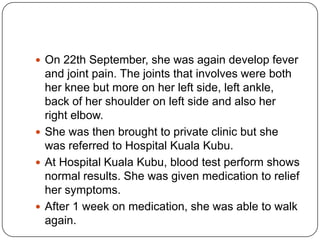
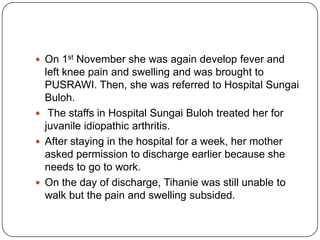
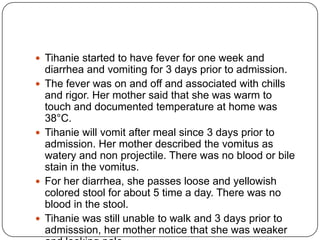
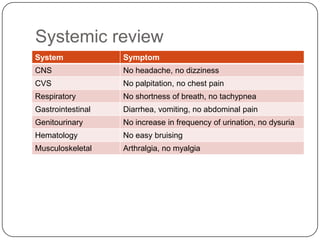
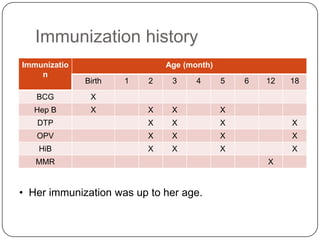
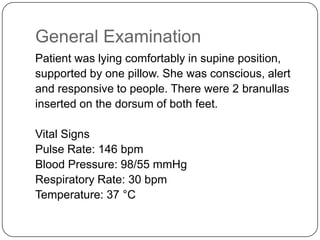
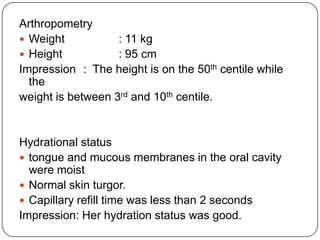
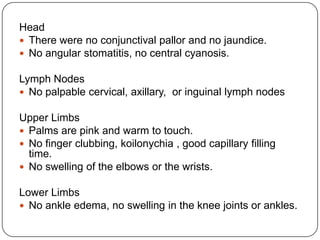
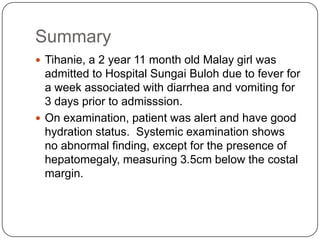
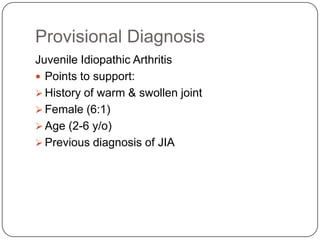
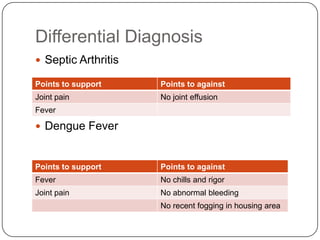
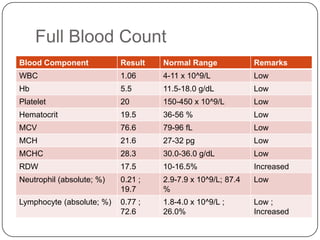
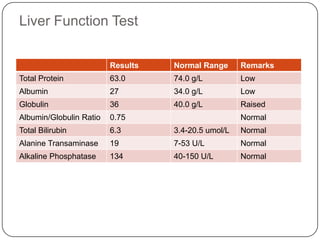
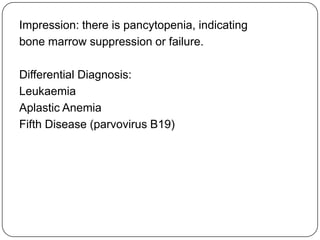
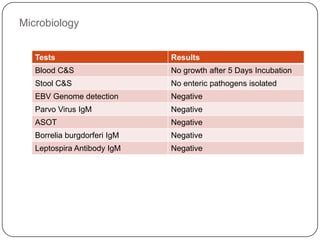
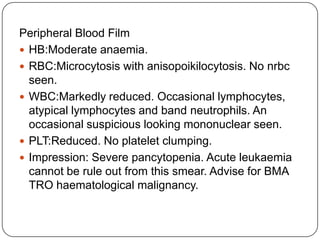
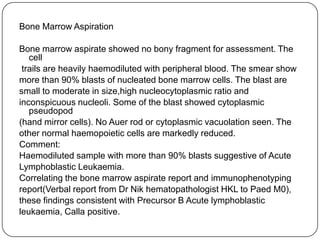
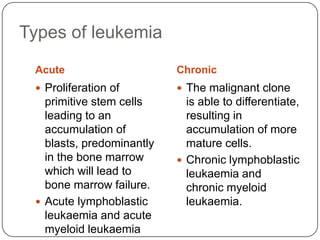
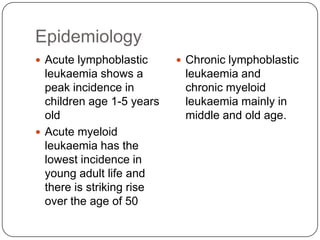
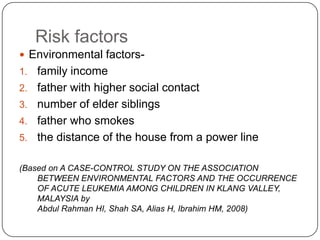
Rose KhadeejaTihanie, a 2 year 11 month old girl, was admitted with fever, diarrhea and vomiting. Examination found hepatomegaly but was otherwise normal. Investigations showed pancytopenia. Bone marrow aspiration found over 90% blasts consistent with acute lymphoblastic leukemia. She was diagnosed with juvenile arthritis secondary to ALL. ALL has a peak incidence in young children and risks include genetic and environmental factors. Clinical features include infections, pallor and organomegaly. Management aims to induce remission through chemotherapy while preventing complications like infections. Prognosis depends on factors like age and white cell count.