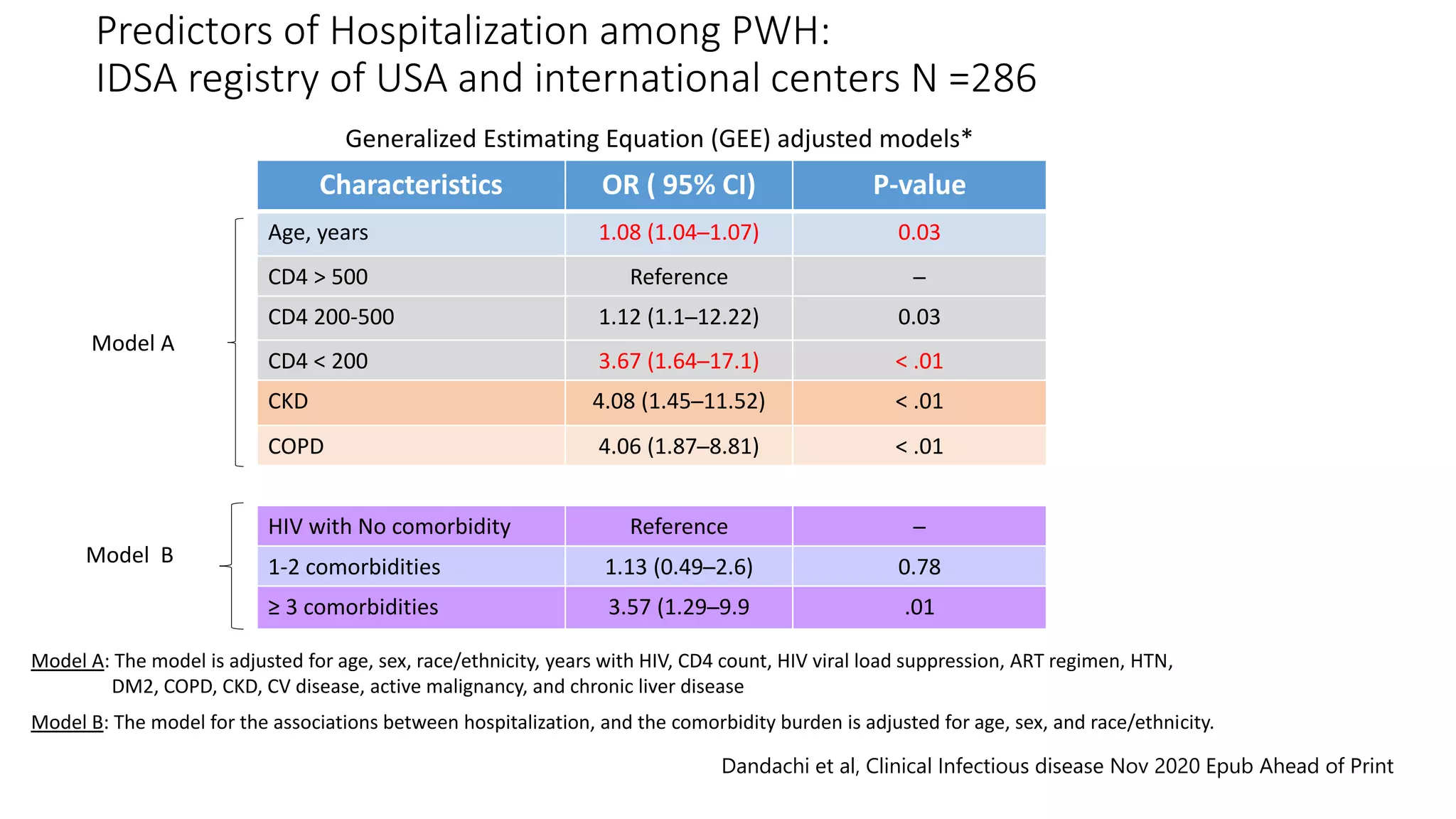
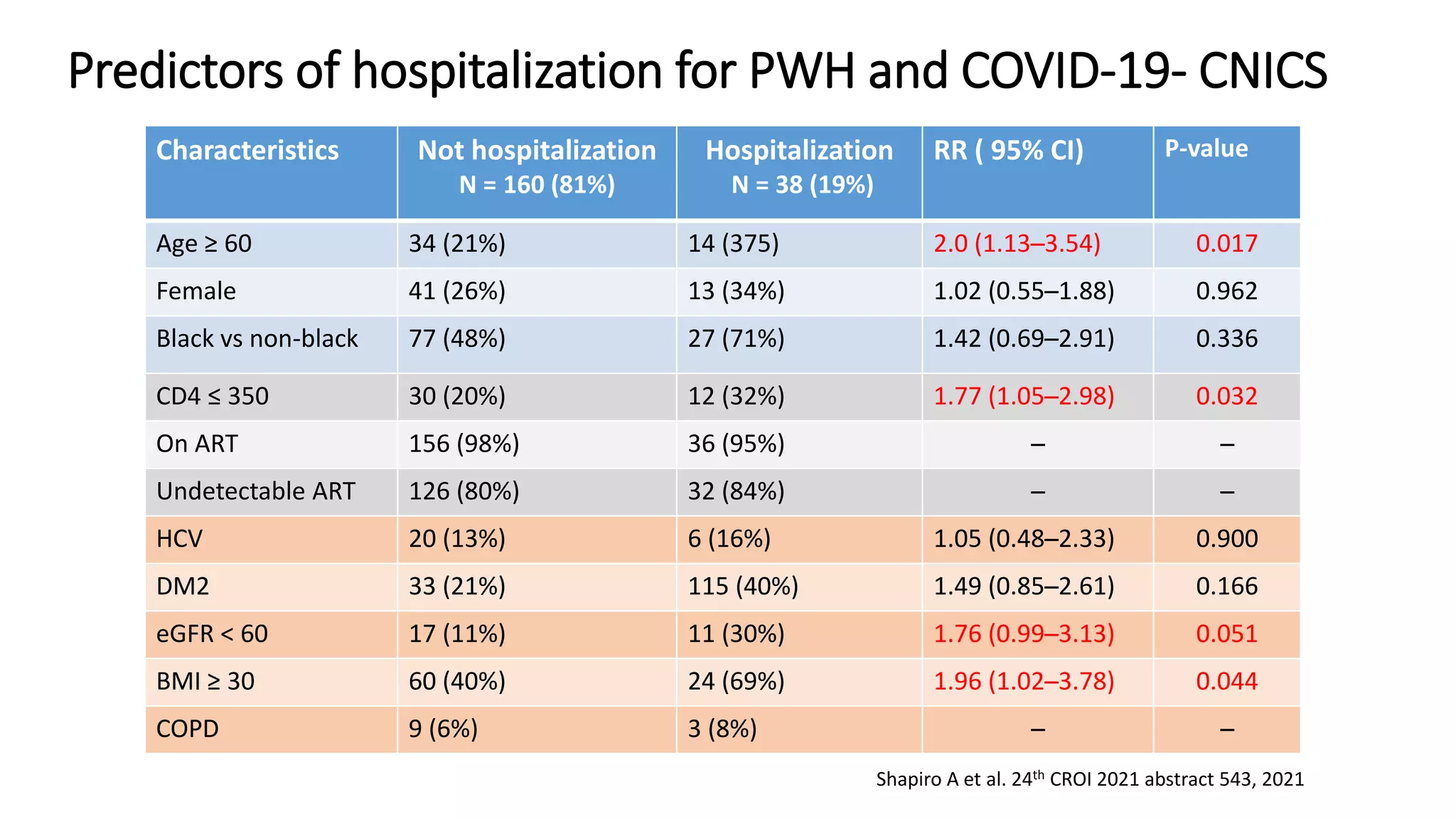
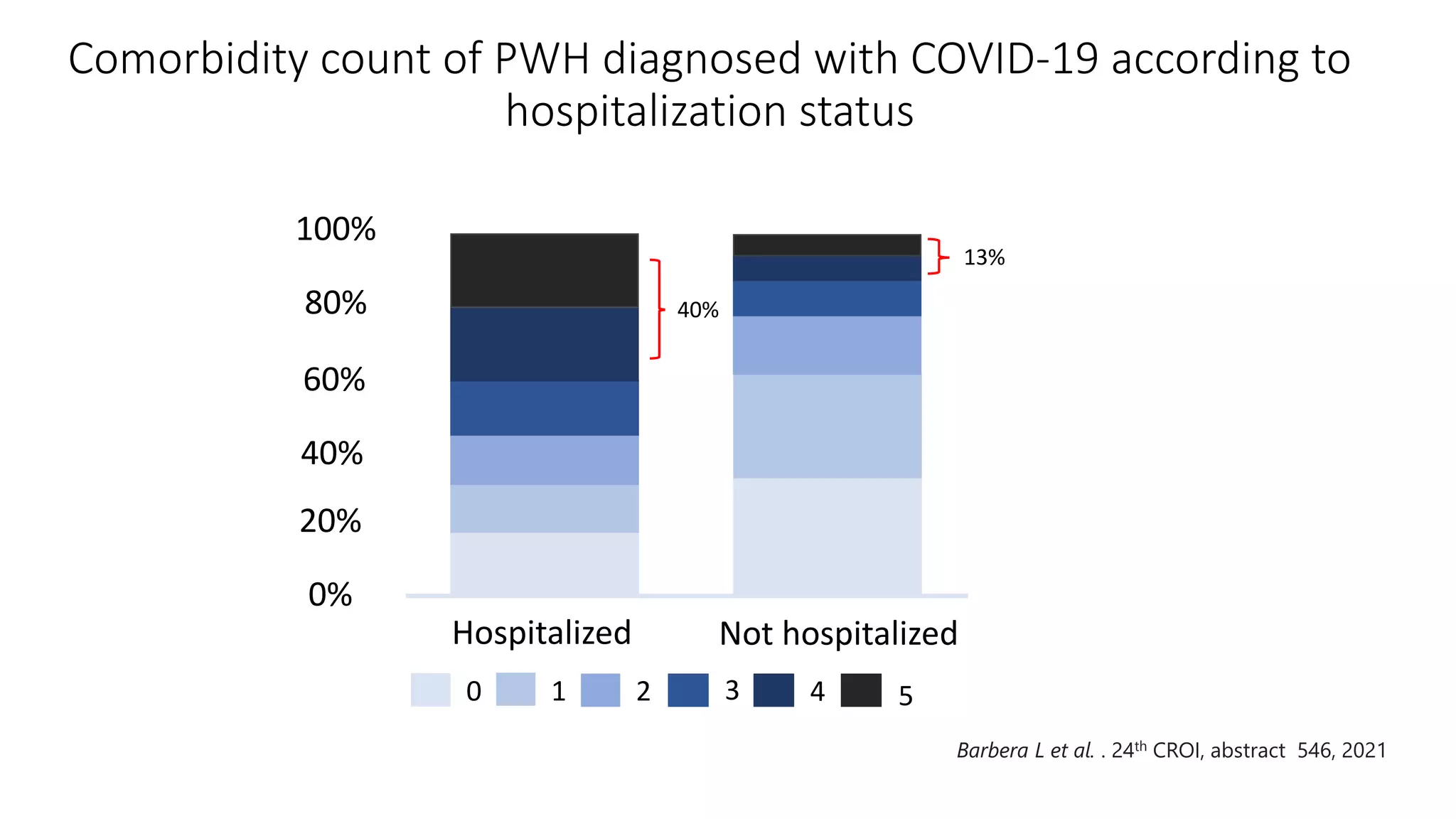
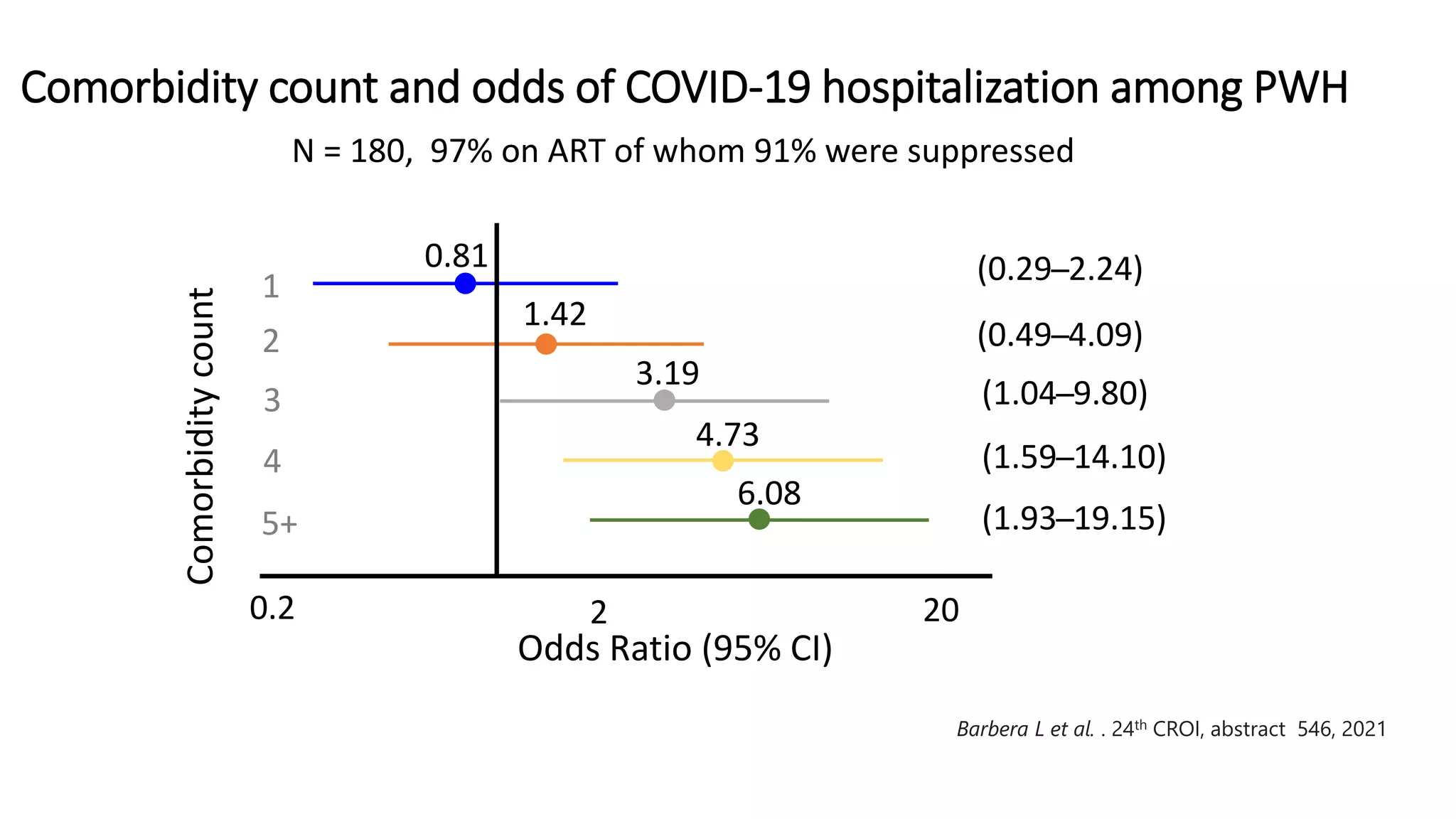
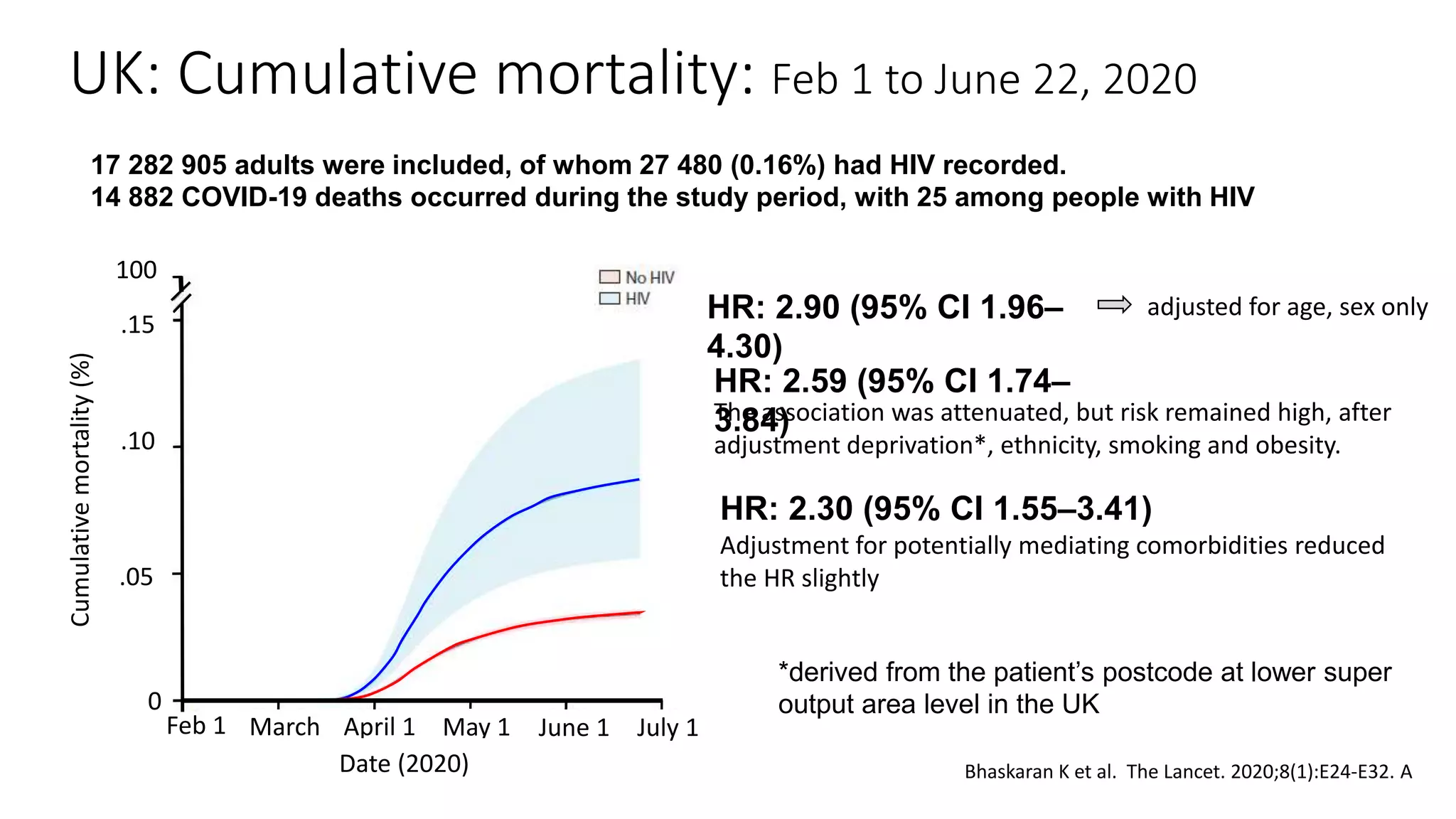
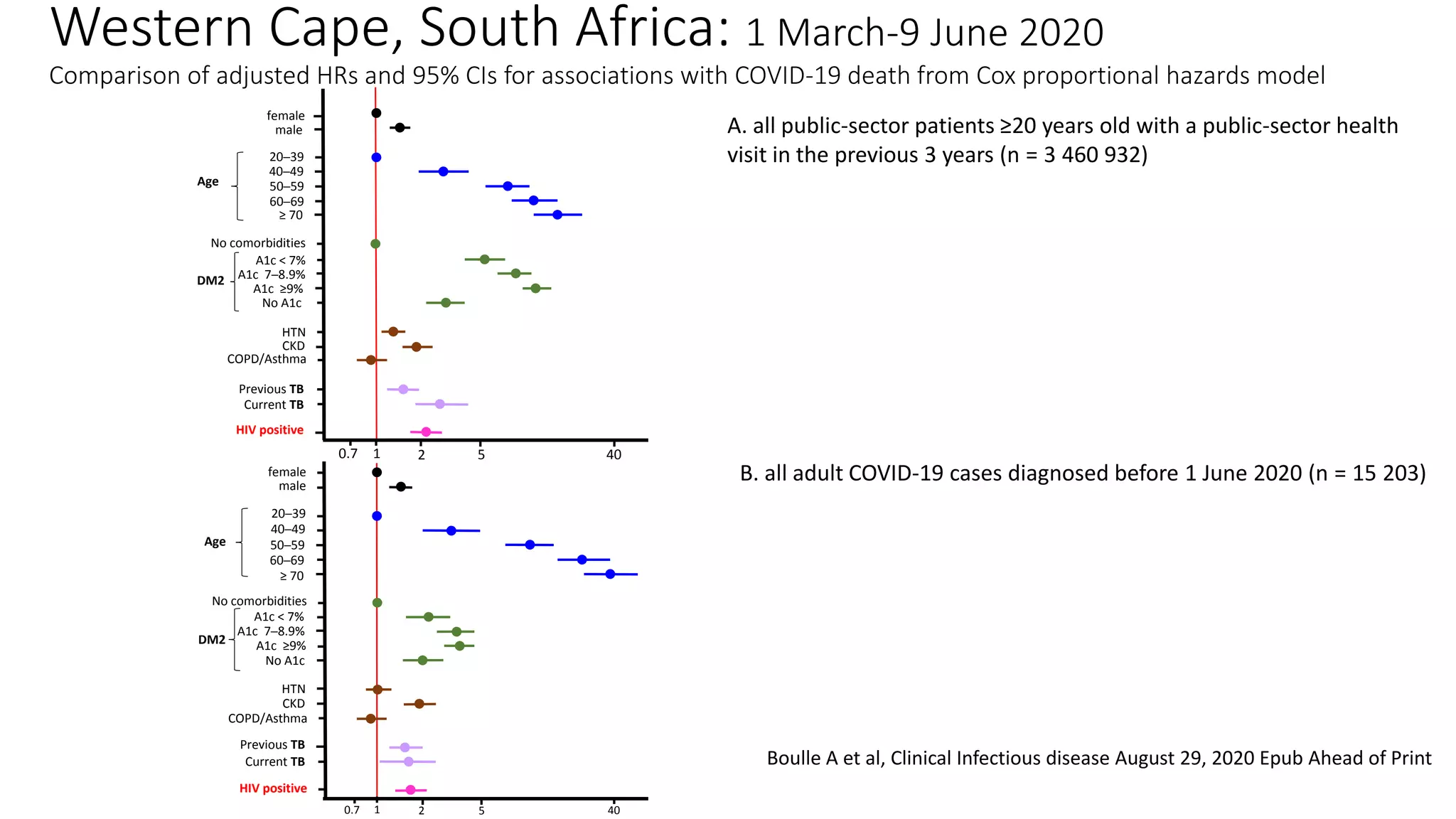
