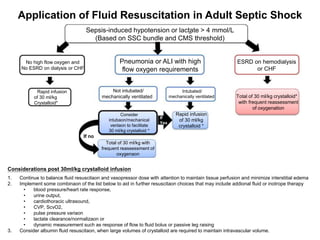
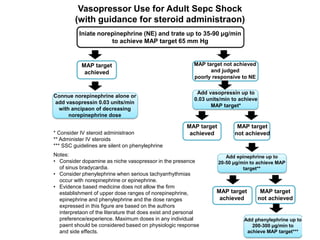
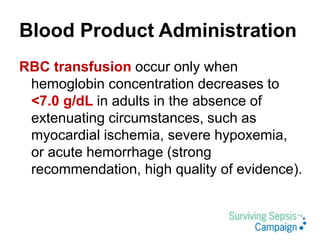
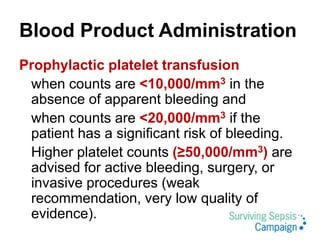
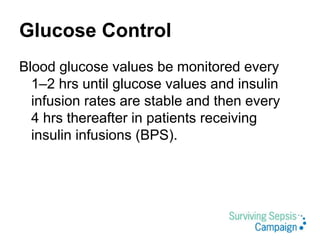
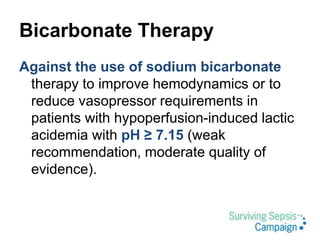
This document summarizes the 2016 guidelines from the Surviving Sepsis Campaign for the management of severe sepsis and septic shock. It outlines recommendations for initial resuscitation with IV fluids, vasopressors, corticosteroids, antibiotics, source control, blood products, glucose control, and bicarbonate therapy. The guidelines emphasize early recognition and treatment, with IV fluids, broad-spectrum antibiotics within 1 hour, and measuring lactate and targeting MAP of 65 mmHg as priorities in initial resuscitation of sepsis and septic shock.