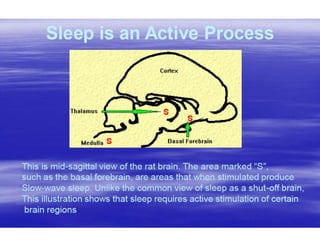
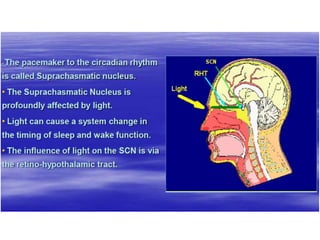
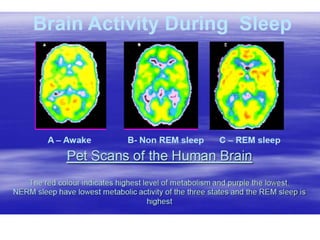
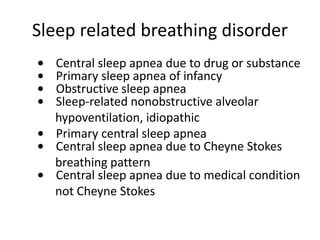
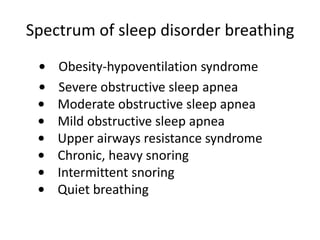
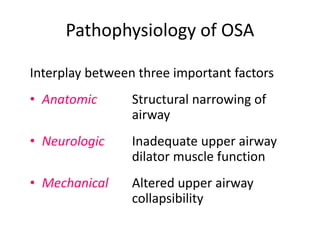
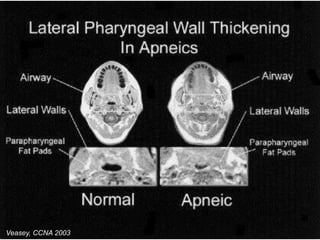
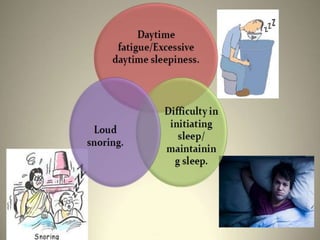
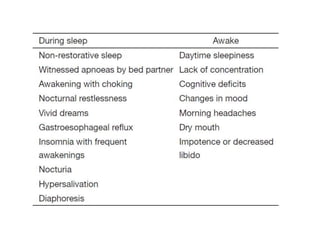
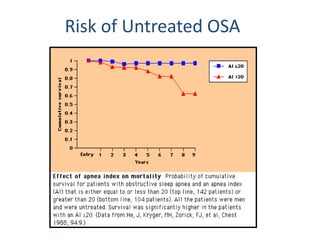
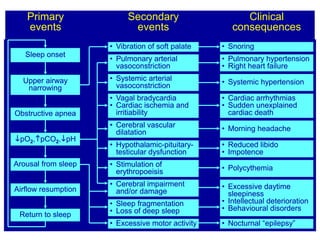
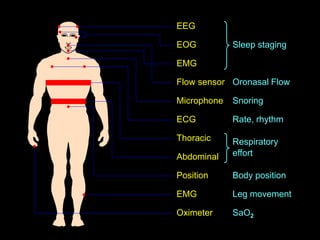
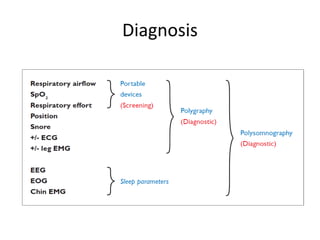
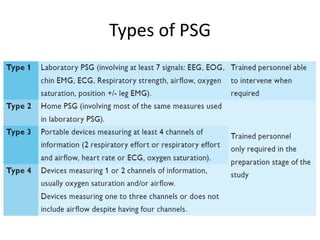
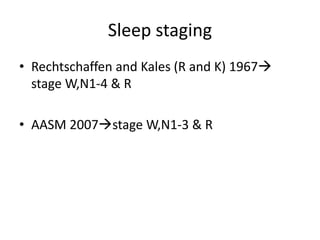
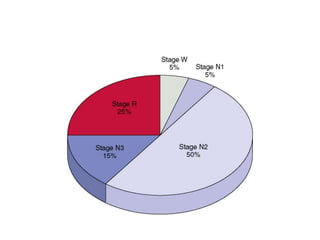
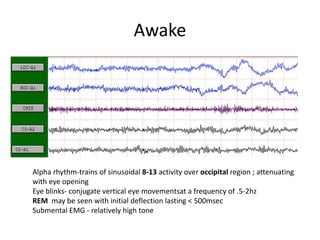
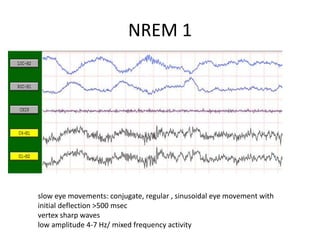
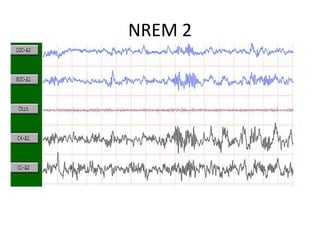
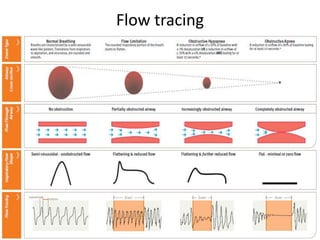
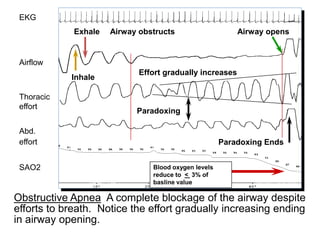
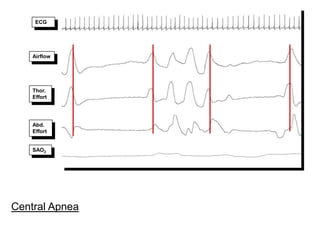
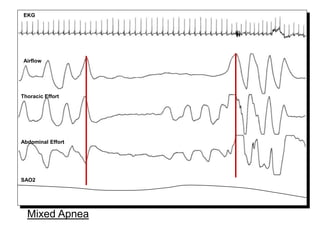
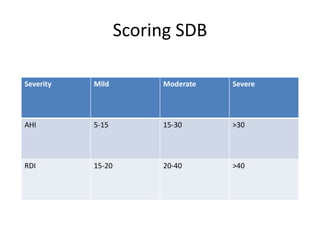
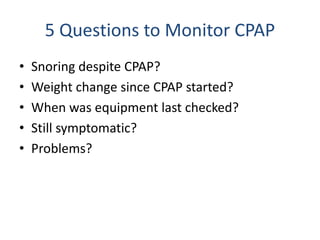
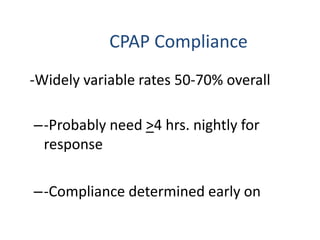