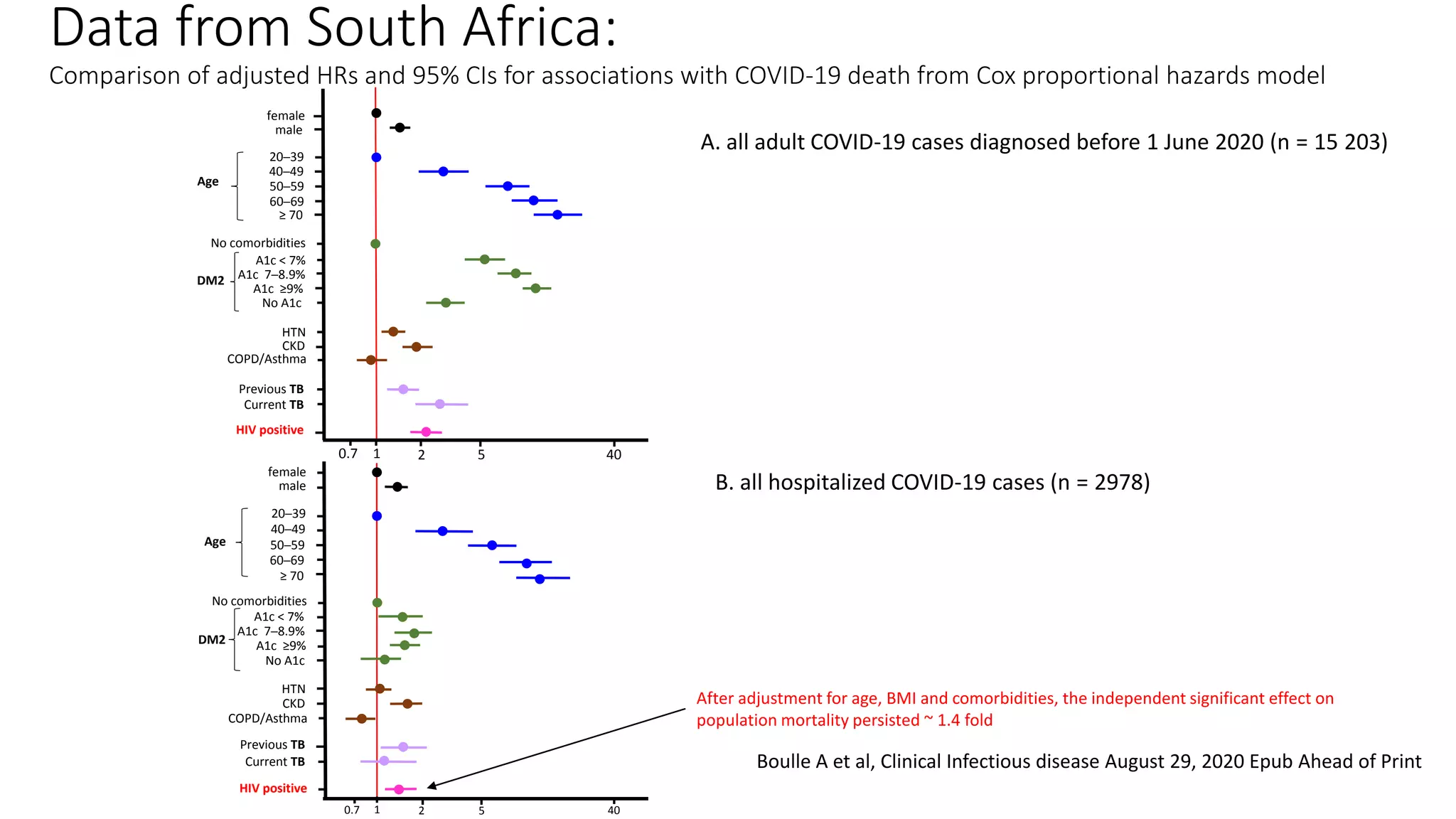
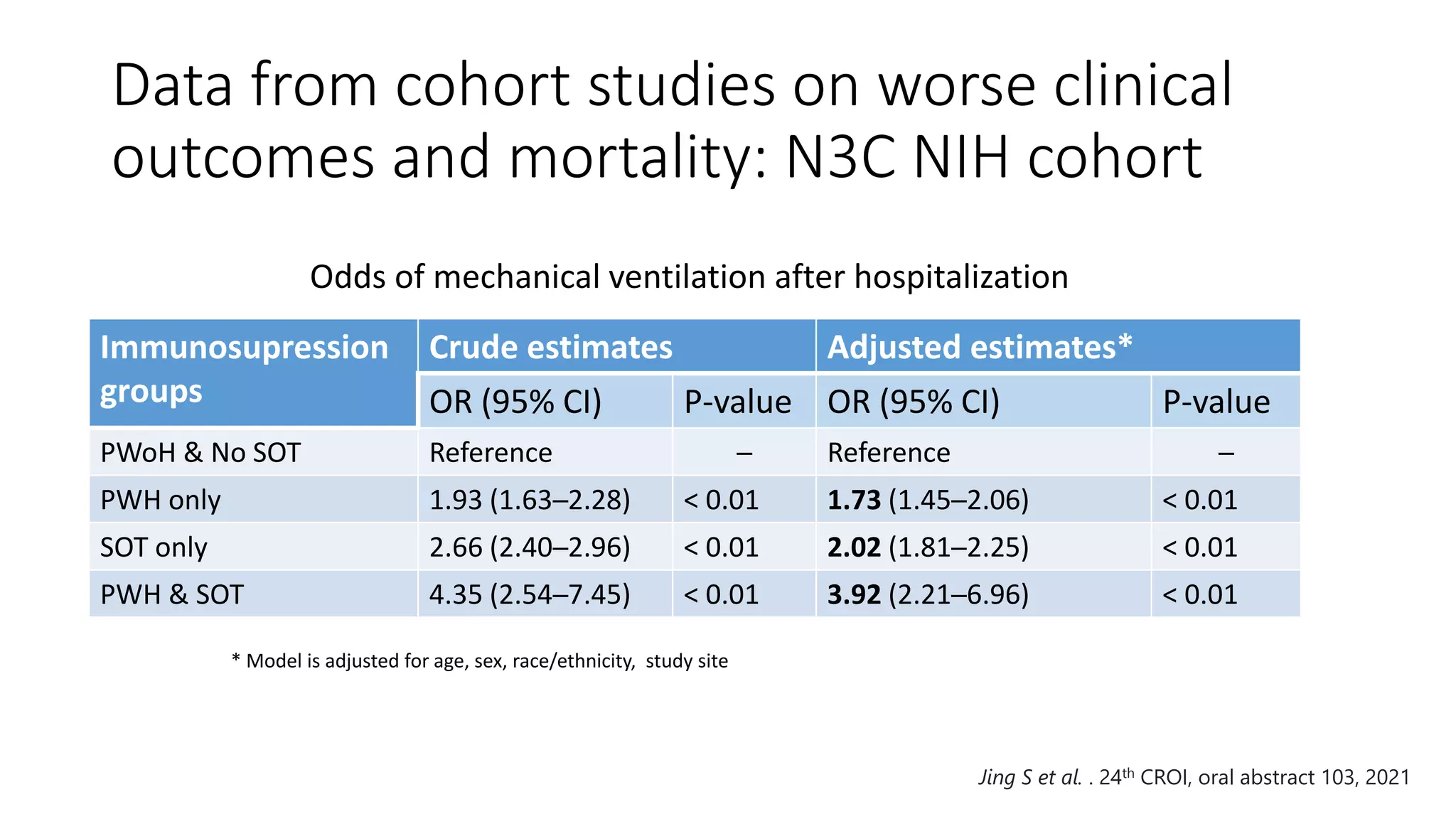
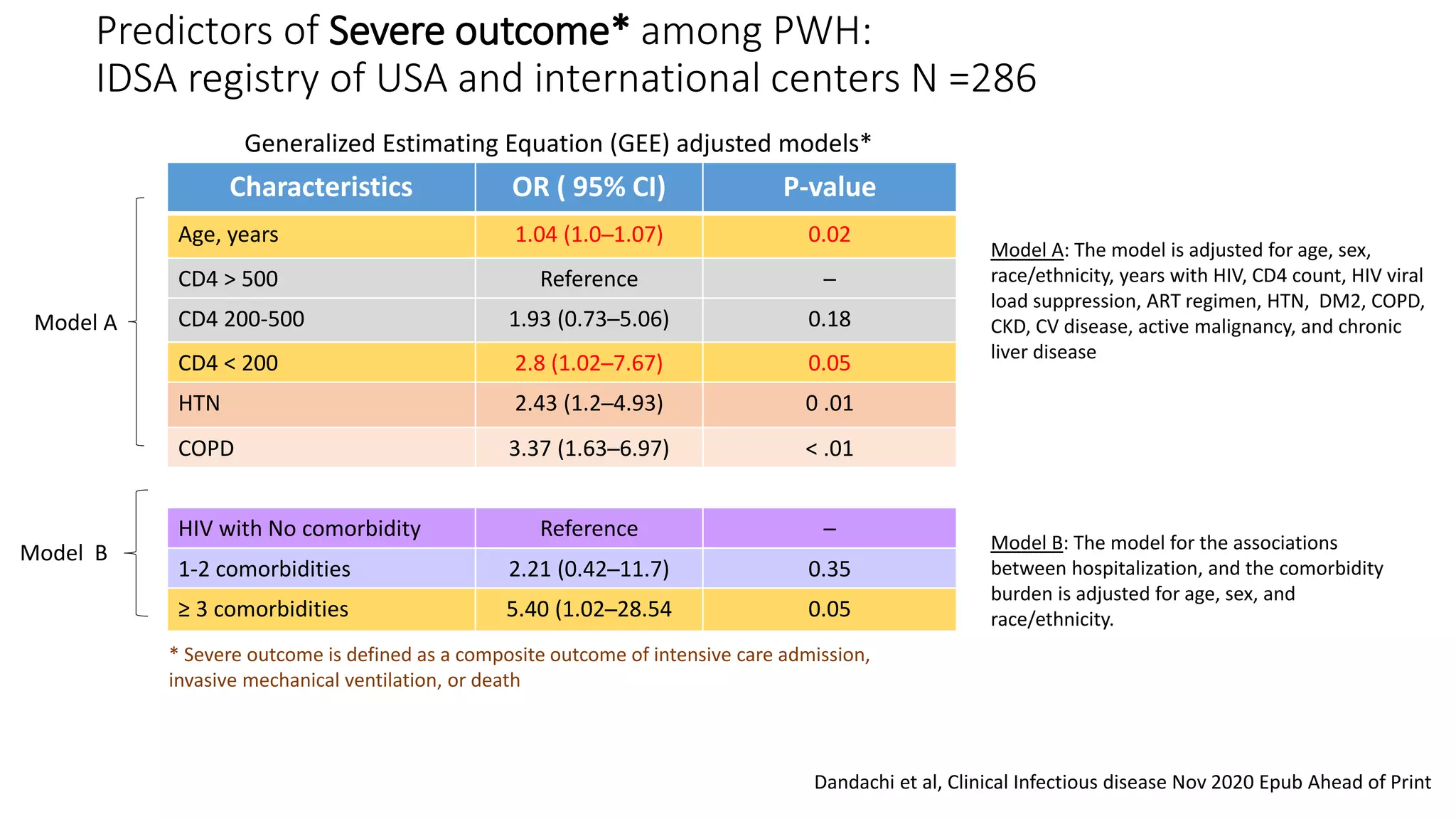
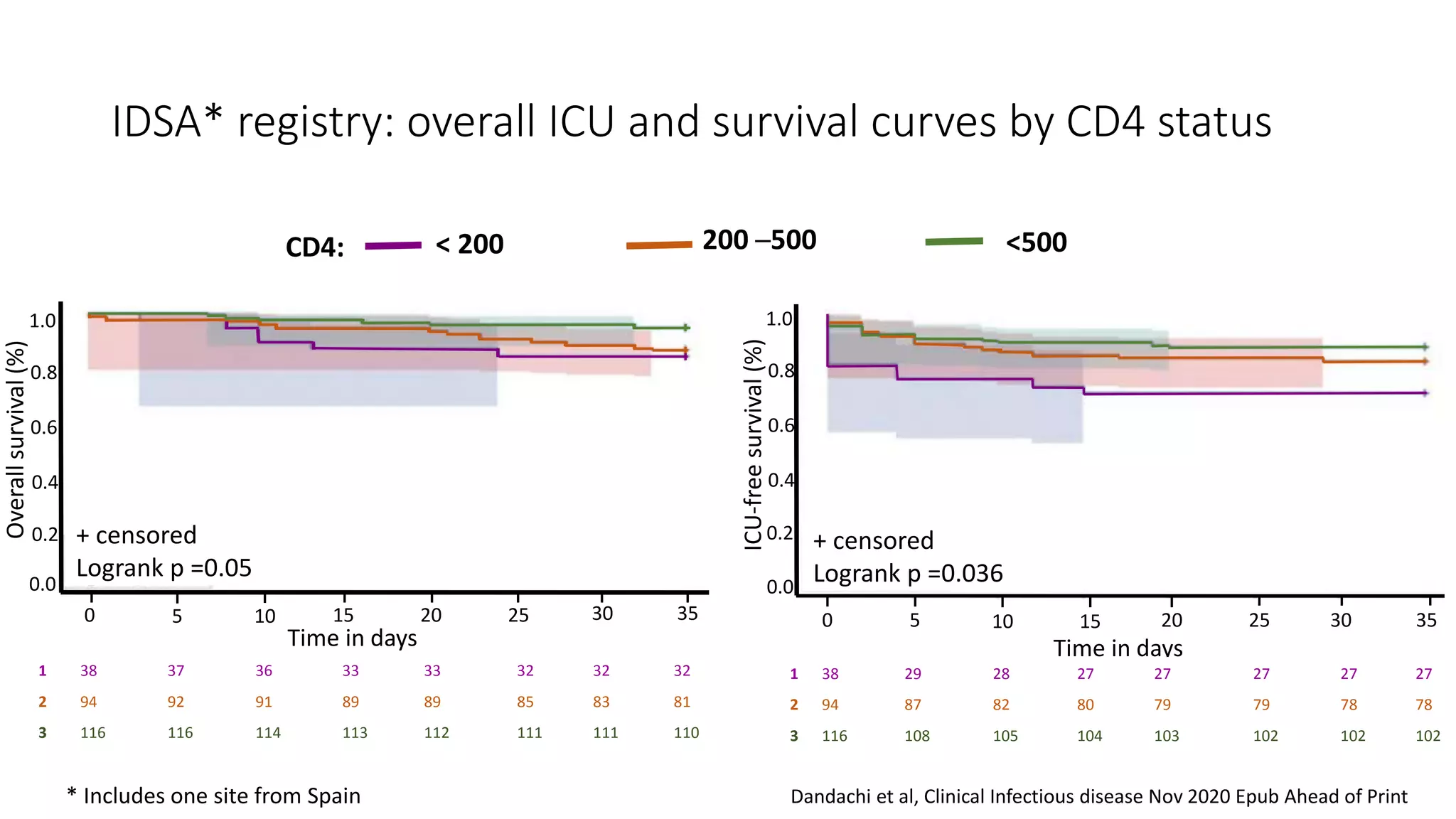
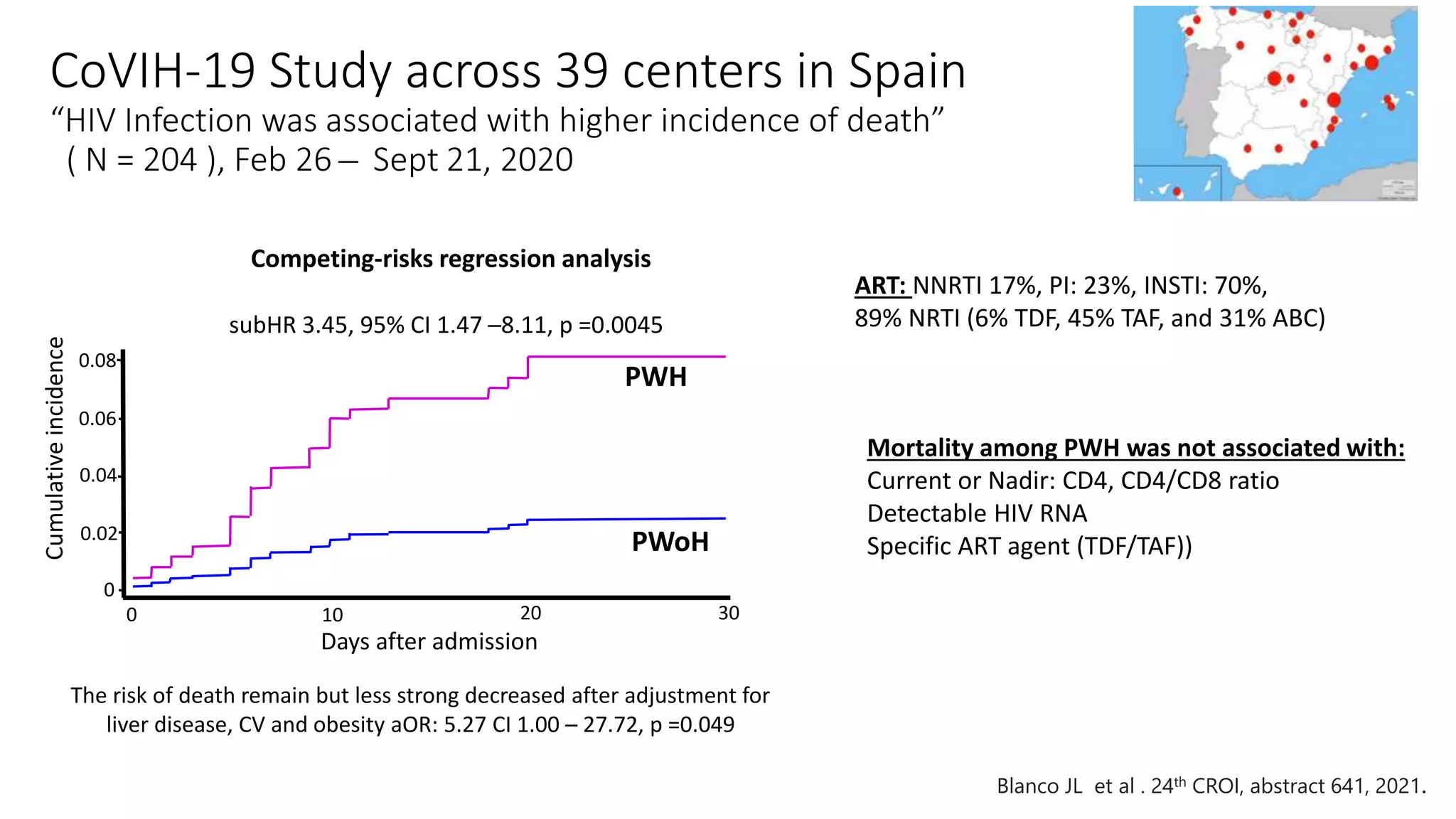
