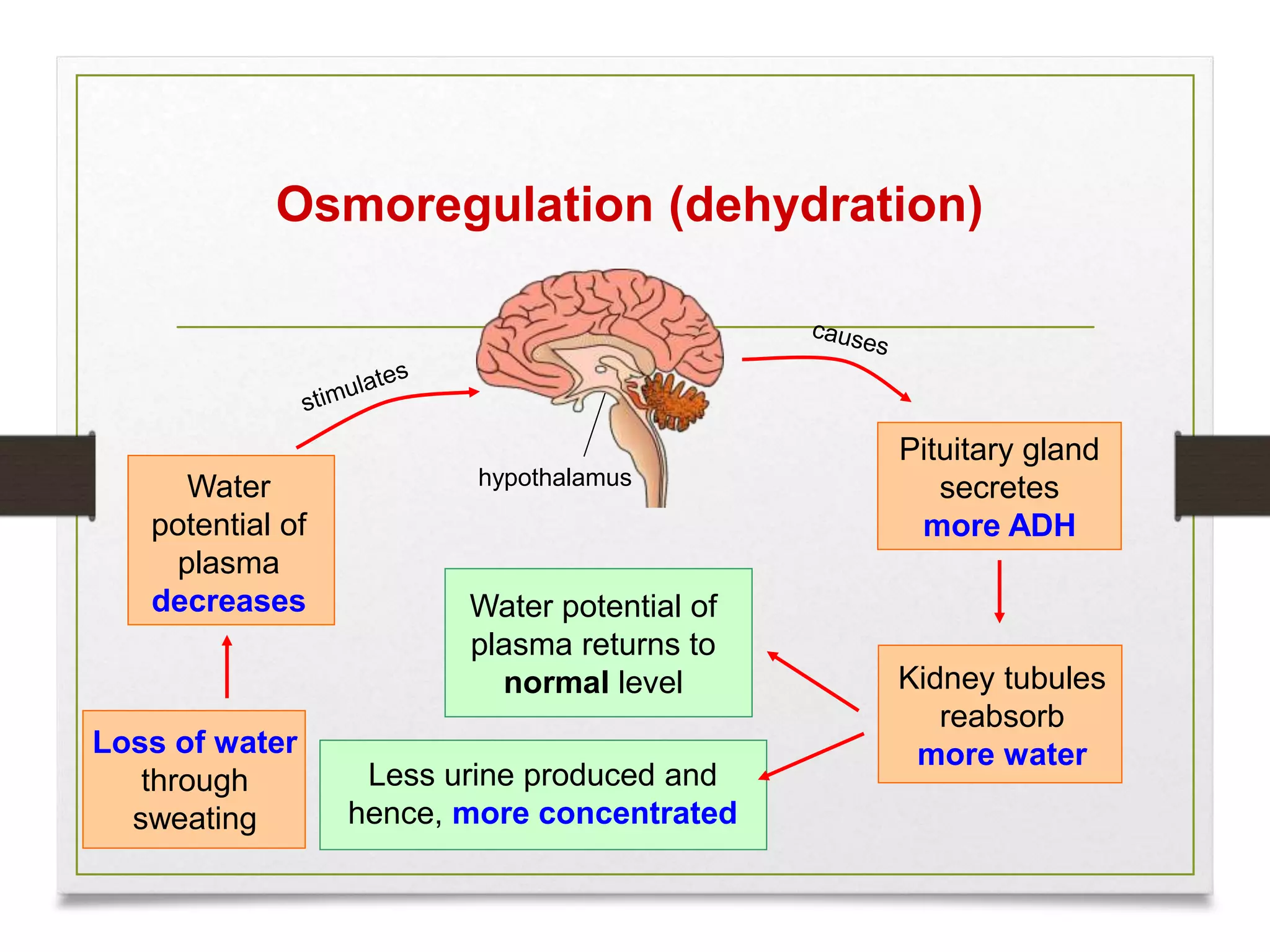
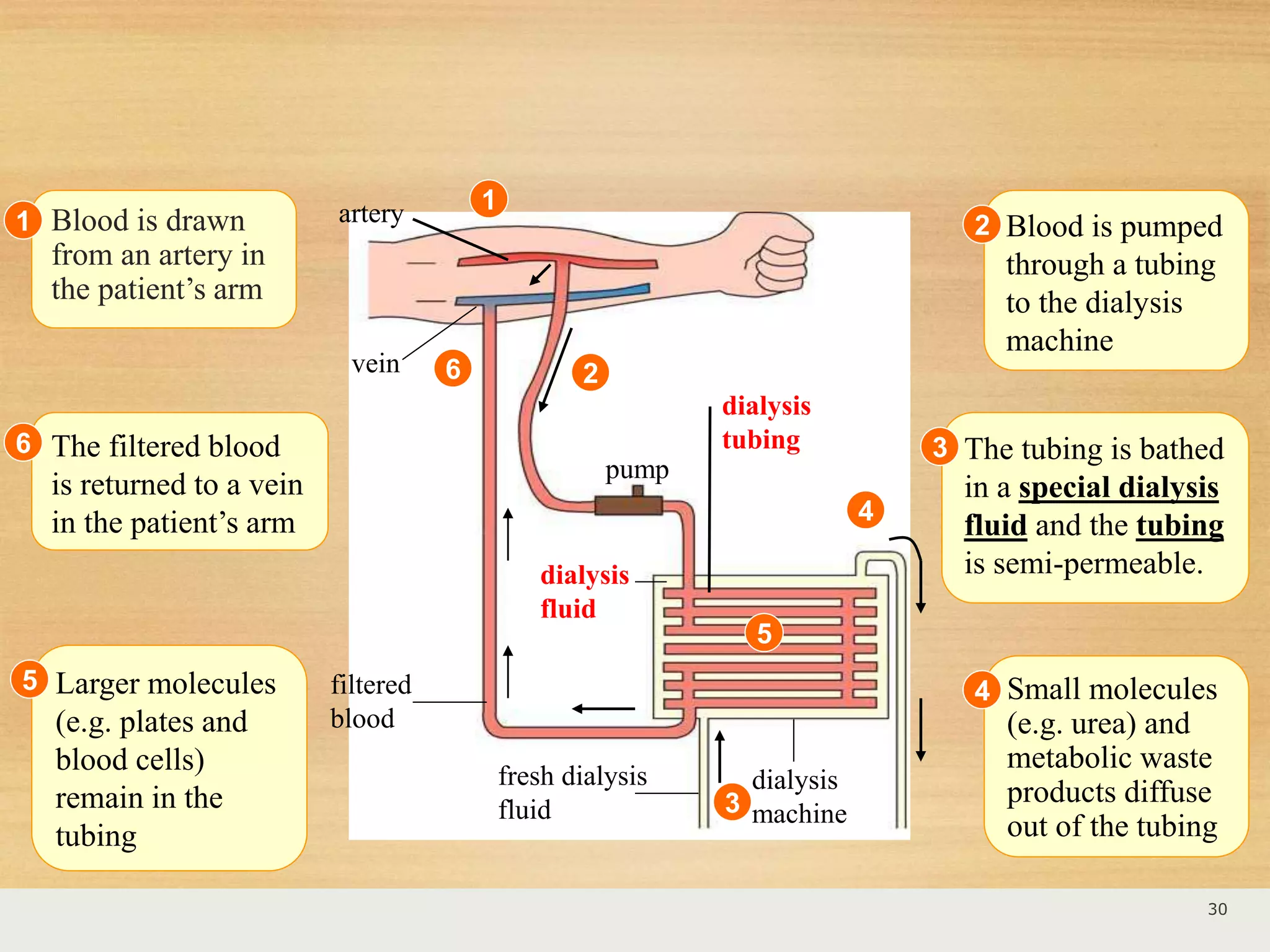
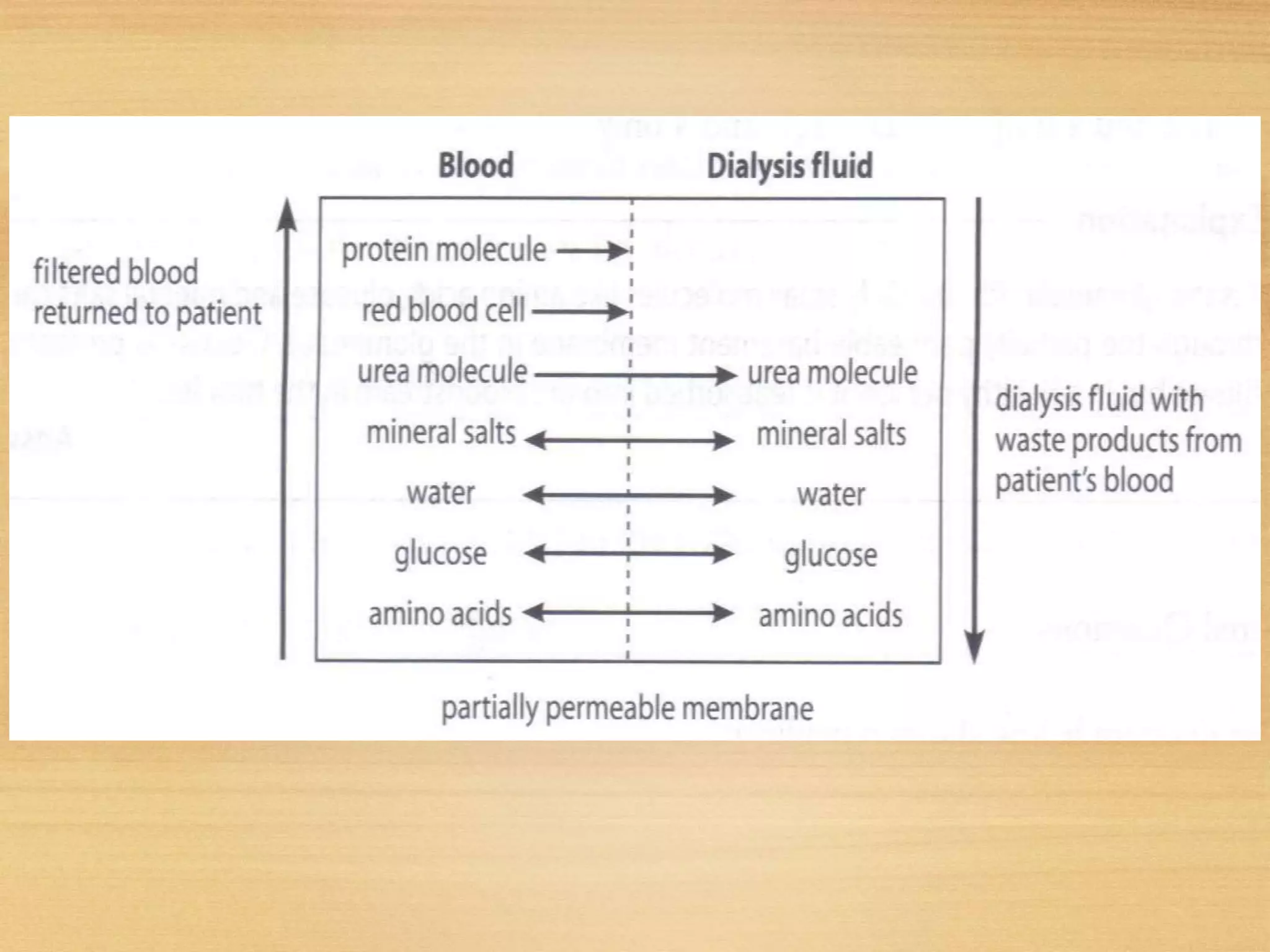
