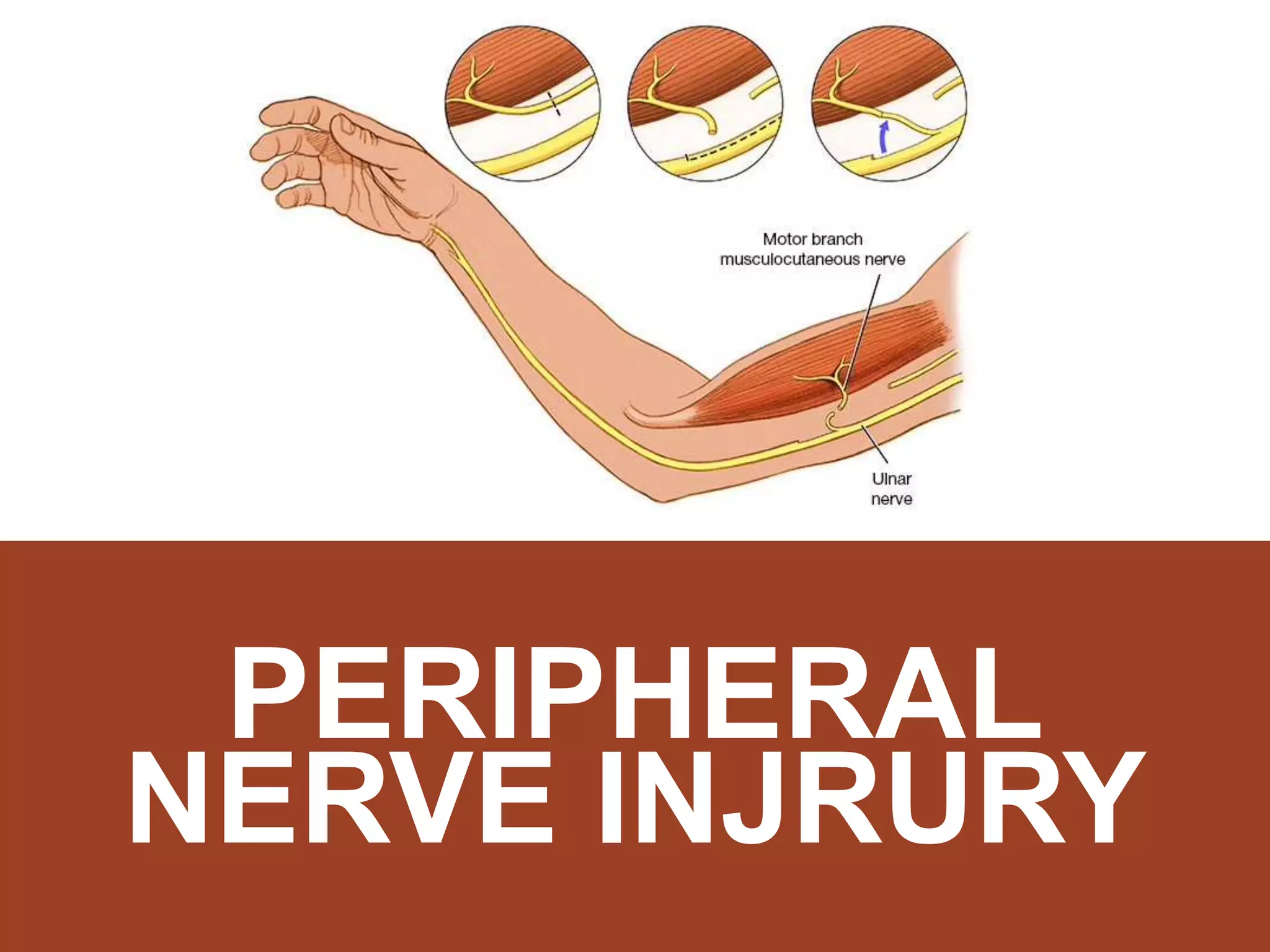
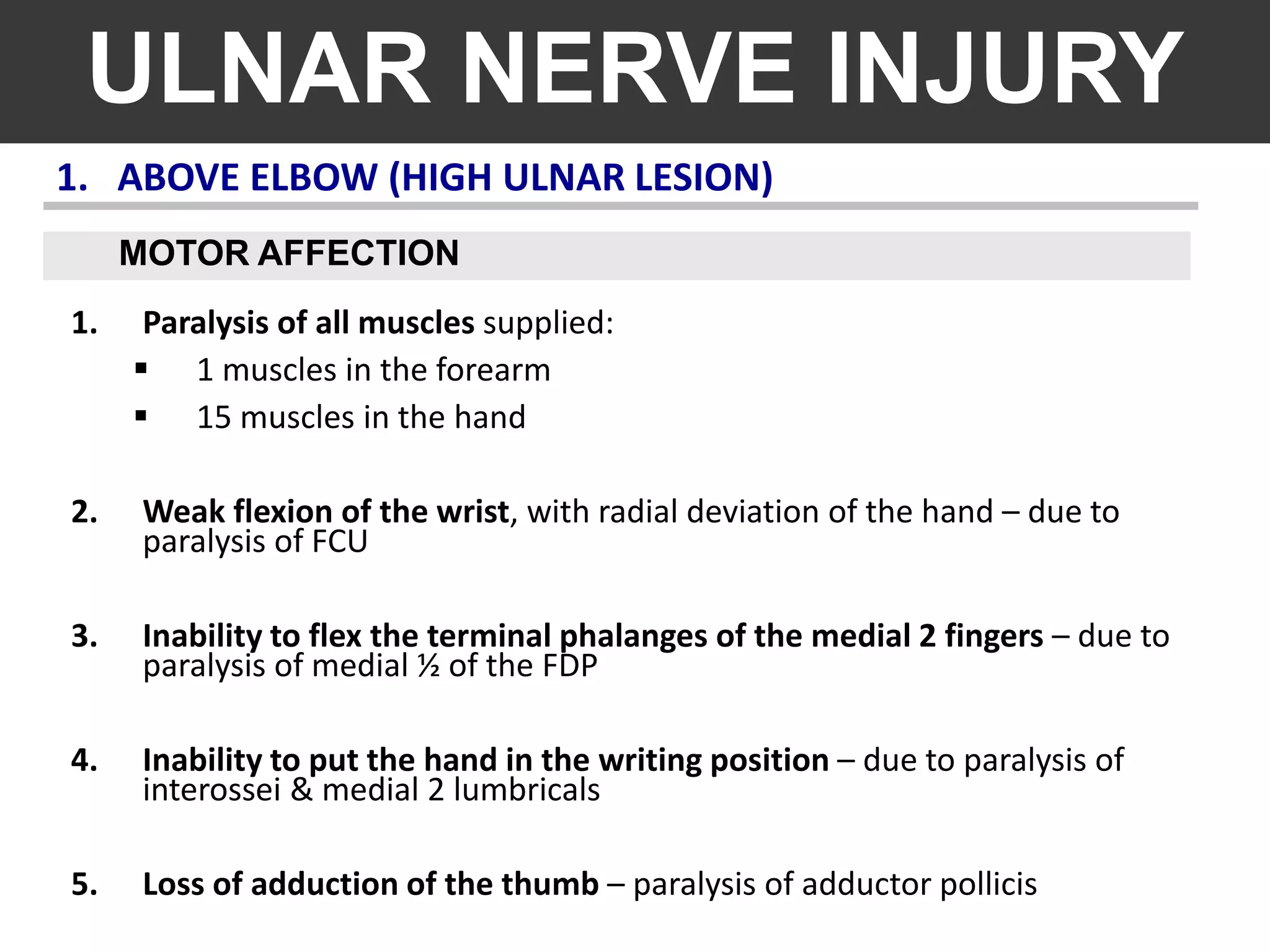
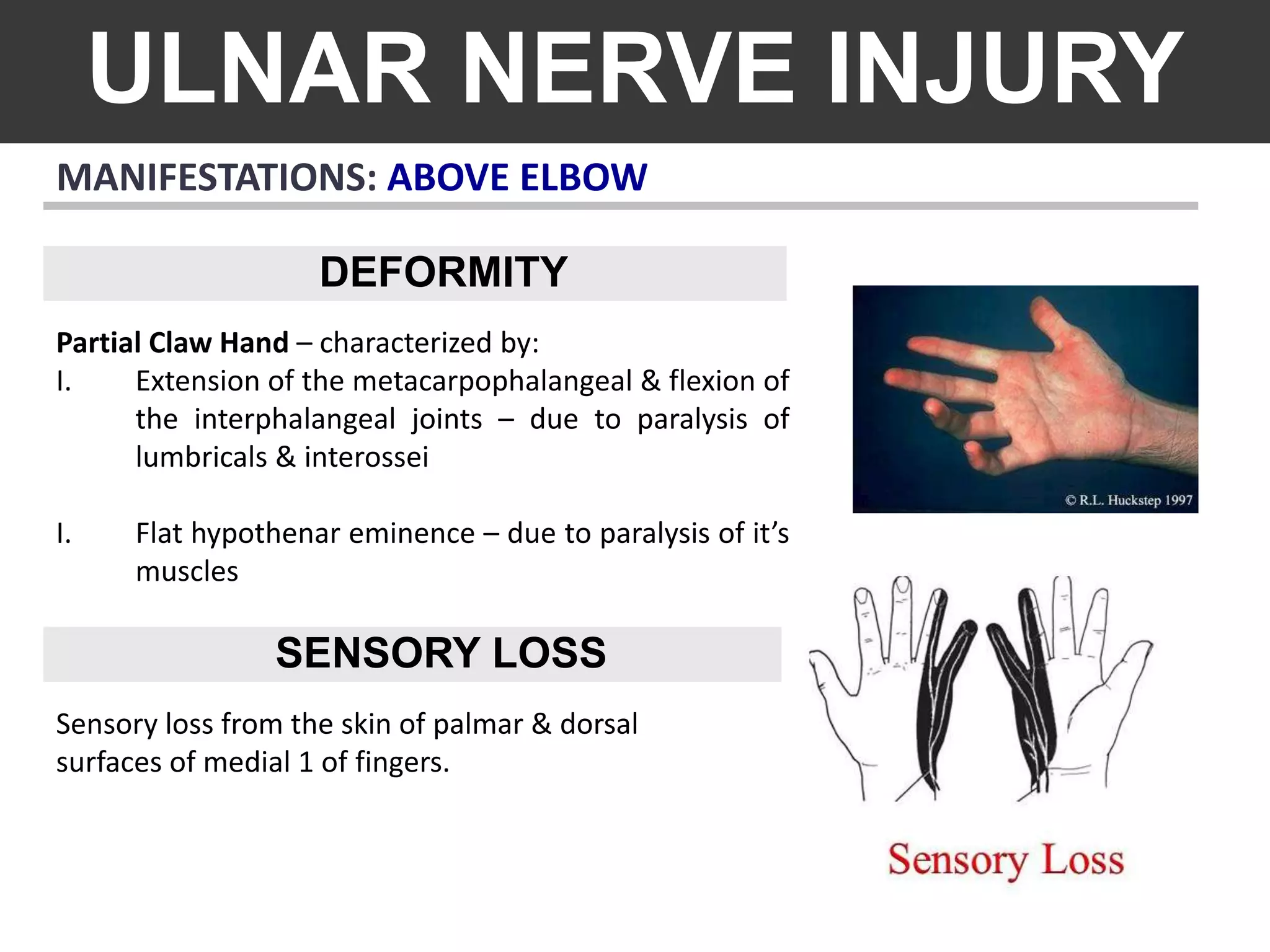
