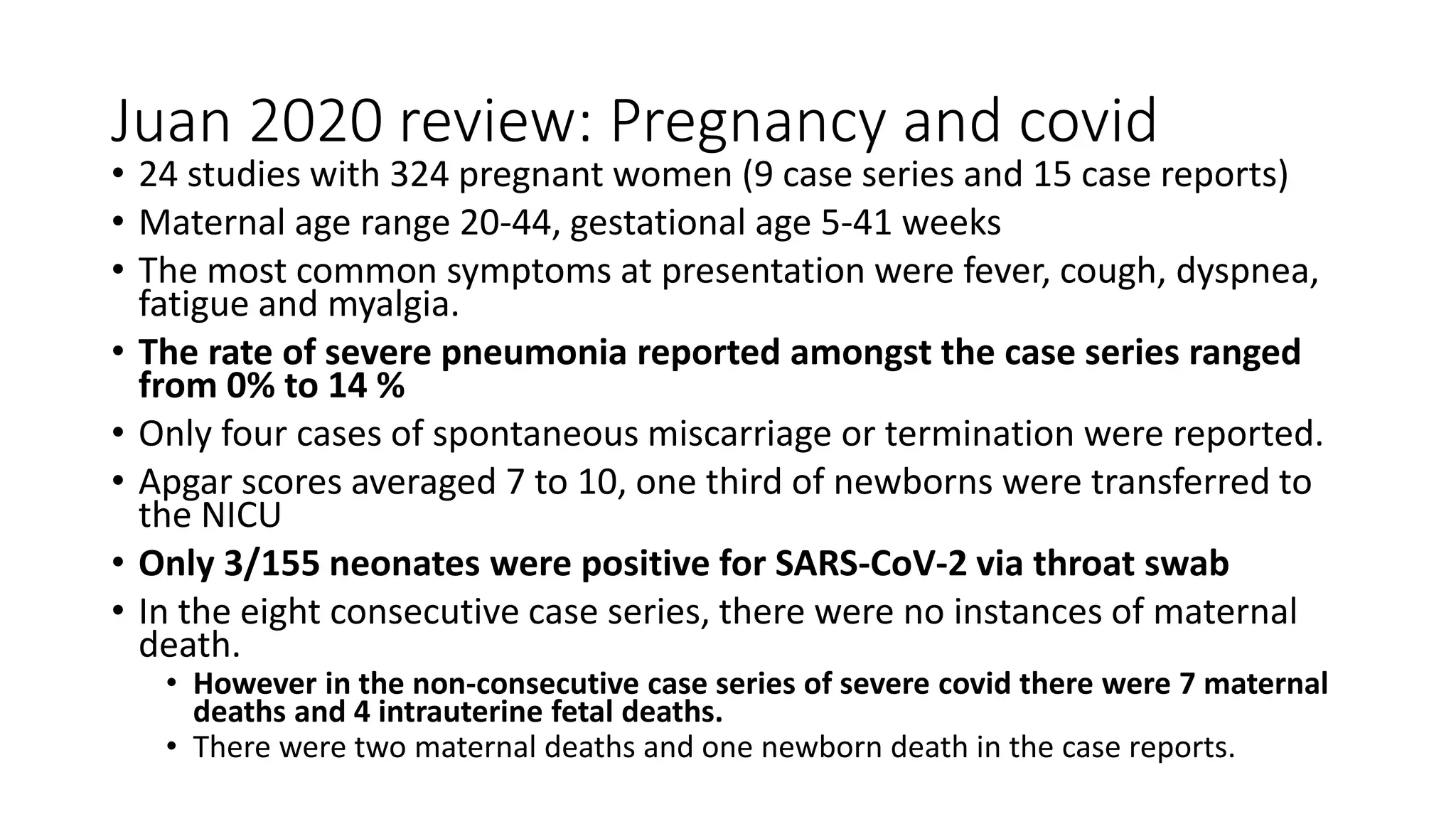
The document discusses the UC San Diego Antiviral Research Center's weekly presentations on HIV and other infectious diseases, focusing on a session about COVID-19 in pregnancy. It outlines physiological and immune system changes in pregnant women, the implications of COVID-19 on maternal health, and treatment considerations. Key findings indicate a low rate of vertical transmission but highlight increased risks associated with severe COVID-19 in pregnant patients.