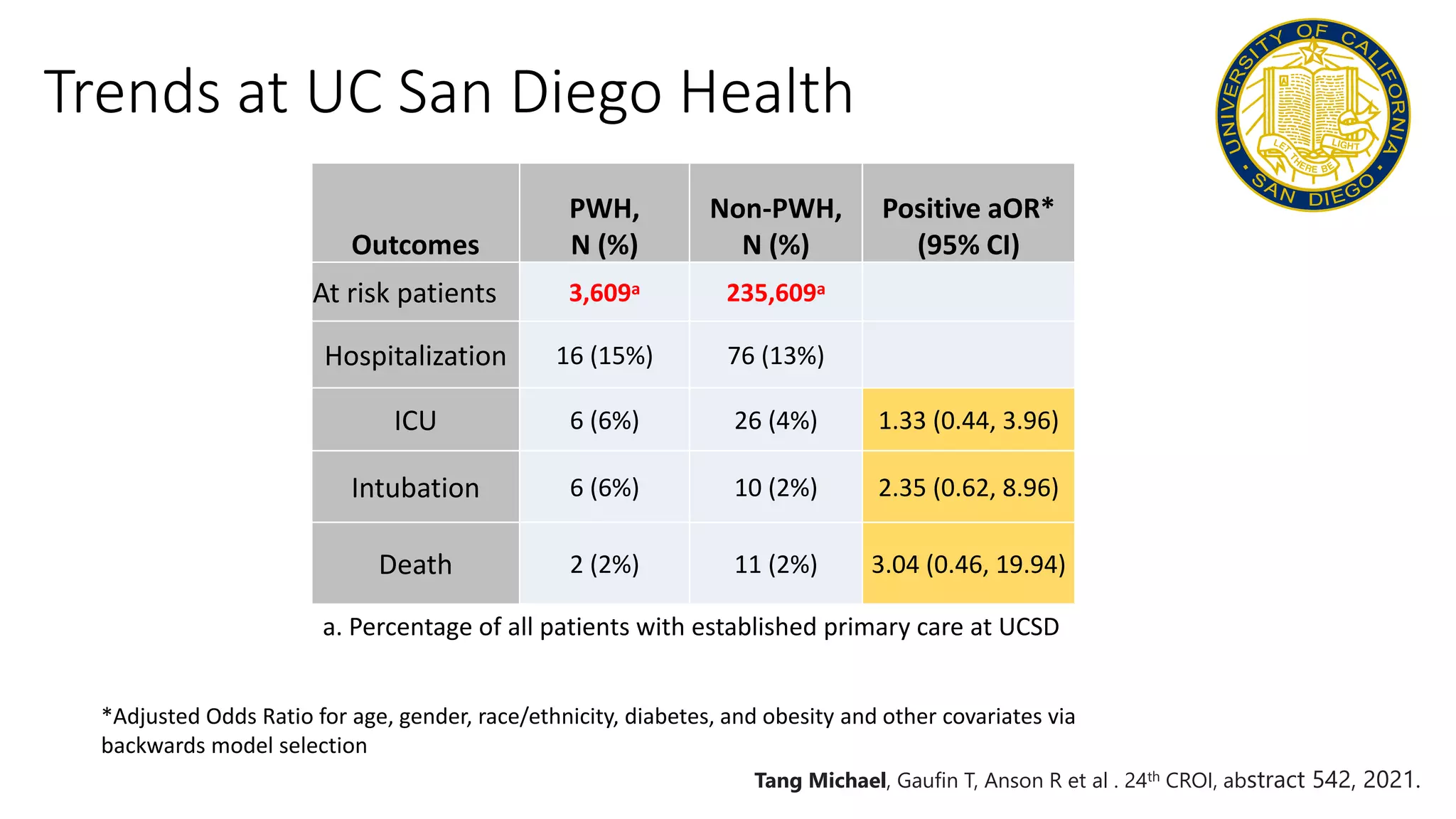
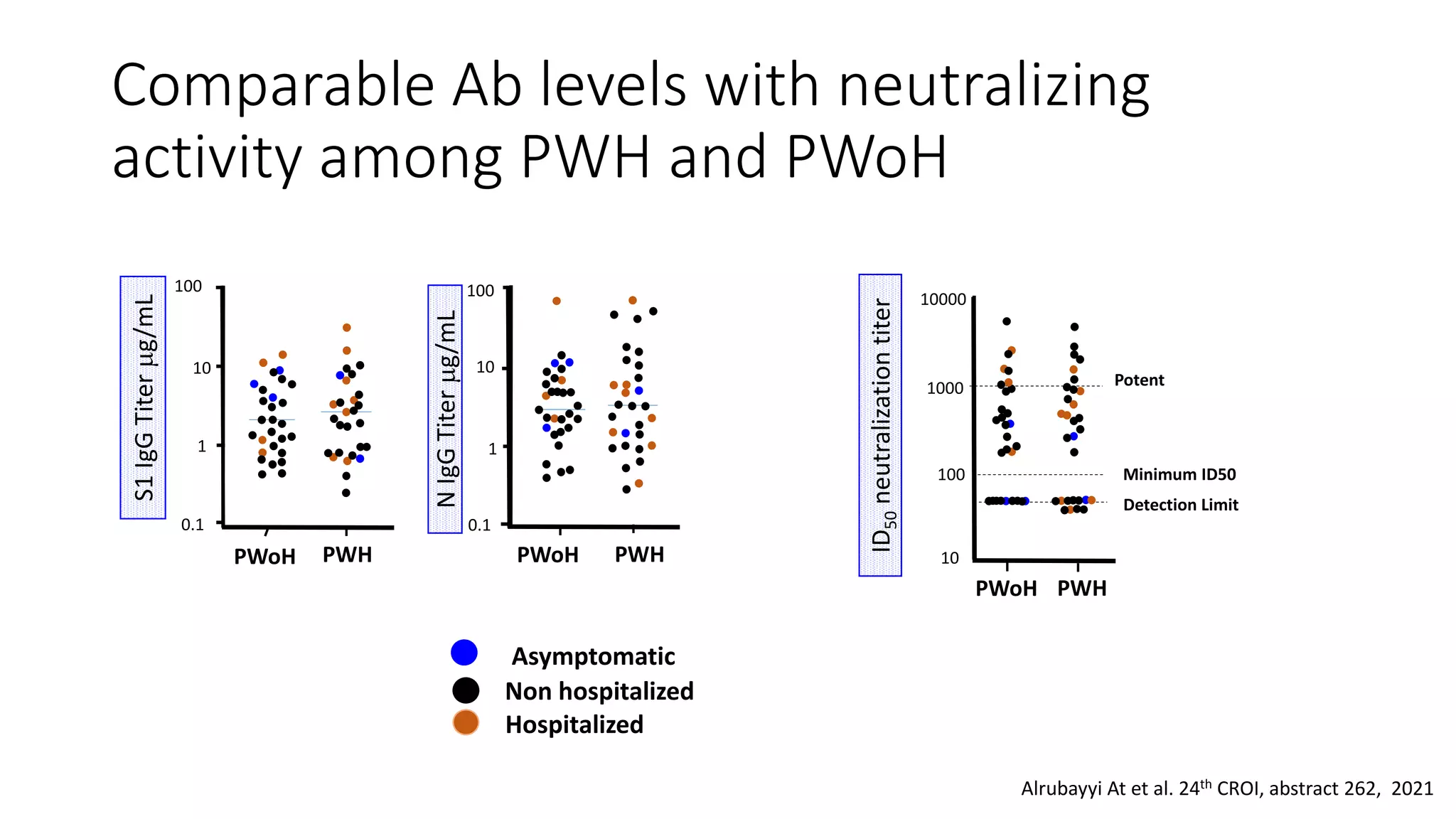
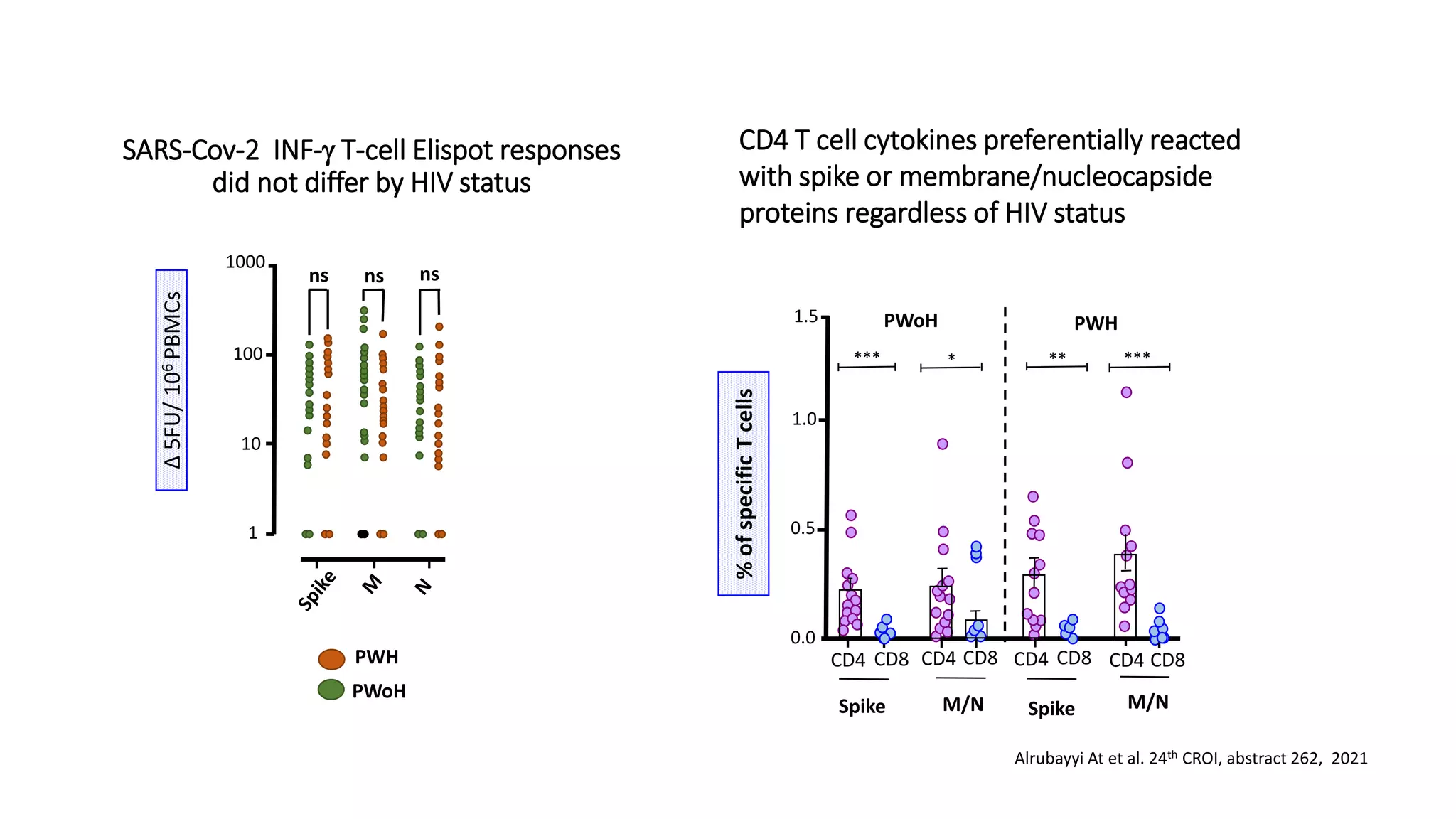
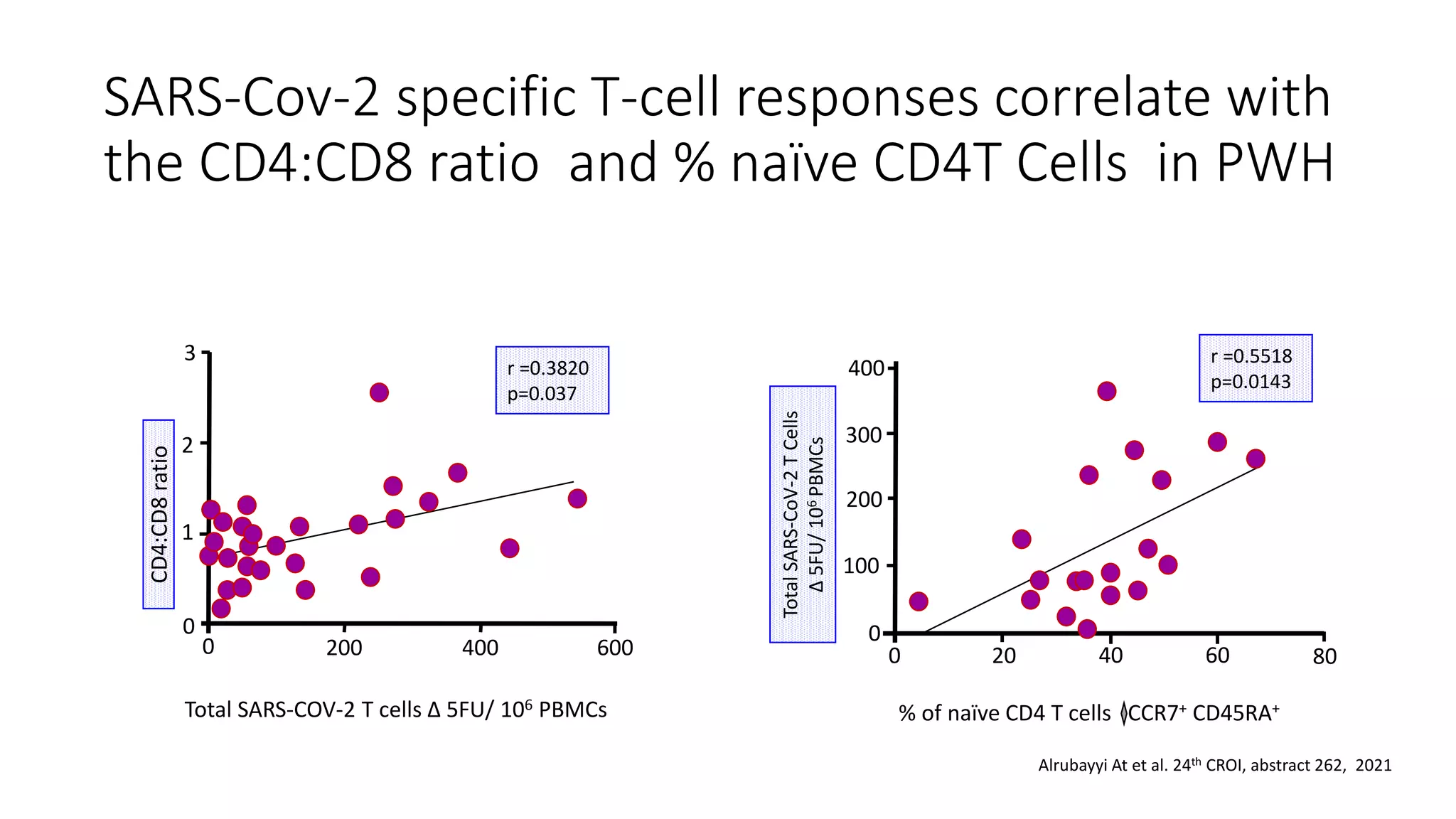
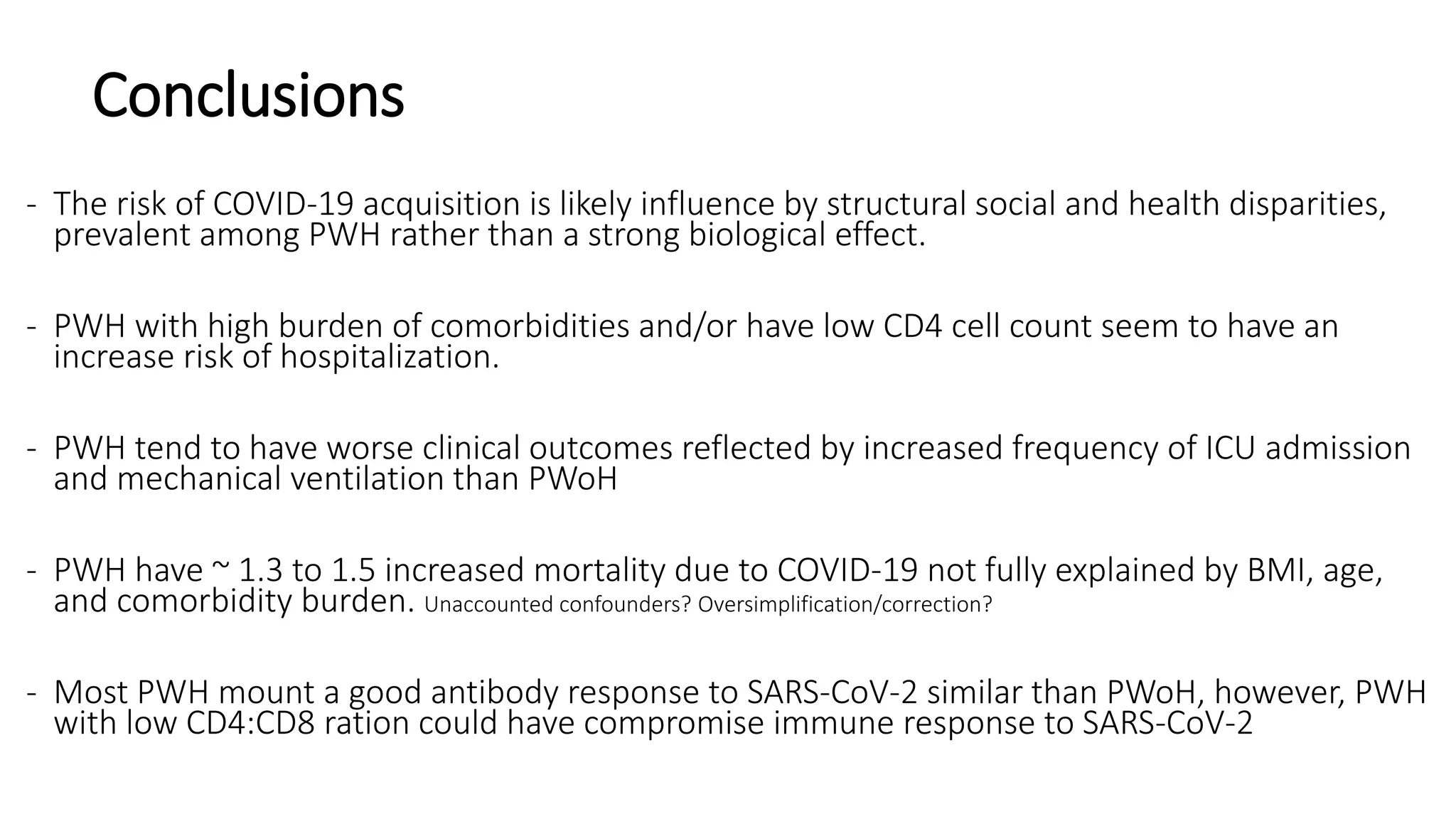
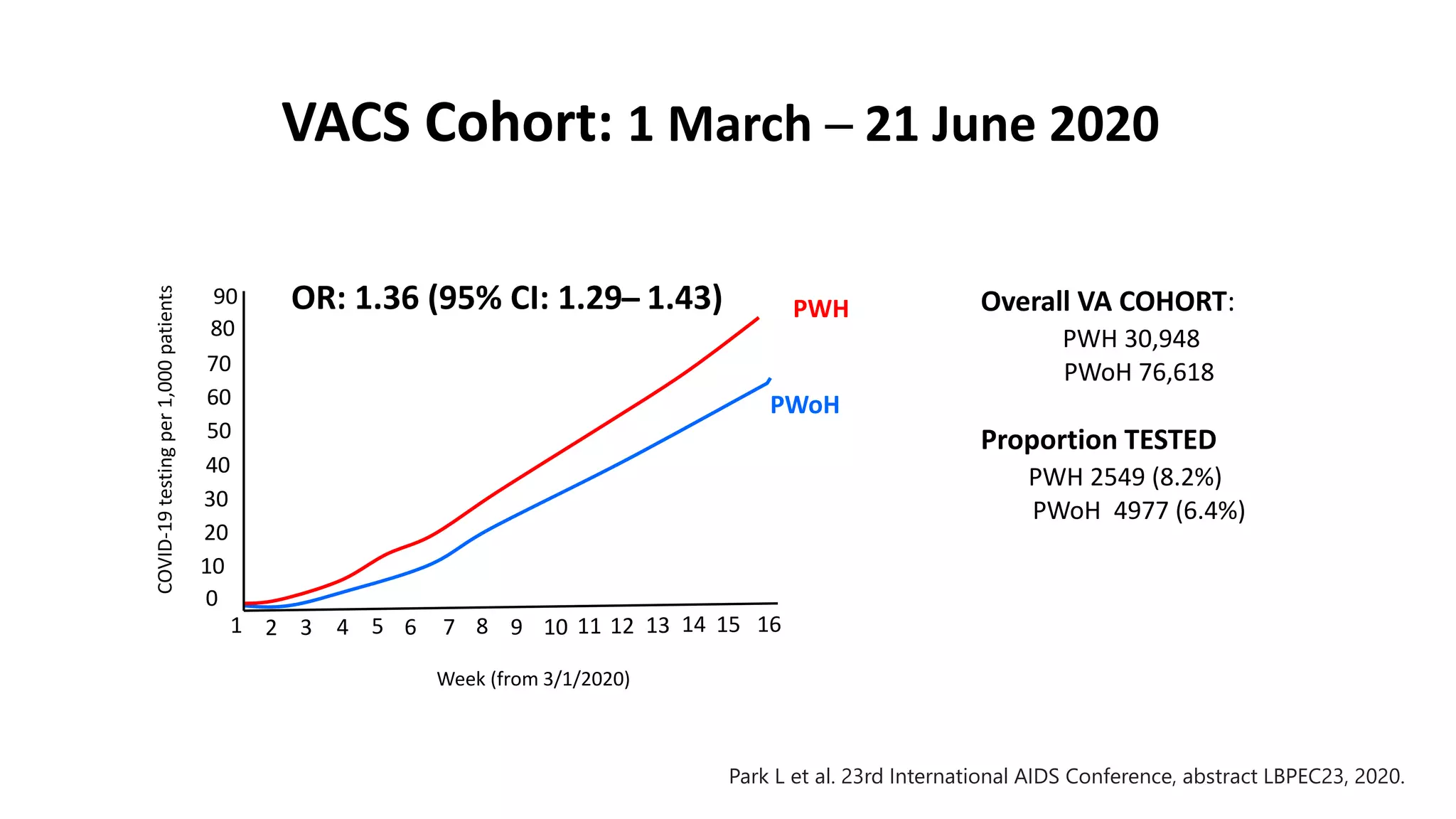
