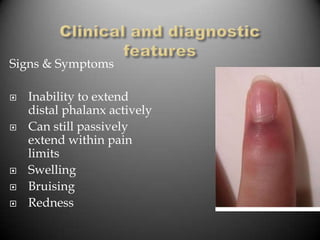
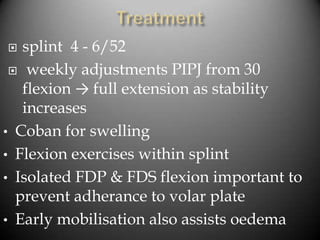
This document provides information on various hand conditions including trigger finger/thumb, De Quervain's tenosynovitis, mallet finger, PIP joint dislocations, and Dupuytren's disease. It describes the presentation, typical mechanisms of injury, conservative and surgical treatment approaches for each condition. The key points are that splinting and injections are usually first-line treatments while surgery is reserved for cases that fail conservative care or have more significant injuries/deformities.