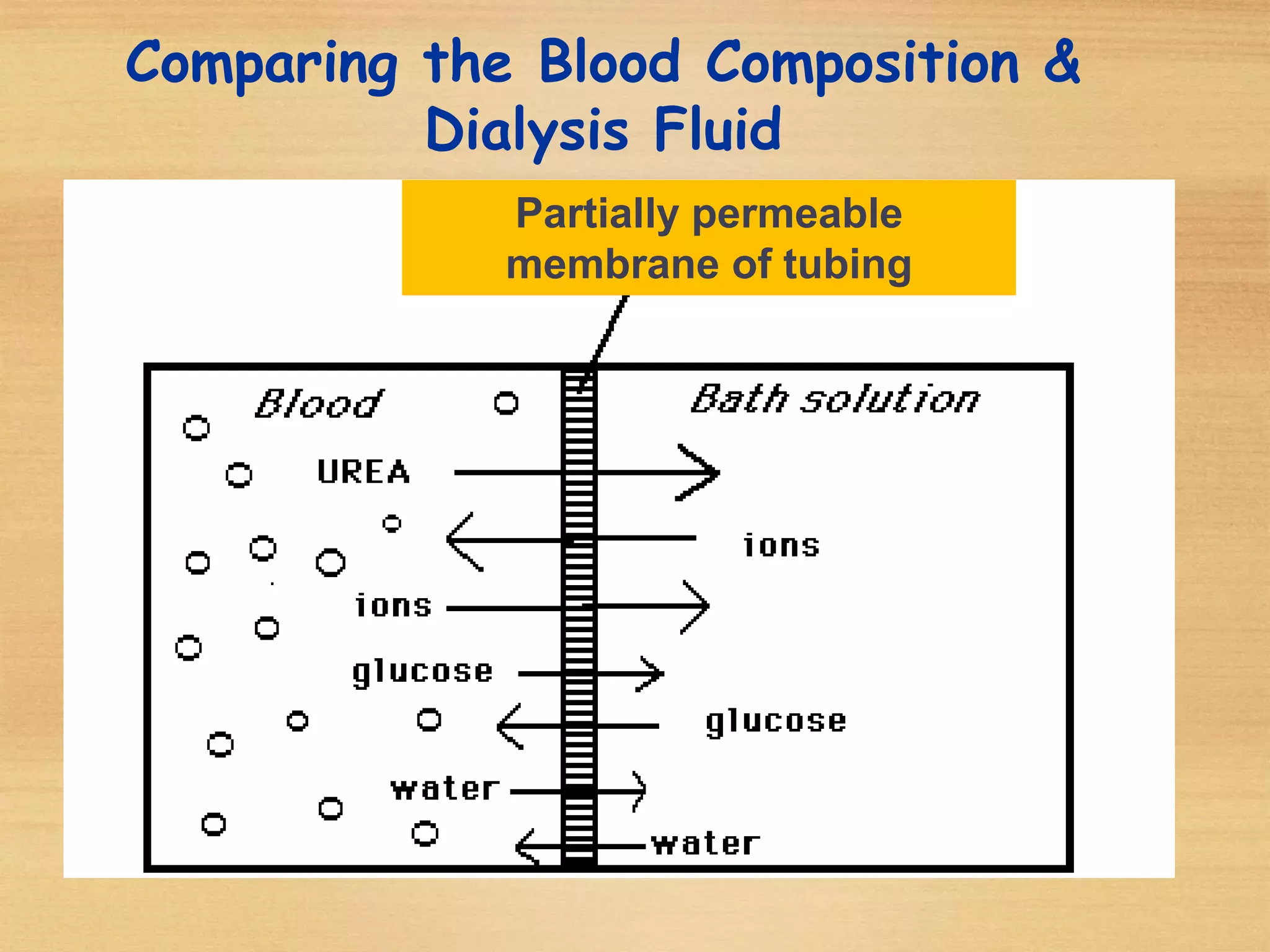
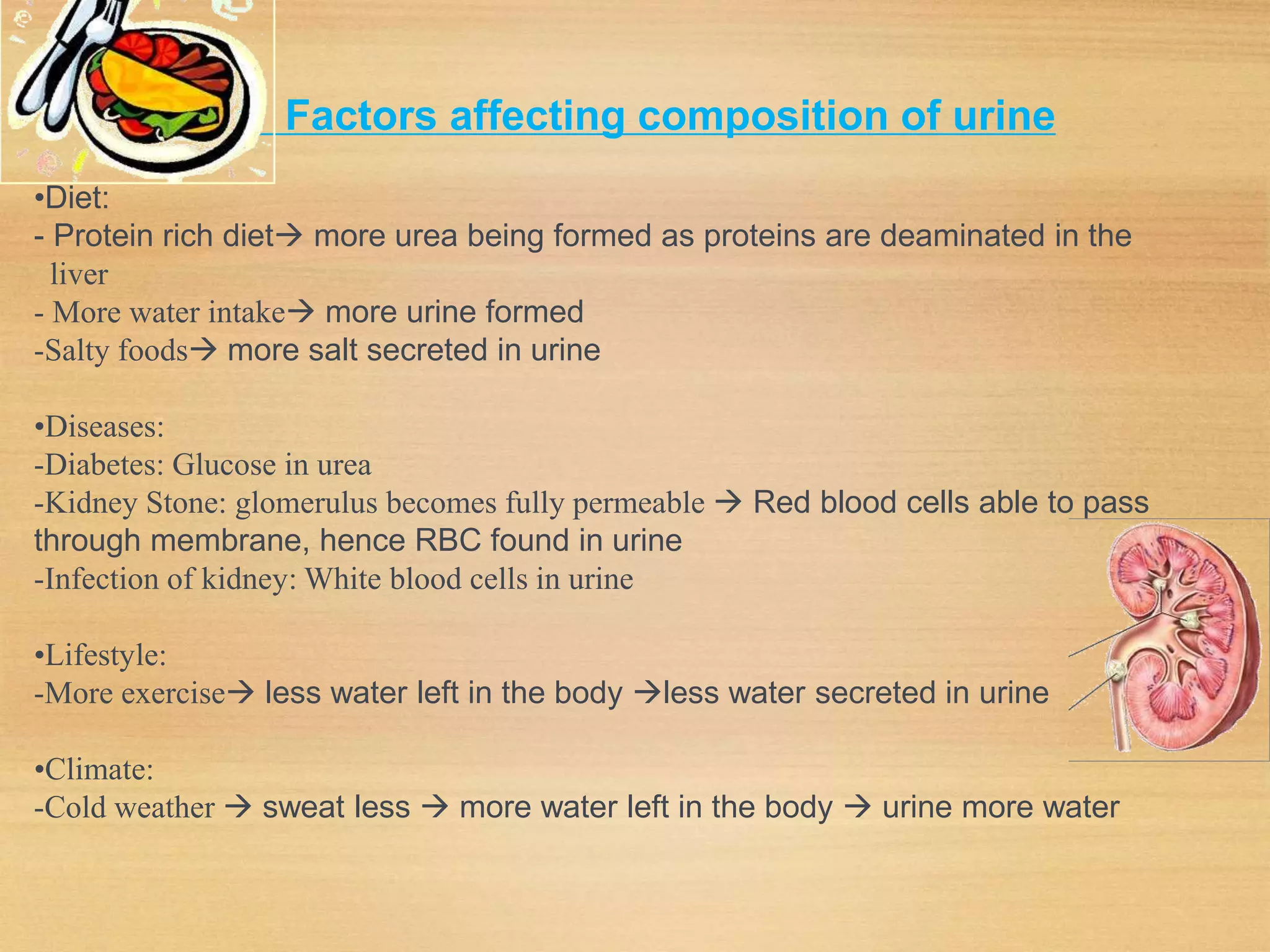
