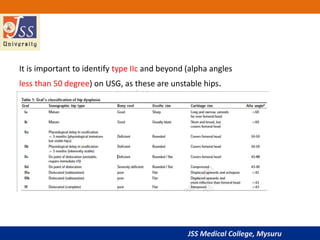
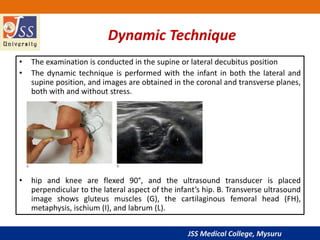
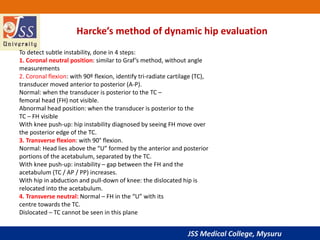
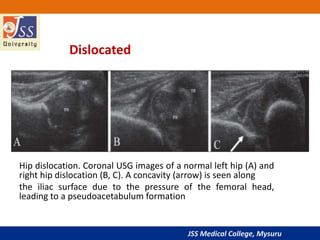
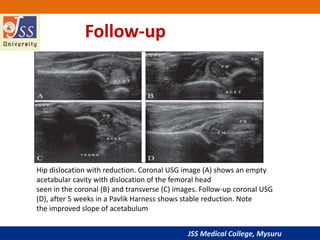
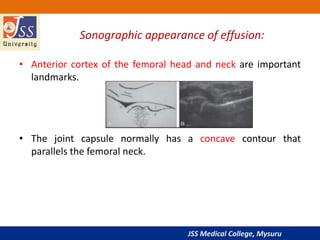
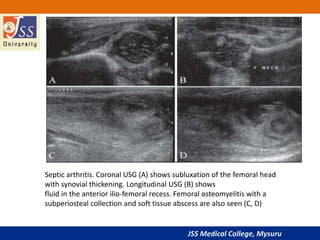
This document discusses using ultrasound to evaluate infant and child hips. It begins with an introduction on the history and effectiveness of hip ultrasound. It then covers developmental dysplasia of the hip, including risk factors, pathophysiology, and ultrasound examination techniques like Graf's method. The document discusses using ultrasound to detect hip effusions, subluxation, dislocation and monitor treatment. It emphasizes ultrasound is very accurate for detecting developmental dysplasia of the hip in infants under 1 year old.

![JSS Medical College, Mysuru
Introduction
• Hip USG was the first and most successful application of USG
in the musculoskeletal system.
• Dr. Graf was the first to realize the potential of USG.
• Real-time and multiplanar USG evaluation of the hip was
introduced soon thereafter by Novick G[2] and Harcke et al.
• The sensitivity and specificity of USG for the diagnosis of hip
dysplasia is nearly 100%.](https://image.slidesharecdn.com/vishwajcppt-190531070520/85/Hip-ultrasonography-in-infants-and-children-3-320.jpg)