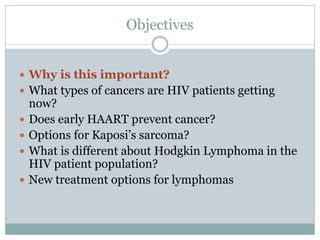
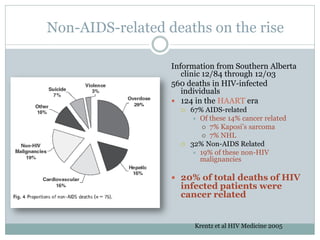
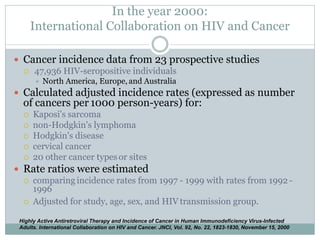
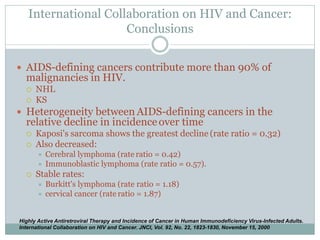
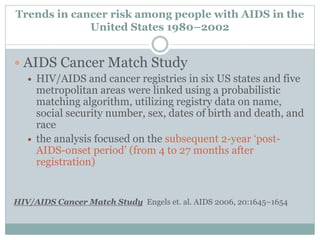
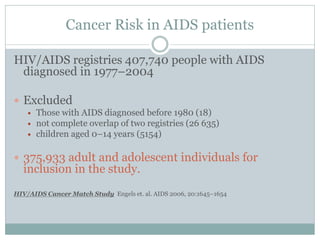
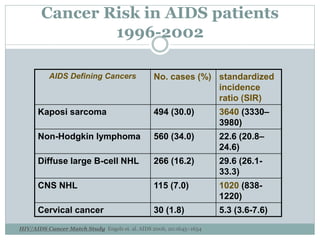
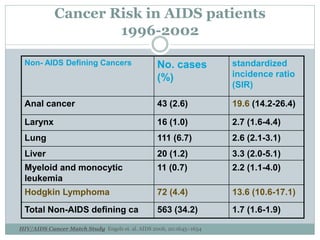
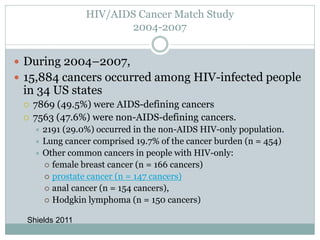
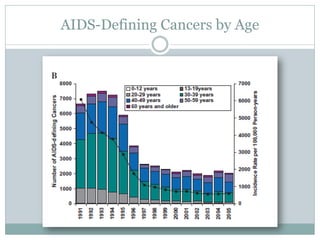
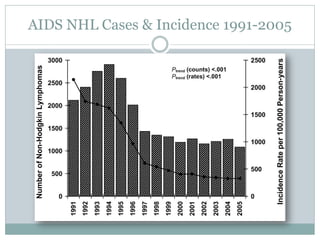
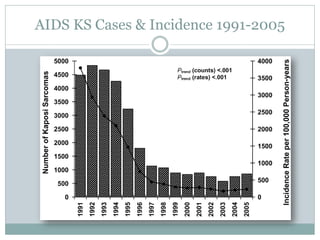
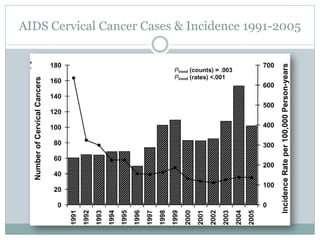
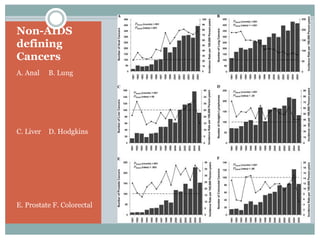
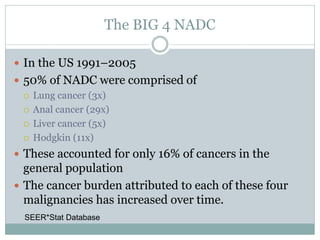
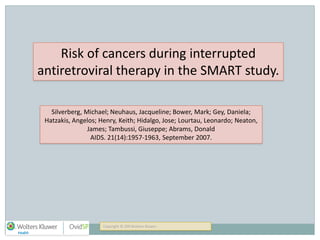
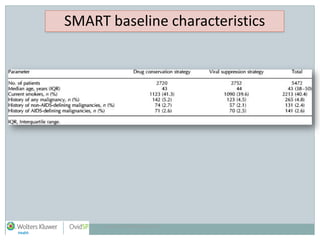
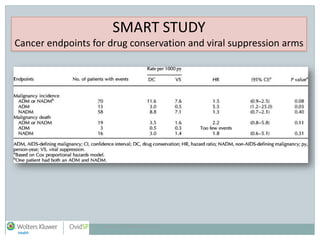