![MMWR published June 2020 (Ellington 2020)
• January 22-June 7, as part of COVID-19 surveillance, CDC identified 8,207 pregnant
patients that they were able to obtain health information on
• Pregnant and non-pregnant cohorts reported similar frequencies of cough (>50%) and
shortness of breath (30%),
• Though pregnant women had fewer HA, myalgia's, fevers/chills and diarrhea
• (31.5%) of pregnant women with COVID-19 were hospitalized compared with 5.8% of
nonpregnant women.
• “After adjusting for age, presence of underlying medical conditions, and race/ethnicity,
pregnant women were significantly more likely to be admitted to the intensive care unit
(ICU) (aRR = 1.5, 95% confidence interval [CI] = 1.2-1.8) and receive mechanical
ventilation (aRR = 1.7, 95% CI = 1.2-2.4)."
• “Sixteen (0.2%) COVID-19-related deaths were reported among pregnant, and 208
(0.2%) such deaths were reported among nonpregnant women (aRR = 0.9, 95% CI = 0.5-
1.5)”.
• Mortality appears similar with pregnant vs non-pregnant women, however pregnant
women are more likely to require ICU stays and intubations](https://image.slidesharecdn.com/highrounds20210205jkeehner-210614222442/75/02-05-21-COVID-19-and-Pregnancy-17-2048.jpg)











![references
• Soma-Pillay P, Nelson-Piercy C, Tolppanen H, Mebazaa A. Physiological changes in pregnancy. Cardiovasc J Afr. 2016;27(2):89-94. doi:10.5830/CVJA-2016-021
• Cornish EF, Filipovic I, Åsenius F, Williams DJ, McDonnell T. Innate Immune Responses to Acute Viral Infection During Pregnancy. Front Immunol. 2020;11:572567. Published 2020 Sep 30. doi:10.3389/fimmu.2020.572567
• Thornton JG. COVID-19 in pregnancy. BJOG. 2020 Aug;127(9):1122. doi: 10.1111/1471-0528.16308. Epub 2020 Jun 4. PMID: 32378774.
• Ferrazzi E, Frigerio L, Savasi V, Vergani P, Prefumo F, Barresi S, Bianchi S, Ciriello E, Facchinetti F, Gervasi MT, Iurlaro E, Kustermann A, Mangili G, Mosca F, Patanè L, Spazzini D, Spinillo A, Trojano G, Vignali M, Villa A, Zuccotti GV, Parazzini F, Cetin I. Vaginal delivery in SARS-CoV-2-
infected pregnant women in Northern Italy: a retrospective analysis. BJOG. 2020 Aug;127(9):1116-1121. doi: 10.1111/1471-0528.16278. Epub 2020 May 28. PMID: 32339382; PMCID: PMC7267664.
