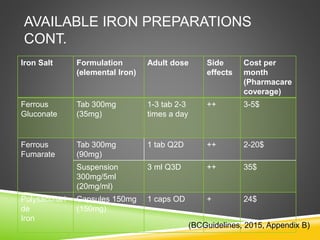
Ms. T is a 38-year-old woman who presents with a 6-month history of heavy menstrual bleeding and fatigue. Her lab results show low hemoglobin, ferritin, iron, MCV and MCH levels consistent with iron deficiency anemia. Her risk factors include female gender, past pregnancies, long-term NSAID use, and intermenstrual bleeding. She is started on iron supplements to replenish her iron stores, treat her anemia, and resolve her symptoms.