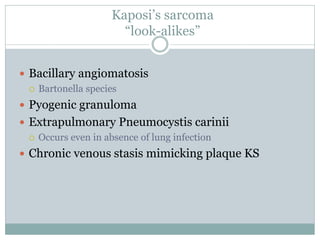
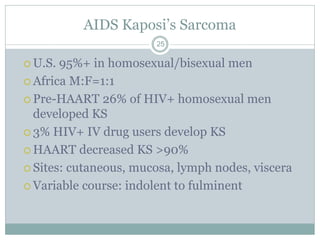
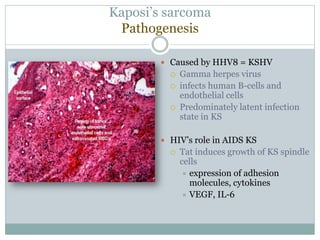
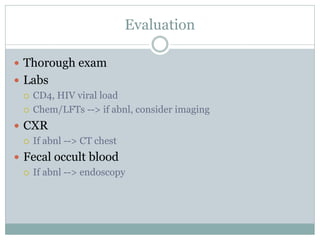
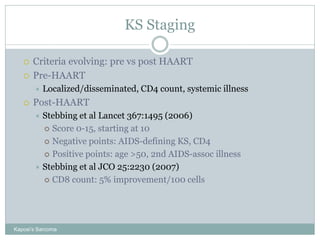
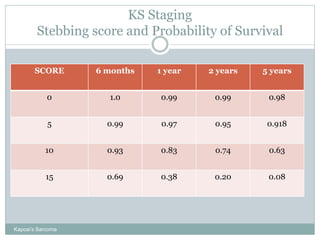
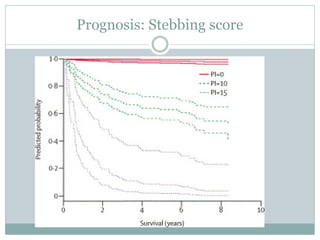
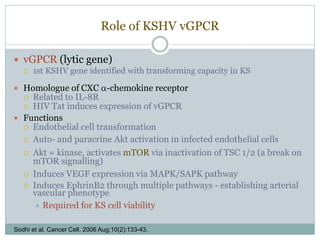
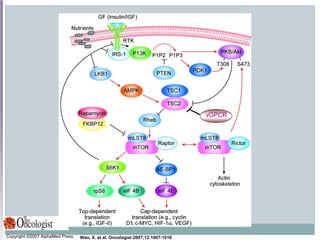
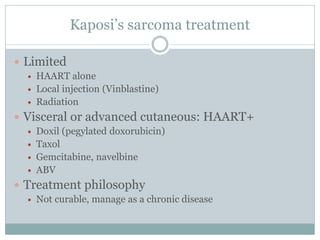
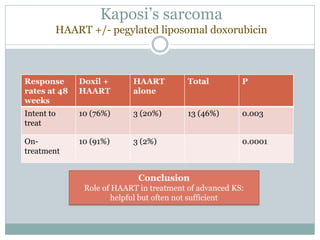
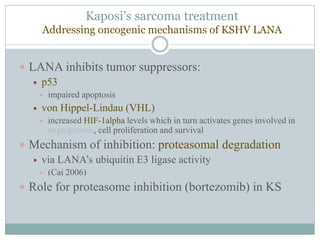
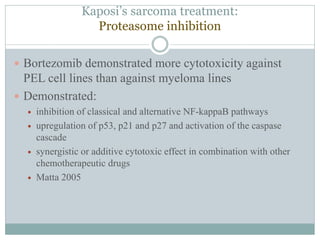
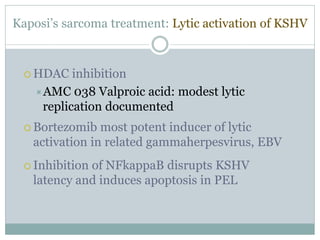
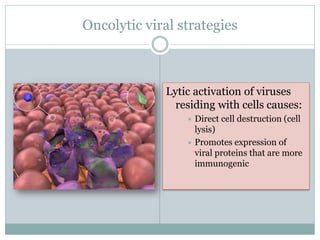
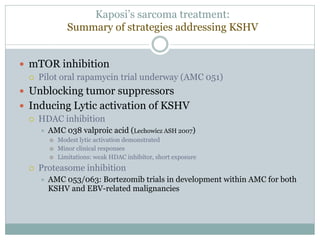
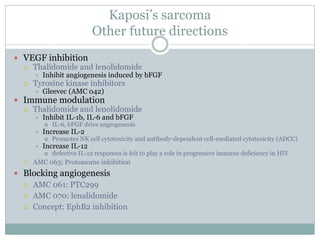
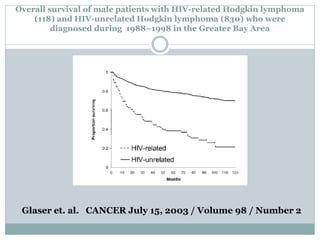