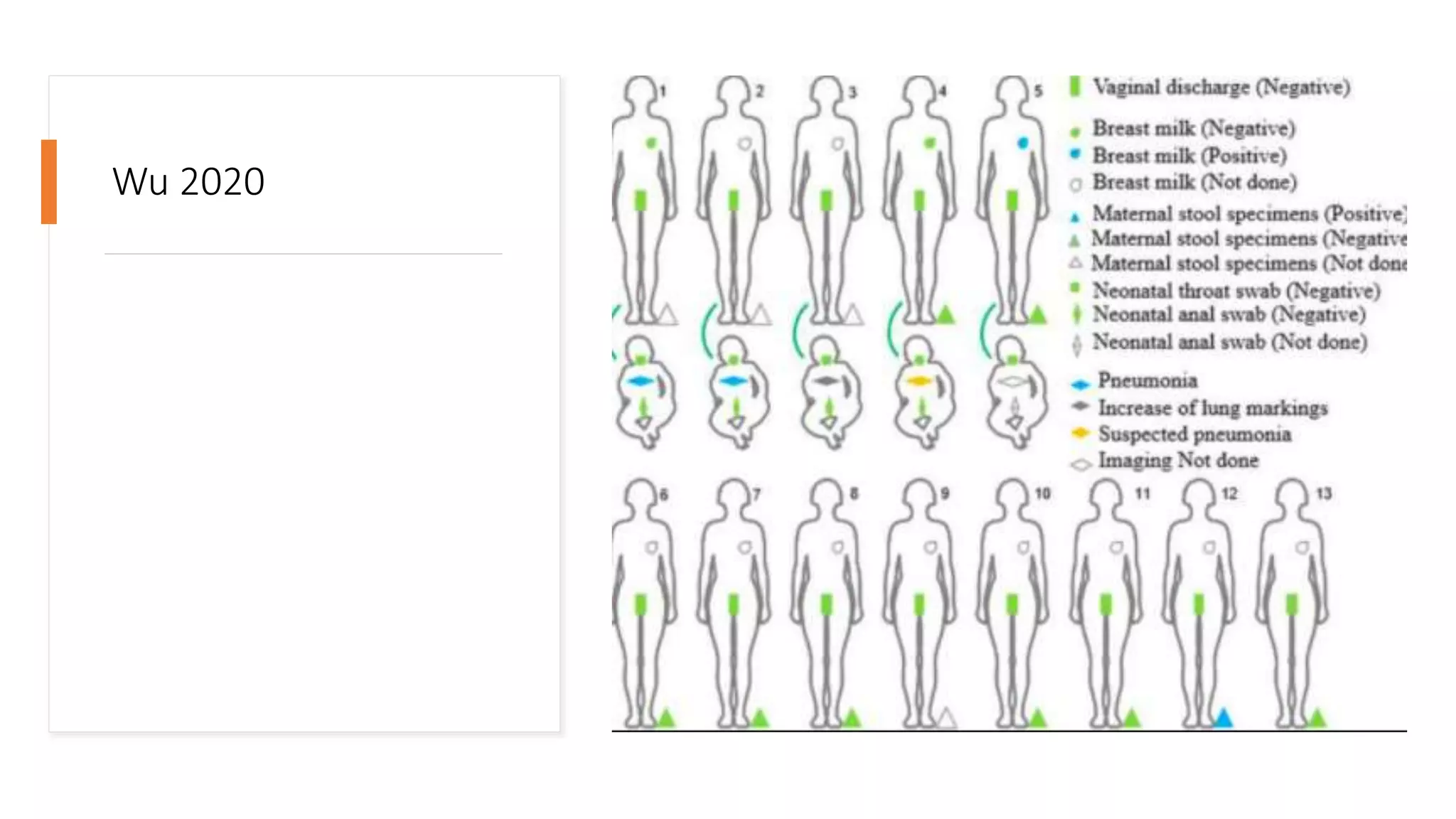
• Wu Y, Liu C, Dong L, Zhang C, Chen Y, Liu J, Zhang C, Duan C, Zhang H, Mol BW, Dennis CL, Yin T, Yang J, Huang H. Coronavirus disease 2019 among pregnant Chinese women: case series data on the safety of vaginal birth and breastfeeding. BJOG. 2020 Aug;127(9):1109-1115. doi:
10.1111/1471-0528.16276. Epub 2020 May 26. PMID: 32369656; PMCID: PMC7383704.
• Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet Gynecol. 2020;56(1):15-27. doi:10.1002/uog.22088
• Metz, Torri “Maternal and neonatal outcomes of pregnant patients with coronavirus disease 2019 (COVID-19): A multistate cohort” Jan 28,2021 Society of maternal Fetal medicine
• Wastnedge EAN, Reynolds RM, van Boeckel SR, Stock SJ, Denison FC, Maybin JA, Critchley HOD. Pregnancy and COVID-19. Physiol Rev. 2021 Jan 1;101(1):303-318. doi: 10.1152/physrev.00024.2020. Epub 2020 Sep 24. PMID: 32969772; PMCID: PMC7686875.
• Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, Nahabedian J, Anderson K, Gilboa SM. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status - United States, January 22-June 7, 2020. MMWR
Morb Mortal Wkly Rep. 2020 Jun 26;69(25):769-775. doi: 10.15585/mmwr.mm6925a1. PMID: 32584795; PMCID: PMC7316319.
• Takemoto MLS, Menezes MO, Andreucci CB, Nakamura-Pereira M, Amorim MMR, Katz L, Knobel R. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int J Gynaecol Obstet ijgo.13300, 2020. doi:10.1002/ijgo.13300
• Berger Abi. Th1 and Th2 responses: what are they? BMJ 2000; 321 :424
• Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, O'Brien P, Quigley M, Brocklehurst P, Kurinczuk JJ; UK Obstetric Surveillance System SARS-CoV-2 Infection in Pregnancy Collaborative Group. Characteristics and outcomes of pregnant women admitted to hospital with
confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020 Jun 8;369:m2107. doi: 10.1136/bmj.m2107. PMID: 32513659; PMCID: PMC7277610.
• Ji HL, Zhao R, Matalon S, Matthay MA. Elevated Plasmin(ogen) as a Common Risk Factor for COVID-19 Susceptibility. Physiol Rev. 2020 Jul 1;100(3):1065-1075. doi: 10.1152/physrev.00013.2020. Epub 2020 Mar 27. PMID: 32216698; PMCID: PMC7191627.