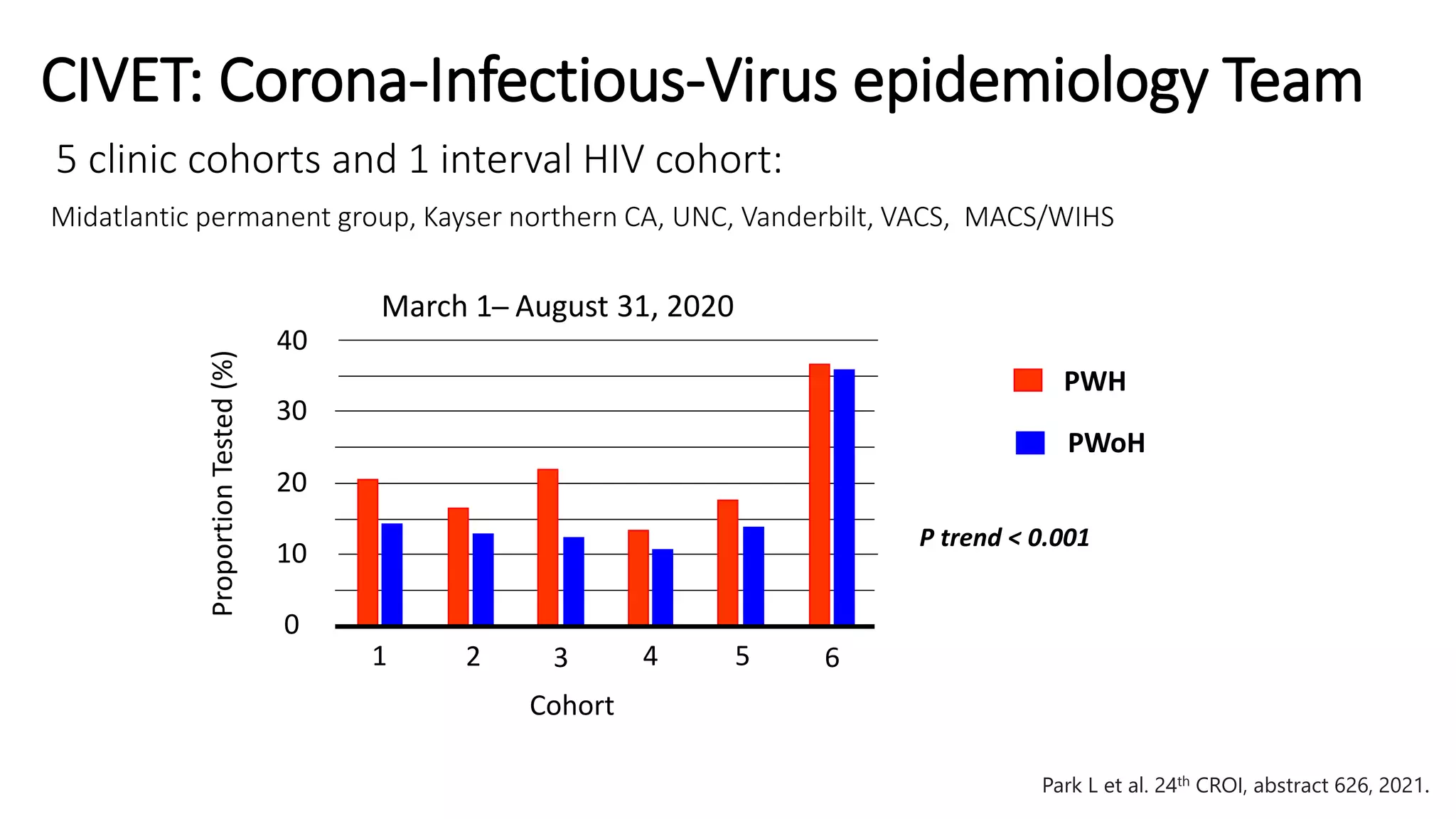
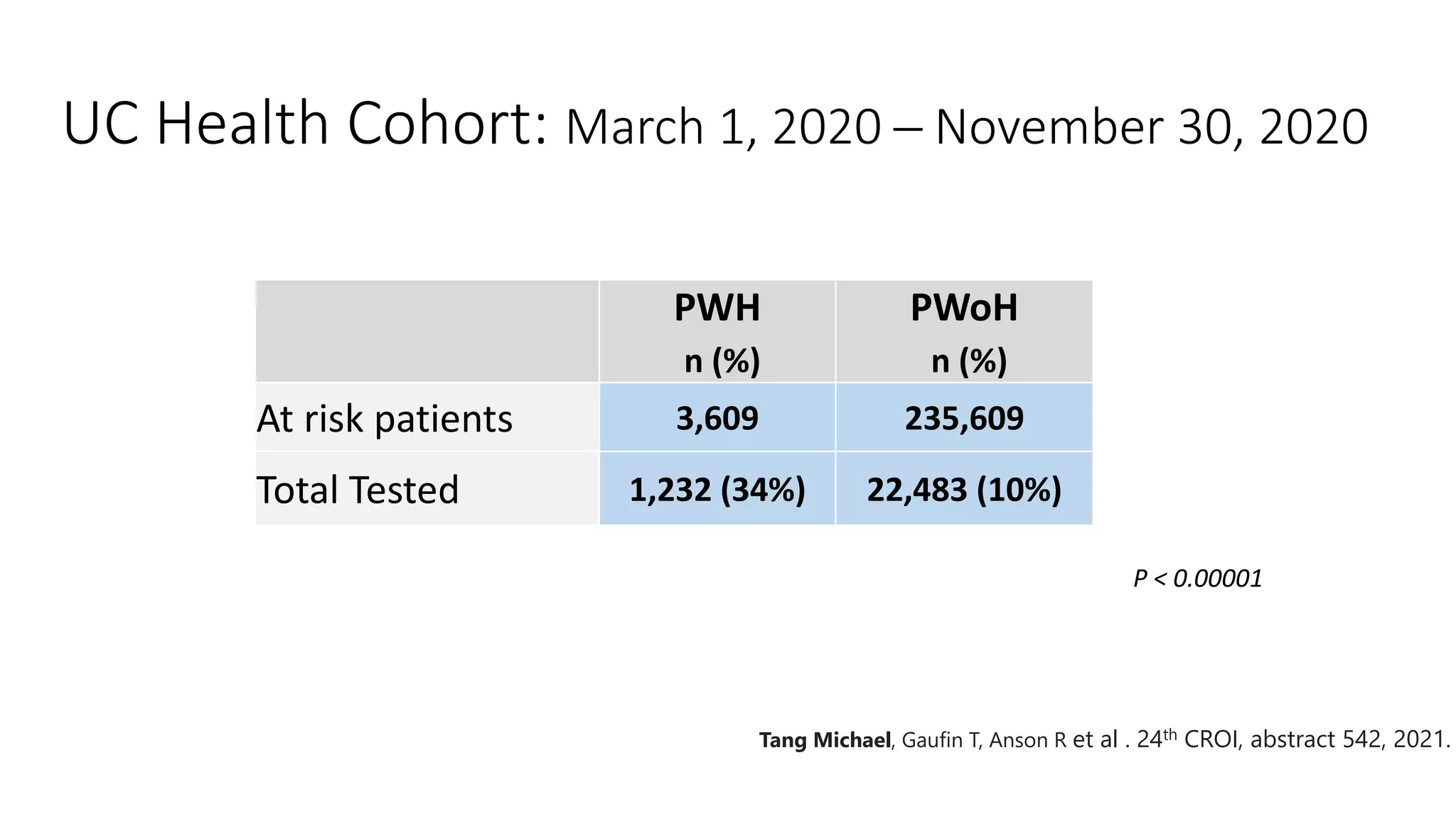
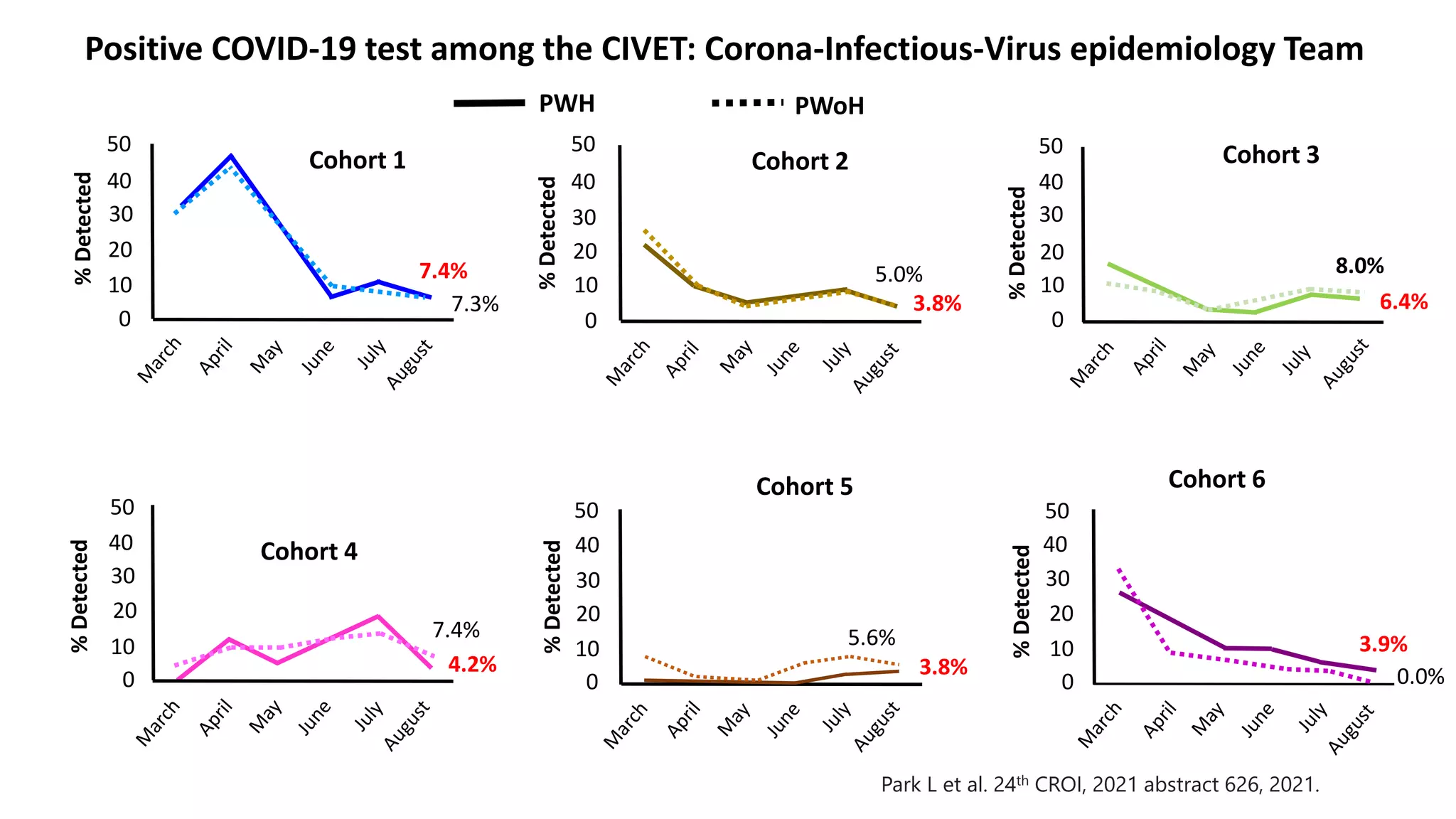
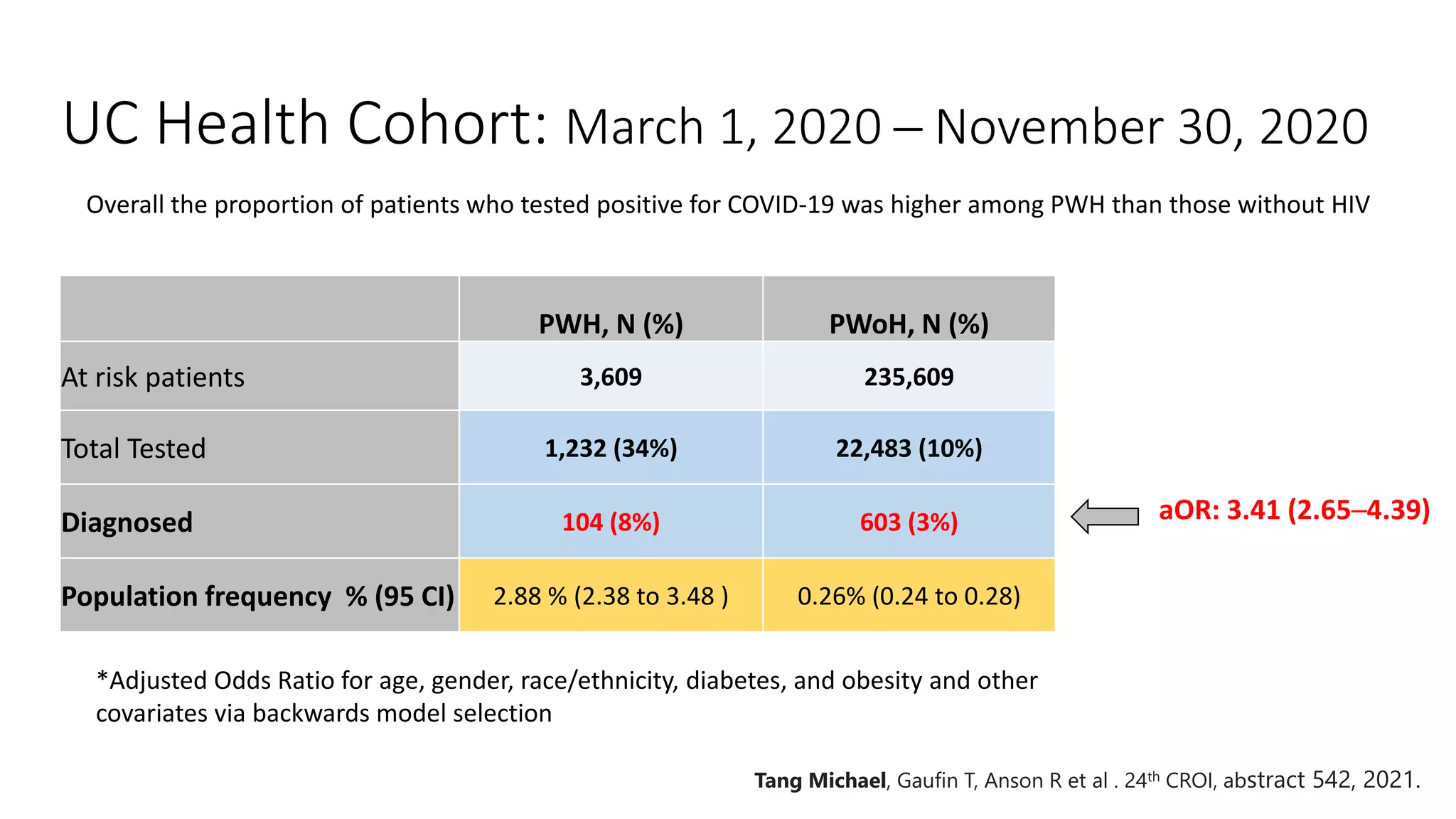
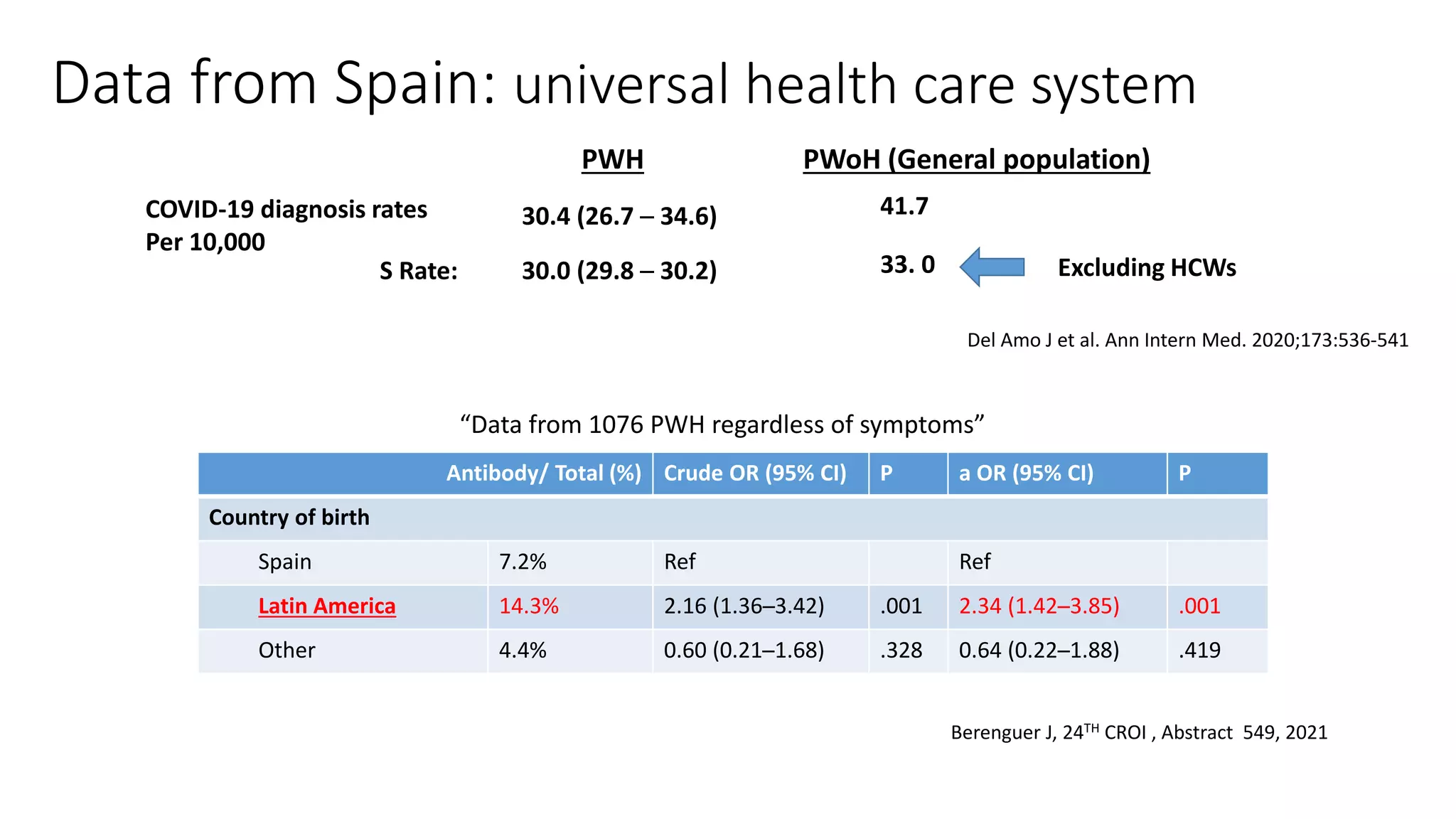
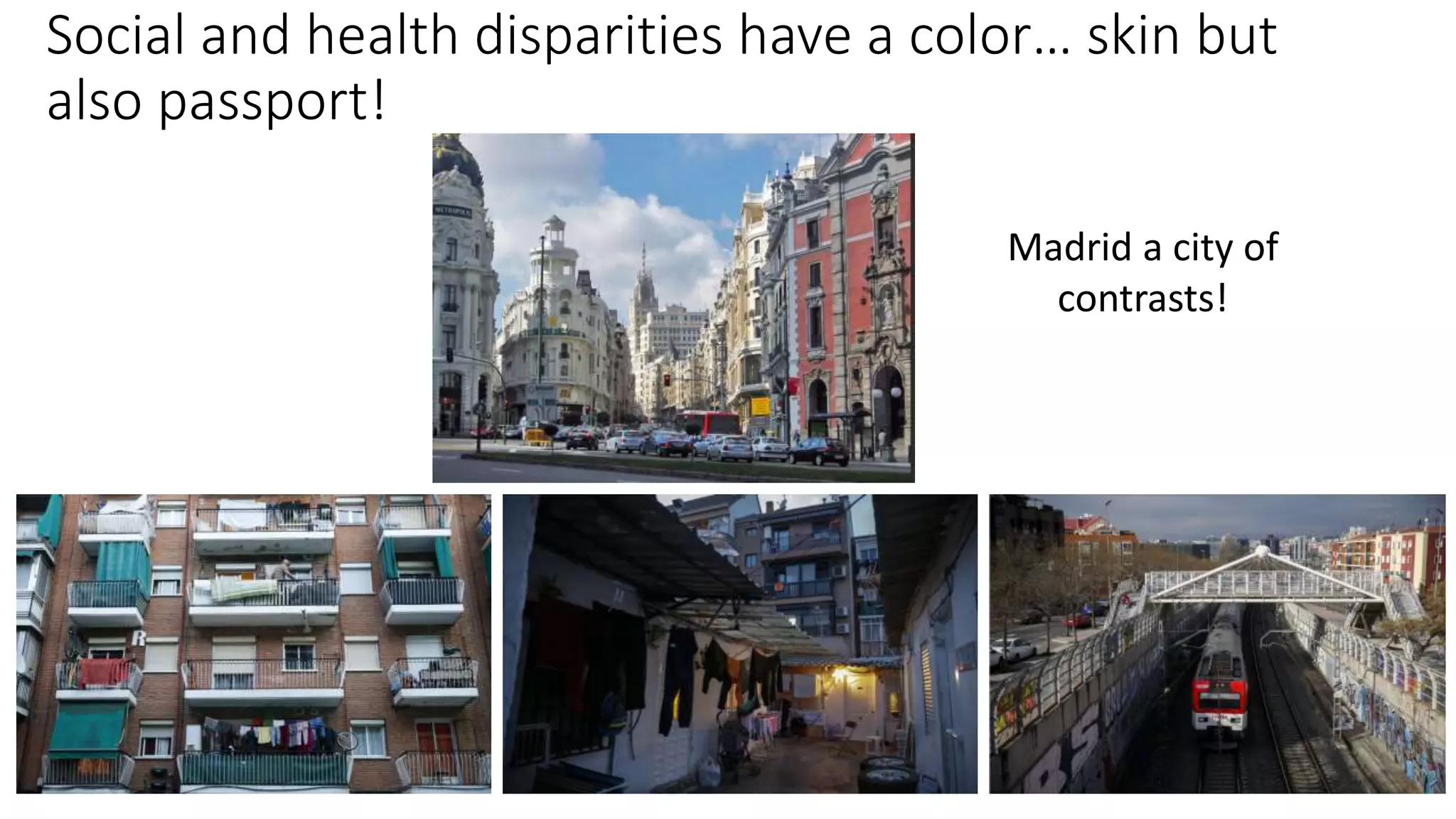