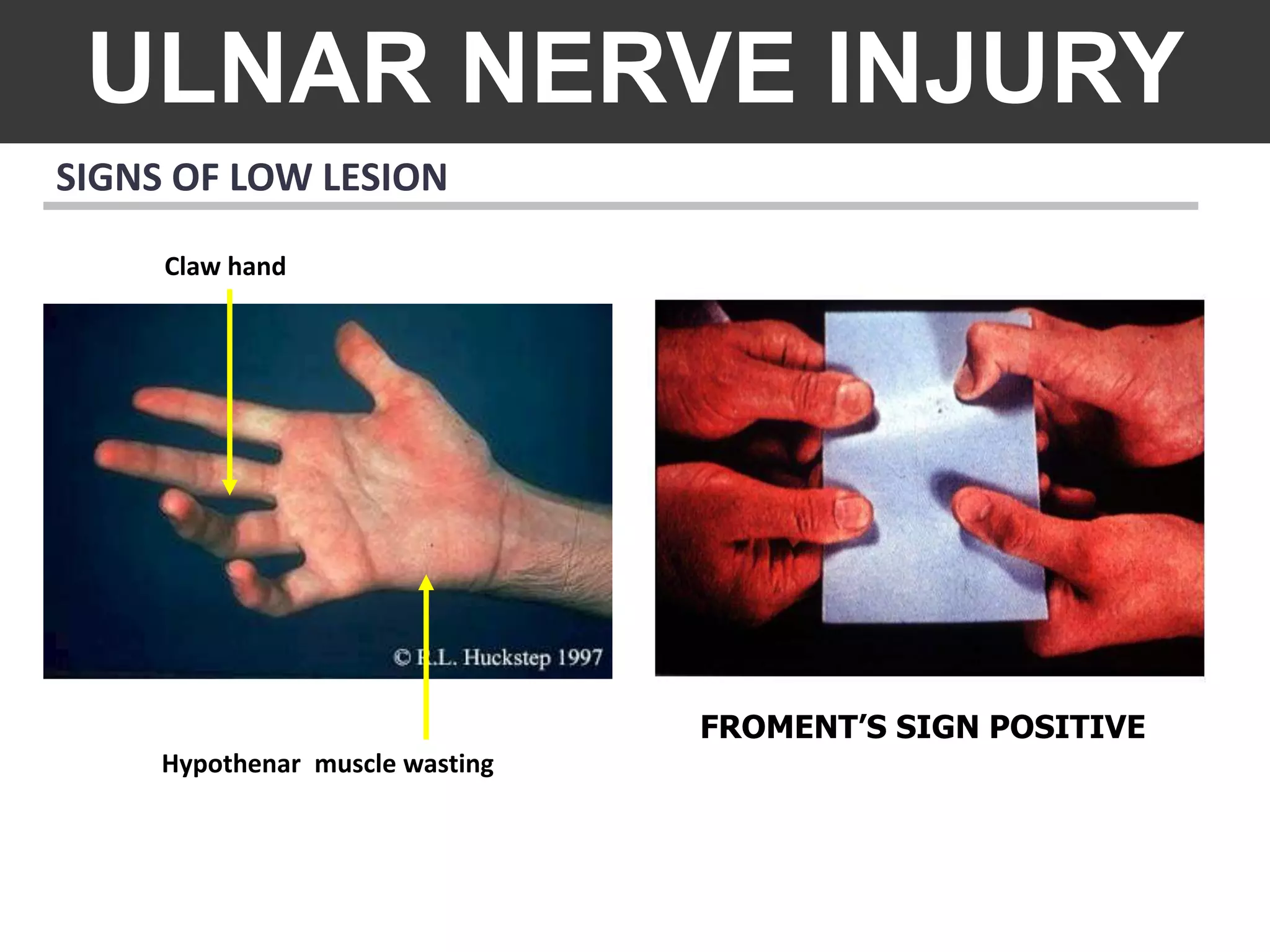
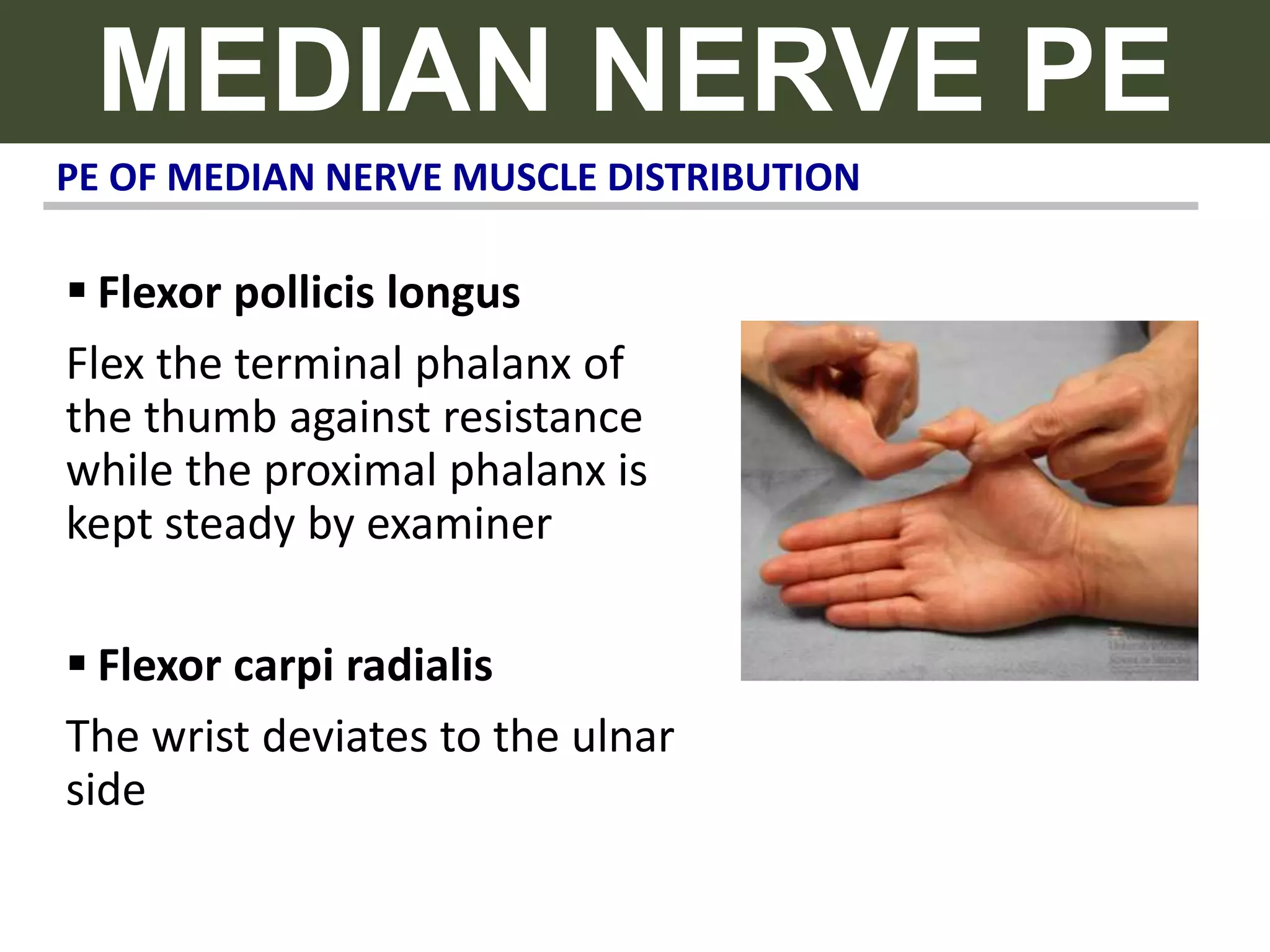
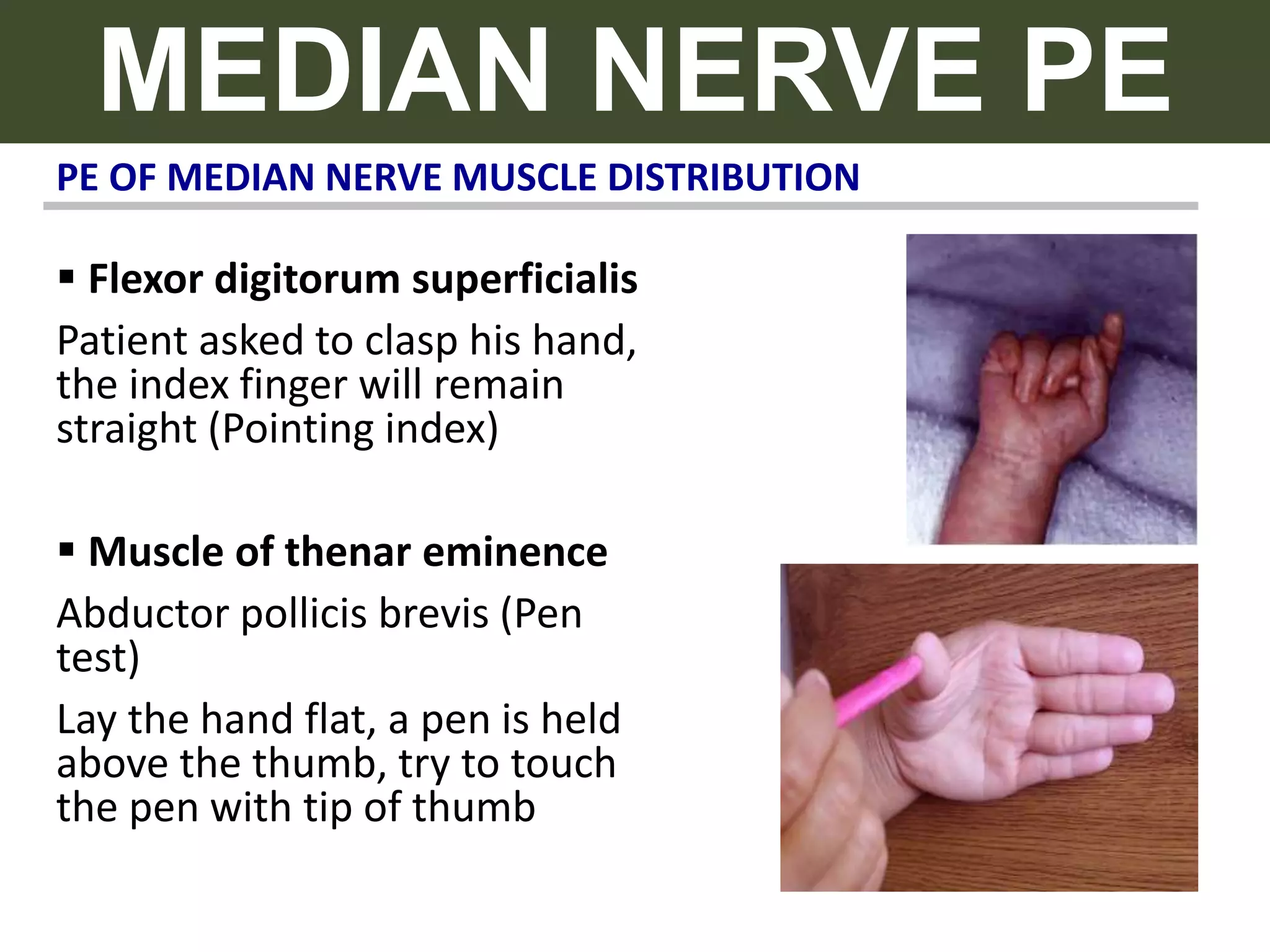
The document provides an extensive overview of various ulnar, median, radial, and tibial nerve injuries, including their classification, anatomy, symptoms, and treatment options. It details specific conditions like cubital tunnel syndrome, carpal tunnel syndrome, and others, explaining motor and sensory impairments associated with different lesions. Treatment strategies range from conservative measures like physiotherapy and splints to surgical interventions for nerve repair.