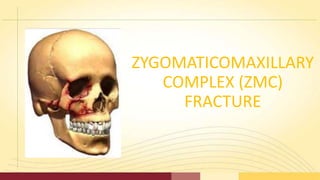
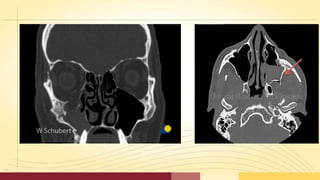
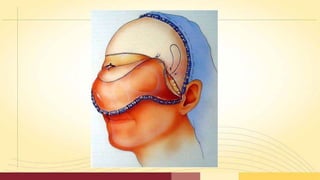
Zygomaticomaxillary complex (ZMC) fractures are the second most common facial fractures. They involve fractures of the zygomatic bone and its articulations with the maxilla, sphenoid, frontal, and temporal bones. Clinical signs include deformity of the zygomatic arch and orbital region, trismus, abnormal sensation, and epistaxis. Radiographic evaluation with CT scanning is important for classification and treatment planning. Treatment options include indirect reduction without fixation, indirect reduction with temporary packing, and direct open reduction with fixation when instability remains. Approaches for reduction include temporal, intraoral, percutaneous, transantral, and lateral brow incisions.