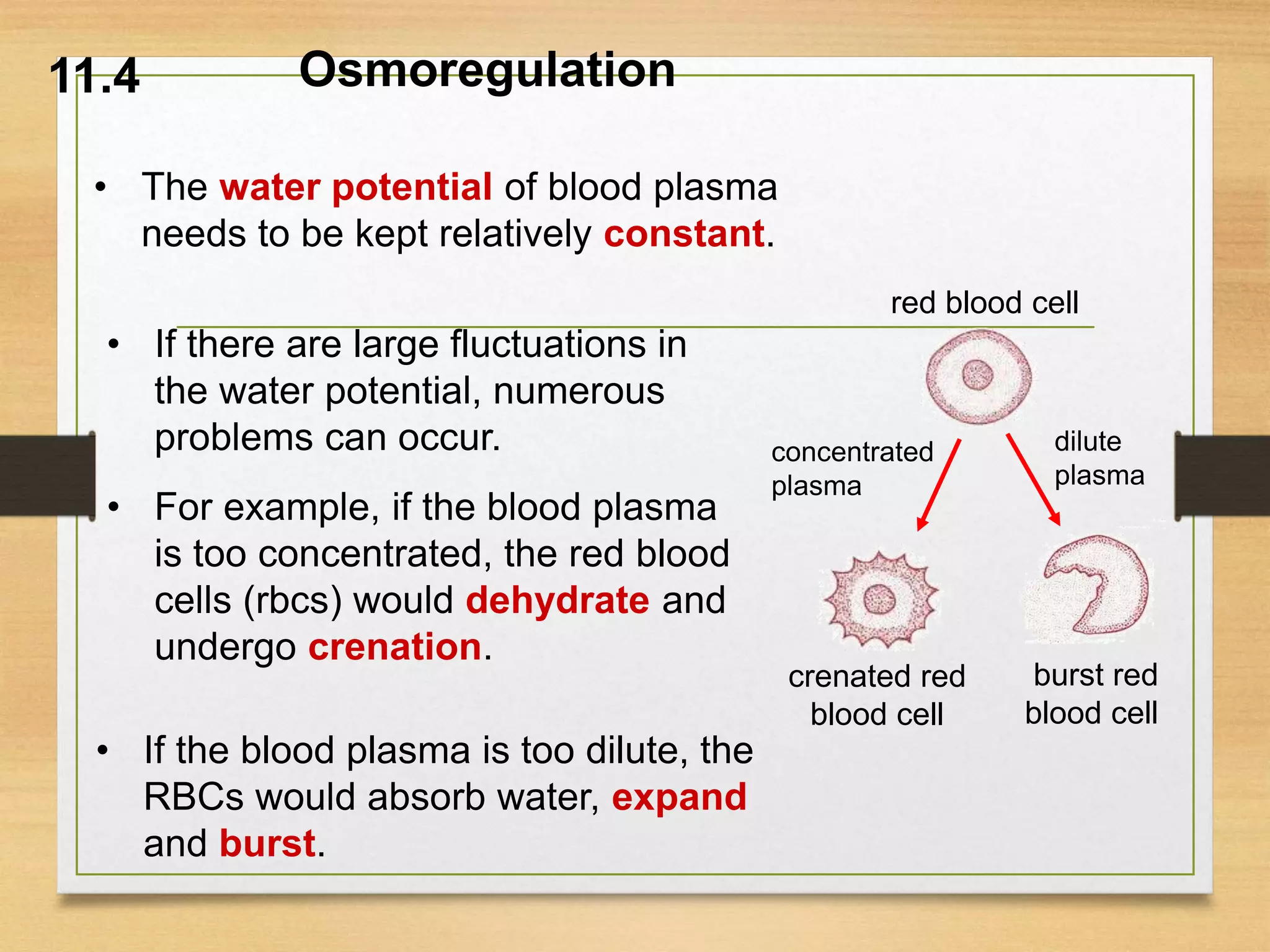
The document summarizes key concepts about excretion and the urinary system. It discusses (1) how the kidneys produce urine through ultrafiltration and selective reabsorption, (2) how anti-diuretic hormone regulates water concentration in the blood through urine production, and (3) how dialysis can remove waste when the kidneys fail by diffusion across a semi-permeable membrane.