• “Special Considerations in Pregnancy” https://www.covid19treatmentguidelines.nih.gov/special-populations/pregnancy/
• Naqvi M, Zakowski P, Glucksman L, Smithson S, Burwick RM. Tocilizumab and Remdesivir in a Pregnant Patient With Coronavirus Disease 2019 (COVID-19). Obstet Gynecol. 2020 Nov;136(5):1025-1029. doi: 10.1097/AOG.0000000000004050. PMID: 32618794.
• Favilli A, Mattei Gentili M, Raspa F, et al. Effectiveness and safety of available treatments for COVID-19 during pregnancy: a critical review [published online ahead of print, 2020 Jun 7]. J Matern Fetal Neonatal Med. 2020;1-14. doi:10.1080/14767058.2020.1774875
• Shanes ED. Placental pathology in COVID-19 (Preprint). MedRxiv 20093229, 2020. doi:10.1101/2020.05.08.20093229.
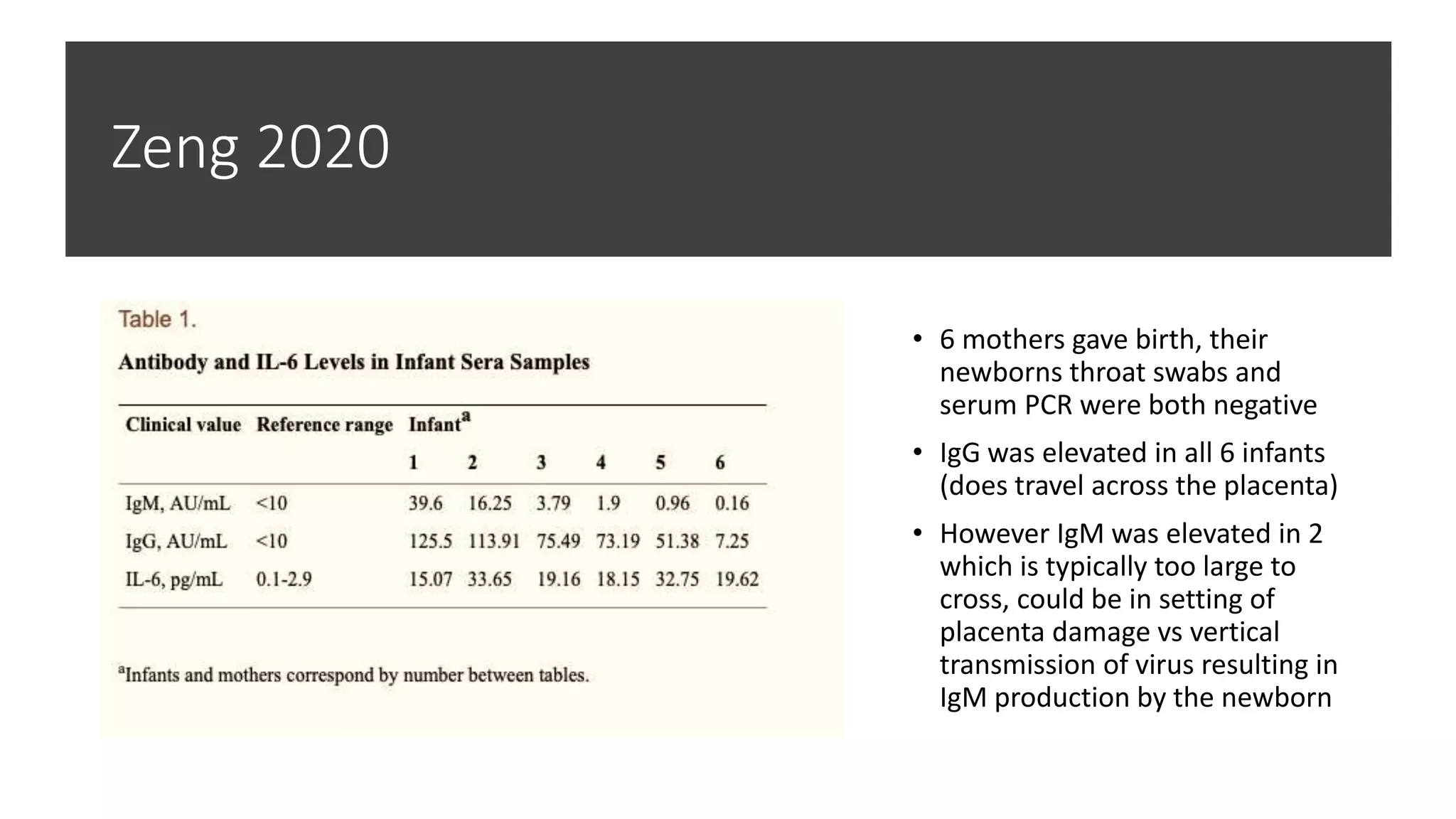
• Antibodies in Infants Born to Mothers With COVID-19 Pneumonia.Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, Long XJAMA. 2020 May 12; 323(18):1848-1849.
• Hoeltzenbein M, Beck E, Rajwanshi R, Gøtestam Skorpen C, Berber E, Schaefer C, Østensen M. Tocilizumab use in pregnancy: Analysis of a global safety database including data from clinical trials and post-marketing data. Semin Arthritis Rheum. 2016 Oct;46(2):238-245. doi:
10.1016/j.semarthrit.2016.05.004. Epub 2016 May 25. PMID: 27346577.
• Adhikari EH, Moreno W, Zofkie AC, et al. Pregnancy Outcomes Among Women With and Without Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Netw Open. 2020;3(11):e2029256. Published 2020 Nov 2. doi:10.1001/jamanetworkopen.2020.29256
• https://www.covid19treatmentguidelines.nih.gov/statement-on-casirivimab-plus-imdevimab-eua/
• https://www.covid19treatmentguidelines.nih.gov/statement-on-bamlanivimab-eua/](https://image.slidesharecdn.com/highrounds20210205jkeehner-210614222442/75/02-05-21-COVID-19-and-Pregnancy-31-2048.jpg)