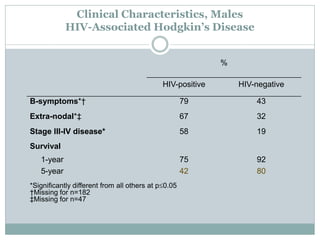
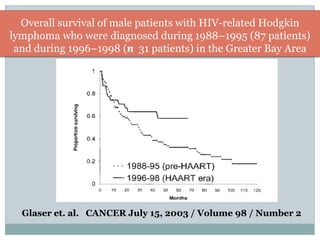
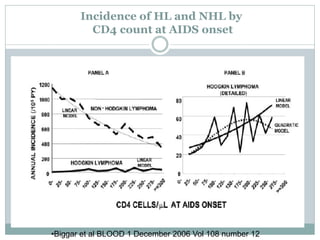
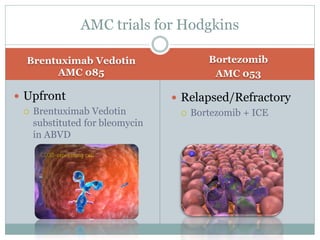
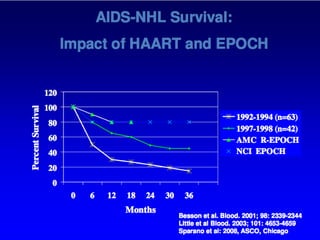
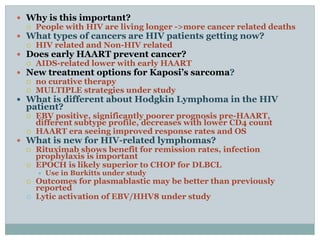
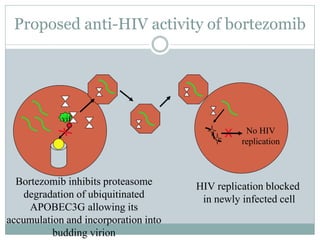
The document summarizes a presentation on AIDS-related malignancies. It discusses trends seen in cancers affecting HIV/AIDS patients, including declines in AIDS-defining cancers like Kaposi's sarcoma and non-Hodgkin's lymphoma since the introduction of HAART. It also examines increases seen in certain non-AIDS defining cancers. Treatment options for Kaposi's sarcoma are reviewed, including the role of HAART and experimental approaches targeting KSHV mechanisms.