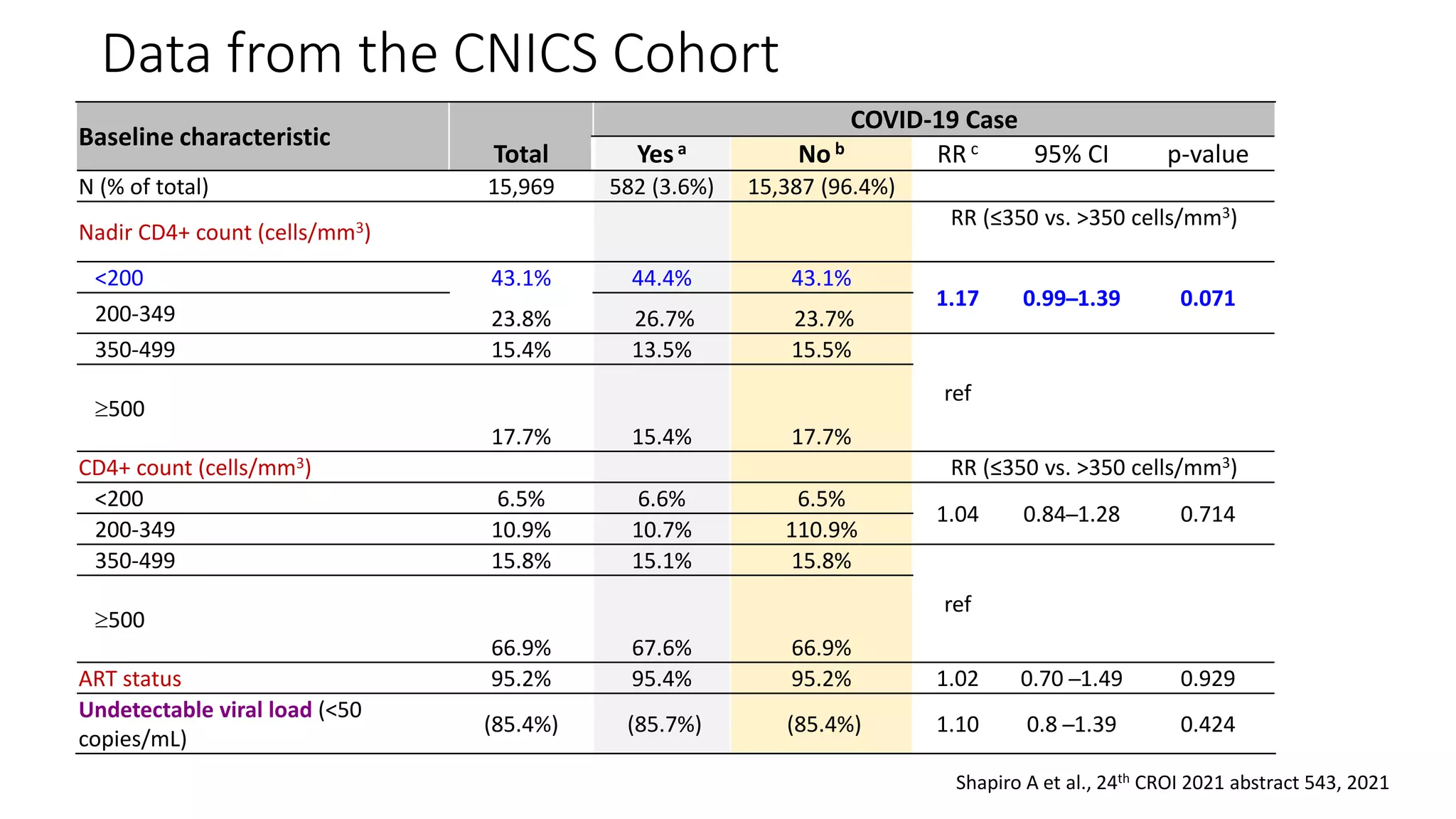
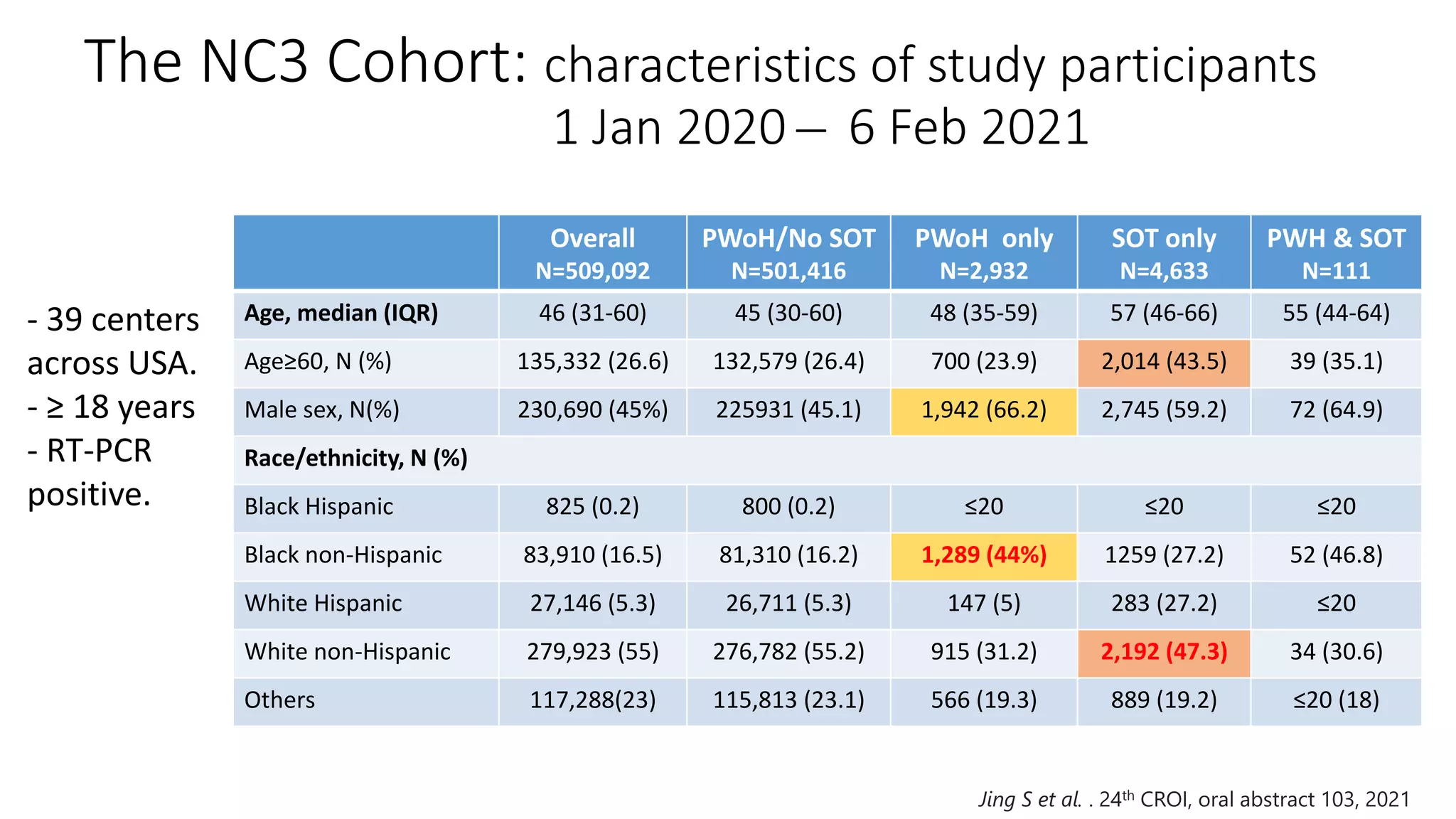
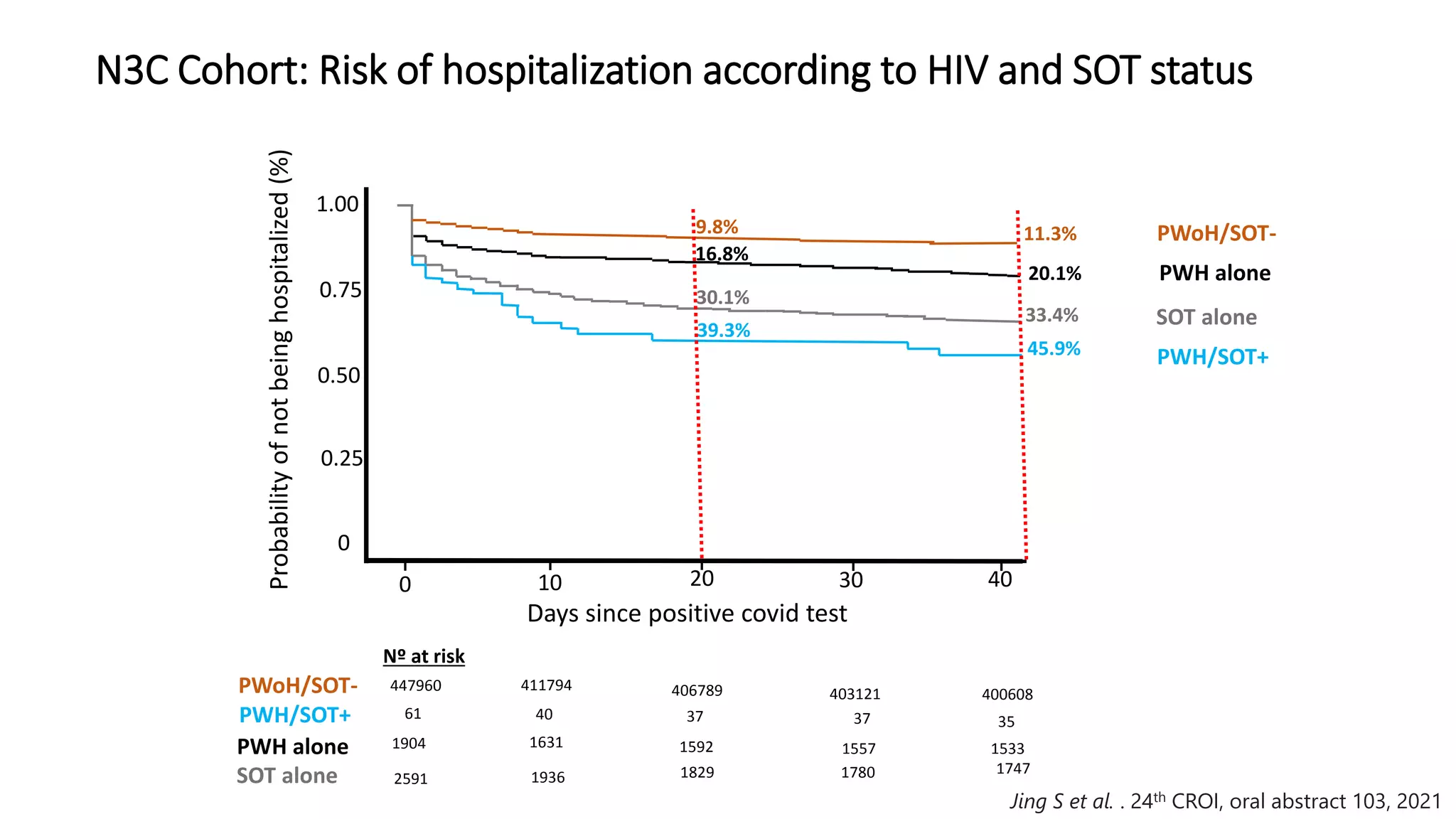
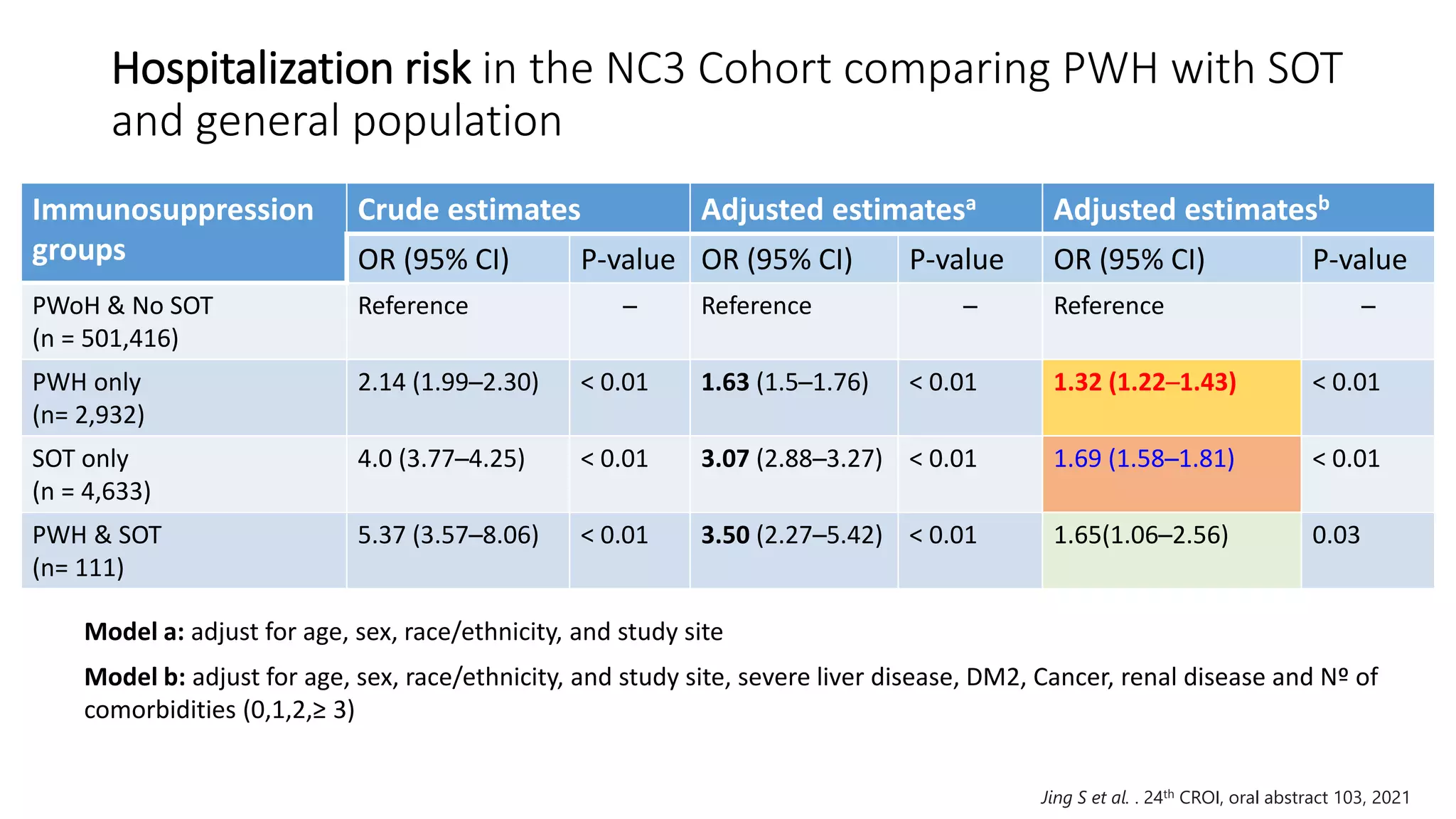
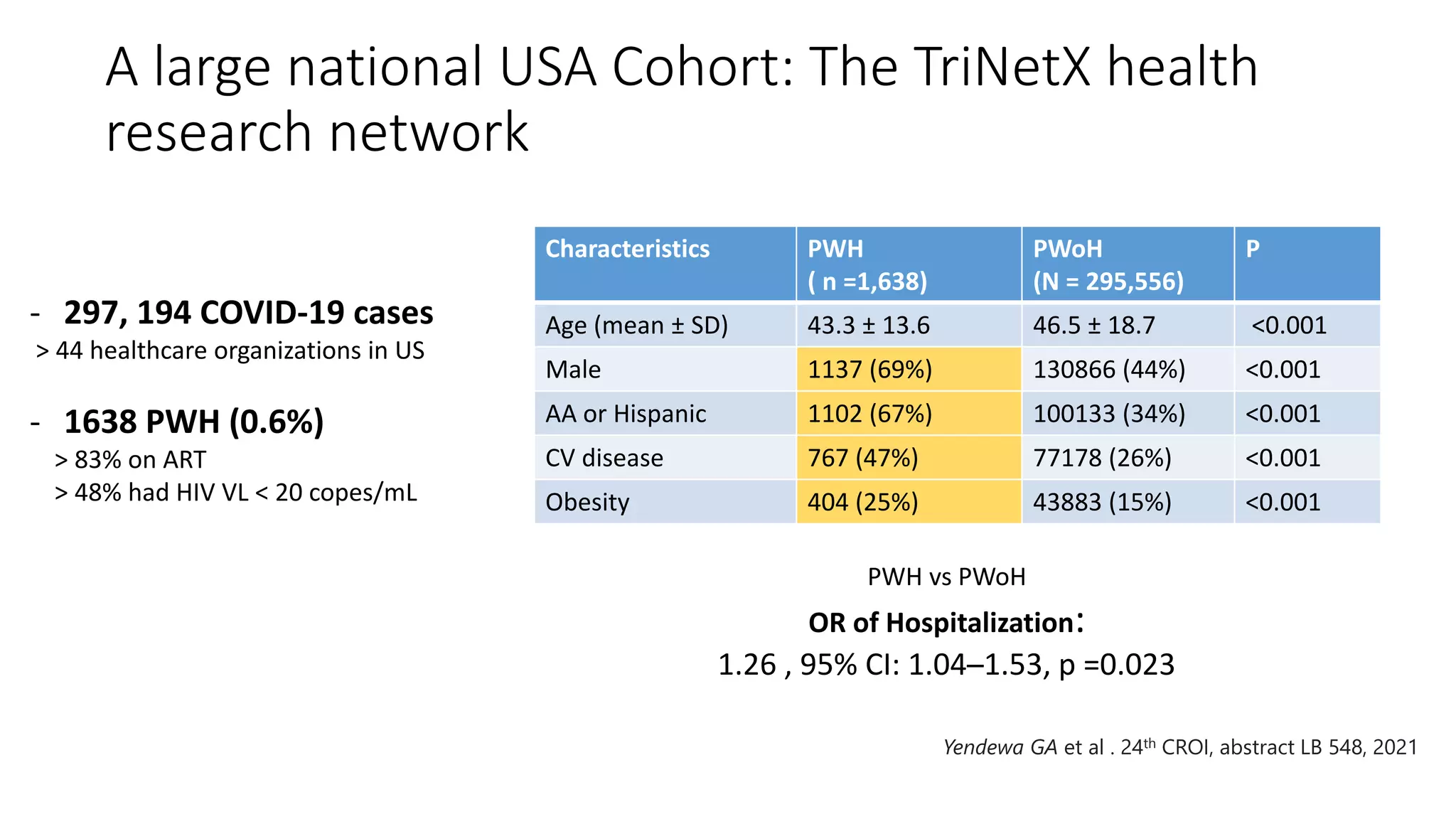
The HIV & Global Health Rounds at UC San Diego present ongoing research on infectious diseases, emphasizing the impact of COVID-19 on individuals living with HIV. Data suggests that people with HIV may have varying rates of COVID-19 acquisition and outcomes, influenced by social disparities and CD4 counts. The document reviews multiple studies illustrating testing rates, susceptibility, and clinical outcomes of people living with HIV in the context of the pandemic.