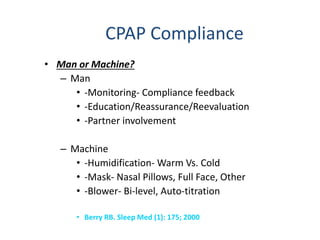
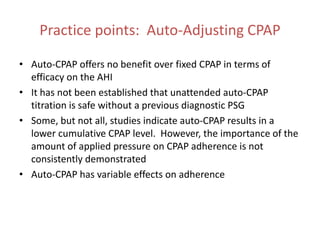
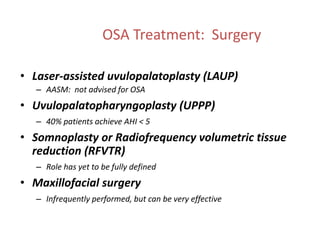
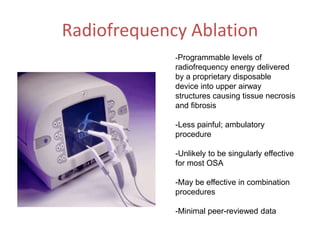
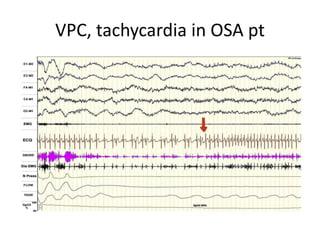
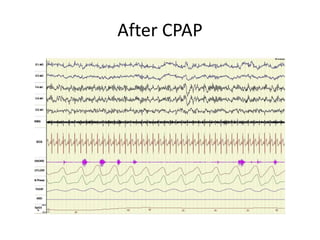
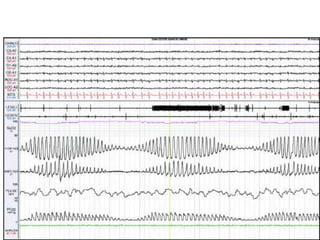
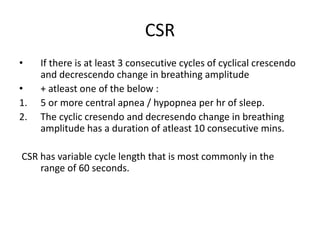
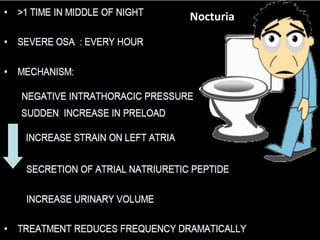
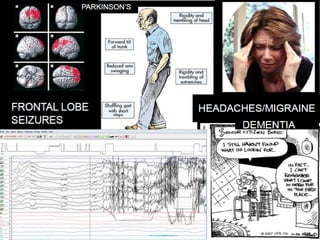
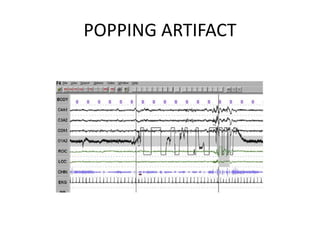
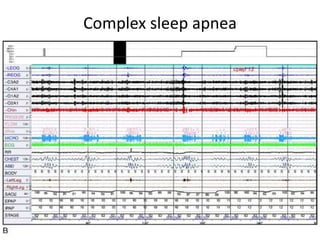
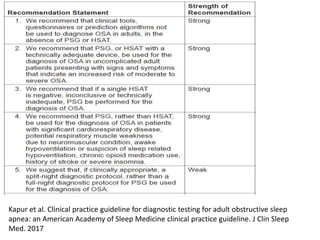
This document provides an overview of sleep disorders including sleep related breathing disorders, movement disorders, insomnias, parasomnias, hypersomnias, and circadian rhythm disorders. It discusses obstructive sleep apnea (OSA) in detail including its pathophysiology, risks of untreated OSA, diagnostic polysomnography, and treatment options like CPAP and surgery. It also covers some pitfalls in diagnosing and treating sleep disorders and highlights the importance of considering sleep-related issues in other medical specialties.