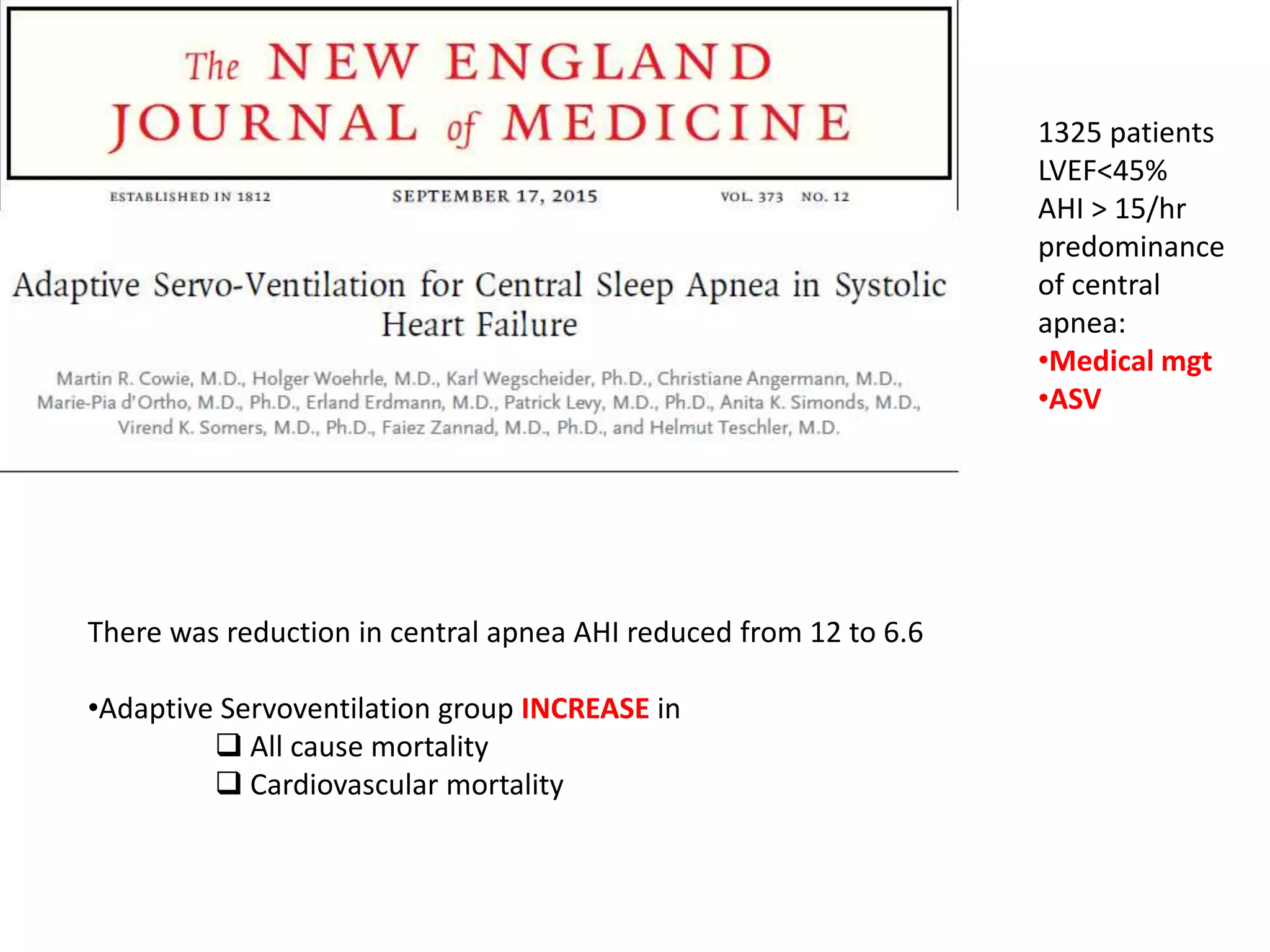
Titration is important to determine the optimal pressure for positive airway pressure (PAP) therapy. Manual titration involves starting at 4 cm for CPAP and gradually increasing pressure until apneas, hypopneas, and snoring are abolished. If high pressure is required or hypoxia occurs, bilevel PAP may be better. Oxygen can be added if needed to target SpO2 of 92-94%. The goal is an optimal or good titration with minimal events and arousals at a pressure the patient can tolerate. Common issues include mask leaks, discomfort, and congestion which may require pressure adjustment or changing the interface.