![PWH, N (%) PWoH, N (%)
At risk patients 108,062 19 345 499
Total diagnosed 2409 (2.2%) 375 260 (1.9%)
Rate per 1000 27.5 19.4
RR: 1.43 [95%CI, 1.38-1.48]
*sRR: 0.94 [95%CI, 0.91-0.97)
* controlling for age, sex, and region
Tesoriero J, et al. JAMA Netw Open. 2021;4(2):e2037069.
Data from Statewide in New York: march 1 to June 7, 2020](https://image.slidesharecdn.com/highrounds20210409ecachay-210614223023/75/04-09-21-Making-Sense-of-the-COVID-19-Data-in-Persons-with-HIV-16-2048.jpg)
![0
10
20
30
40
50
PWH w/COVID-19 PWH w/o COVID-19 PWoH w/ COVID-19
Braunstein SL, et al. Clin Infect Dis. 2020 Nov 30 Epub ahead of print.
New York City: A Population-Level Analysis of Linked Surveillance Data
Black White Very high poverty (≥30% below FPL)*
Hispanic
%
* Less than 28,236$ annually for a 3-member household
N =113 907 N= 202 012
N =2410
31.6%
16.1%
25.1%
aRR, 1.59 [95%CI, 1.40-
1.81])
aRR, 2.08 [95%CI, 1.83-
2.37
March 1 to June 2, 2020
86.4% 78.6%
33%](https://image.slidesharecdn.com/highrounds20210409ecachay-210614223023/75/04-09-21-Making-Sense-of-the-COVID-19-Data-in-Persons-with-HIV-18-2048.jpg)
![Risk of diagnosis using population data from Statewide in
New York: March 1 – June 7, 2020
Population
size
№ Diagnosed Rate per
1000 PWH
Rate ratio (95% CI)
Unadjusted Adjusted
CD4 ≥ 500 63712 1774 27.84 1 [ Reference ] 1 [ Reference ]
CD4: 200-499 27905 843 30.21 1.08 (0.99─1.18) 1.02 (0.94─1.11)
CD4 < 200 7498 270 36.01 1.29 (1.14─1.47) 1.22 (1.07─1.38)
Other 8947 101 11.29 NA NA
Viral Suppression*
Yes 87 480 2628 30.04 1 [ Reference ] NA
No 12 027 267 22.20 0.74 (0.65─0.84) NA
Other 8555 93 10.87 NA NA
Tesoriero J, et al. JAMA Netw Open. 2021;4(2):e2037069.
* HIV VL < 200 copies/mL
Model adjusted for age, sex, race/ethnicity, HIV
transmission risk , region of residence.](https://image.slidesharecdn.com/highrounds20210409ecachay-210614223023/75/04-09-21-Making-Sense-of-the-COVID-19-Data-in-Persons-with-HIV-23-2048.jpg)
![Summary of 1st wave of studies: No worse outcomes
Time Region Design Setting Number Hospitalized ICU Died VL <
200
CD4<
200
Comment Reference
3/30 ─ 5/20 /20 Rhode Island,
US
Case series Inpt/outp 27 9/27 (33%) 0 1* ALL 1 19 of 27 non-white JIAC 2020,
23:e25573
2/2─ 4/16/20 Milan, Italy Case series Inpt/outp 47 13/47 (28%) 2 2** 44 of 47 0 Good outcome CID 2020;71:2276–
8
3/11─4/17/20 Munich,
Germany
Cases series Inpt/outp 33 14/33 (42%) 6 3 30 of 32 1 Infection (2020)
48:681–686
3/15─4/15/20 New York, USA Case series Inpatient 31 4 8 (25.8%) ALL 7 ¾ non-whites CID 2020 1:2294–7
2/1─ 4/30/20 Madrid, Spain Cohort Inpt/oupt 51
1.8% (95% CI 1.3–2.3)
28 6 (12%) 2 (4%) ALL 6 follow-up qualitative
RT-PCR assays
Lancet HIV.
2020;7:e554-564.
3/10─5/11/20 New York, USA Cohort Inpatient 4613
(100 HIV+)
ALL HR 1.73
[95% CI:
1.12 to 2.67]
HIV+:22%
HIV-: 24%)
81 of 90 2/3 non-white
No deaths among
PWH w/ VL > 200
JAIDS. 2021
1;86:224-230
3/4─4/3/20 New York, USA Matched
control (1:2)
Inpatient HIV+ 21
HIV- 42
ALL 6 (28.6%)
7 (16.7%)
6 (28.6%)
10 (23.8%)
20 0f 21 1 HIV+ had more non-
white
JAIDS, 2020;85:6-
10.
3/10─5/15/20 New York, USA Matched
control (1:2)
Inpatient HIV+ 30
HIV- 90
ALL HIV+ 4 (13%)
HIV-21 (23%)
HIV+ 2(7%)
HIV-14(16%)
ALL 7 ¾ non-white OFID. 2020
1;7(8):ofaa327
3/12─4/23/2 New York, USA Matched
control (1:5)
Inpatient 88 HIV+
405 HIV-
ALL HIV+ 18%
HIV- 23%
HIV+ 21%
HIV - 20%
66 7 ¾ non white CID 2020;71:2933-
2293
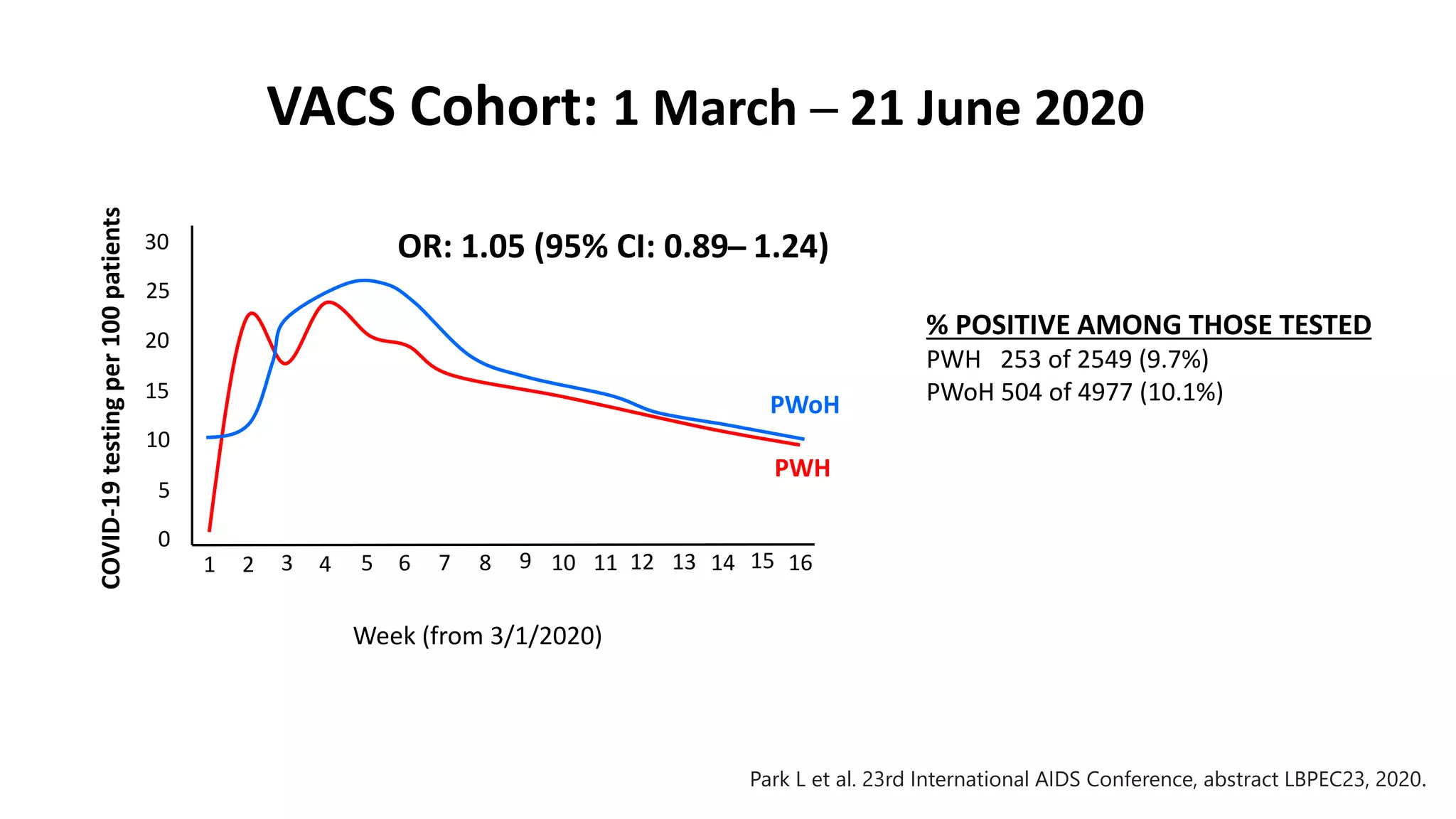
3/1─6/21/20 USA (VACS) Matched
control (1:2)
Inpt/outp POSITIVE
HIV+ 253
HIV- 504
HIV+ 86(35%)
HIV- 178 (35%)
HIV+ 35(14%)
HIV- 75 (25%)
HIV+ 24(10%)
HIV- 56 (11%)
More testing but no
increased positivity
Park L et al.
IAC2020
Cachay et al. In Progress](https://image.slidesharecdn.com/highrounds20210409ecachay-210614223023/75/04-09-21-Making-Sense-of-the-COVID-19-Data-in-Persons-with-HIV-27-2048.jpg)
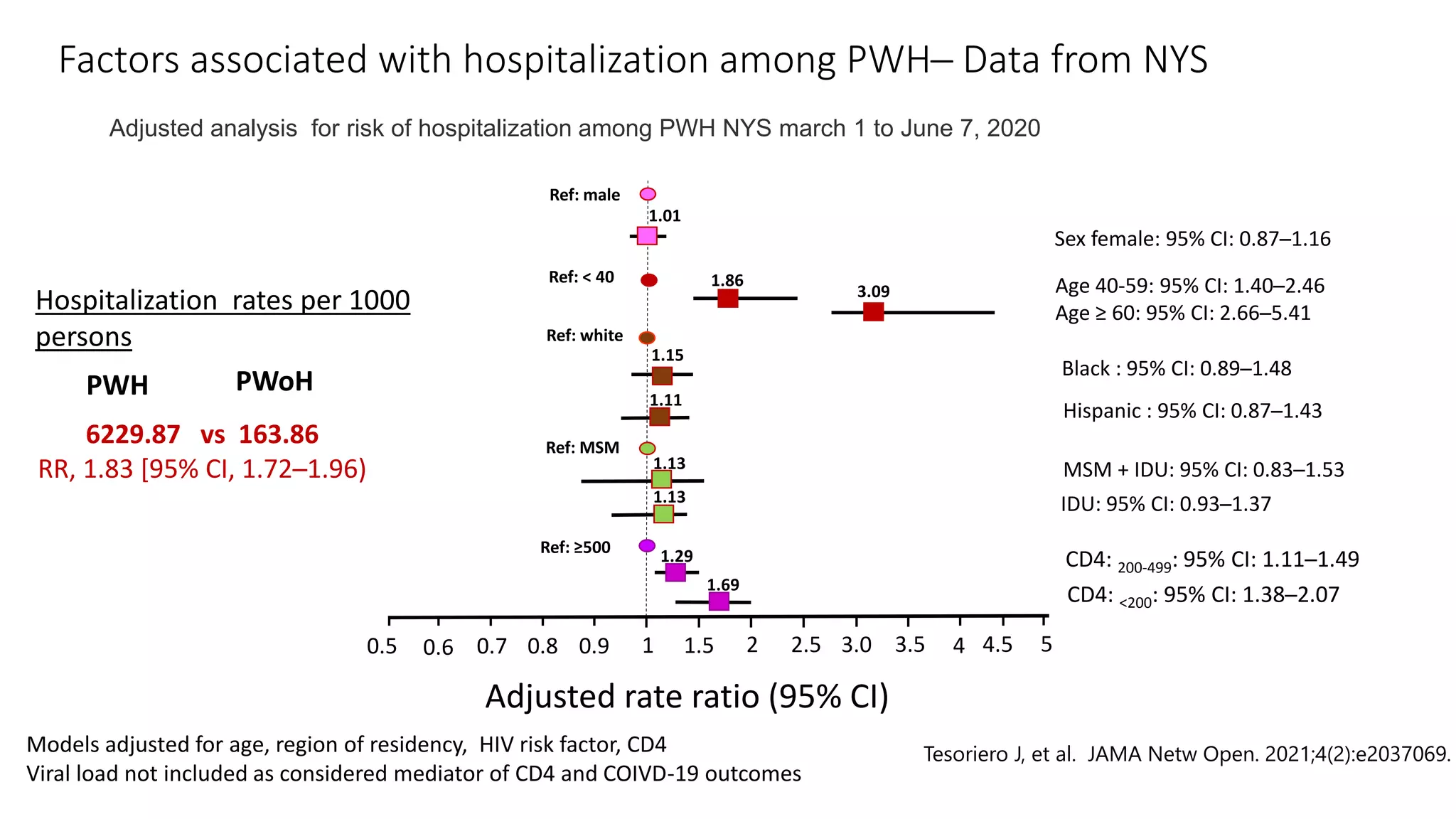
![Population
size
№ Rate per
1000 diagnoses
Rate ratio (95% CI)
Unadjusted Adjusted
HIV suppressed 87480 756 287.7 1 [Reference] NA
HIV unsuppressed 12027 105 393.3 1.37 (1.11─1.68) NA
Other 8555 35 376.3 NA NA
CD4≥500 63712 437 246.3 1 [ Reference ] 1 [ Reference ]
CD4: 200-499 27905 298 353.5 1.44 (1.24─1.66) 1.29 (1.11─1.49)
CD4<200 7498 126 466.7 1.89 (1.55─2.31) 1.69 (1.38─2.07)
Risk of hospitalization using population data from
Statewide in New York: March 1 – June 7, 2020
Tesoriero J, et al. JAMA Netw Open. 2021;4(2):e2037069.
Model adjusted for age, sex, race/ethnicity, HIV transmission risk , region of residence](https://image.slidesharecdn.com/highrounds20210409ecachay-210614223023/75/04-09-21-Making-Sense-of-the-COVID-19-Data-in-Persons-with-HIV-34-2048.jpg)