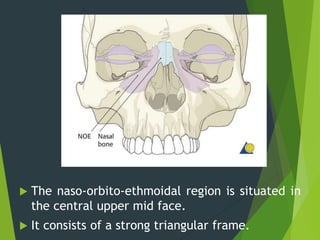
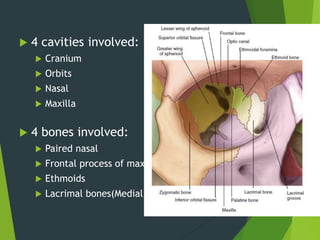
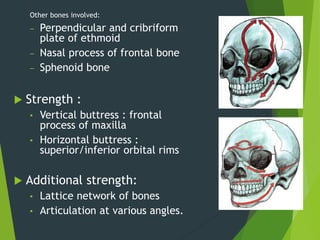
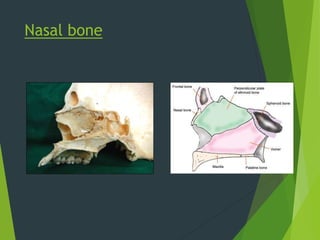
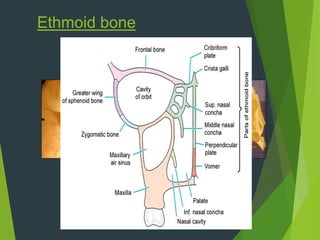
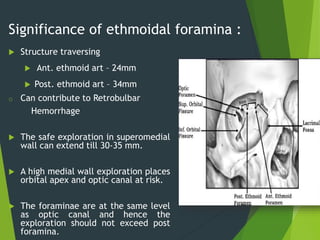
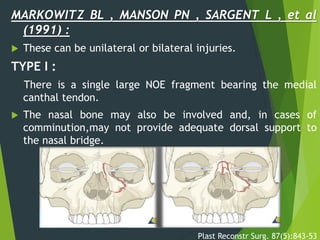
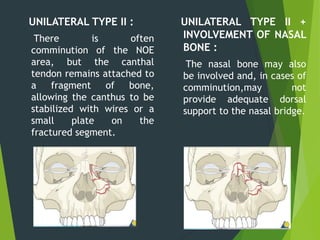
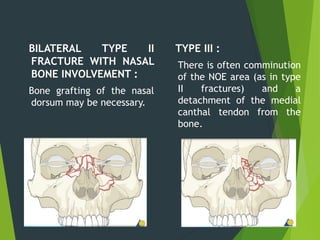
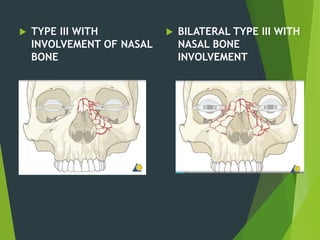
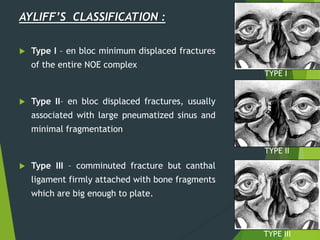
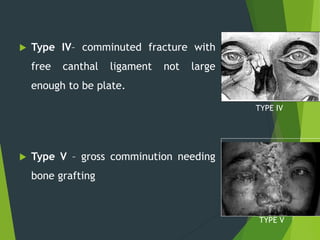
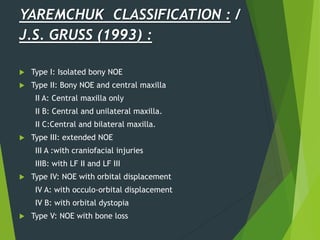
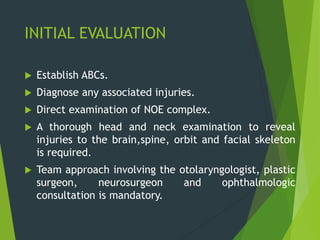
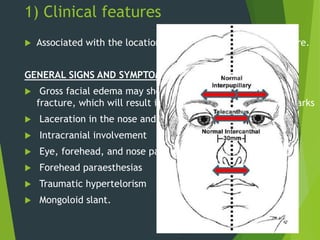
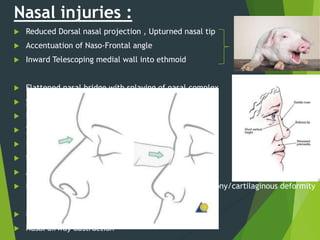
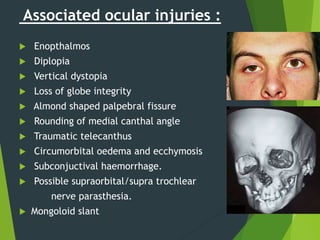
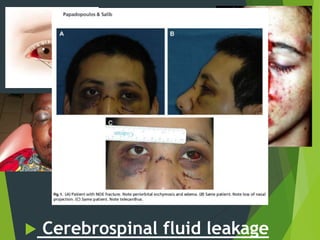
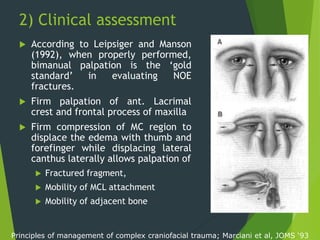
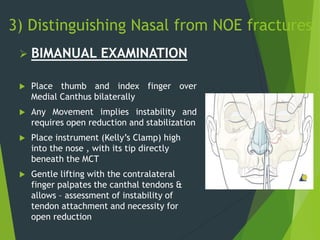
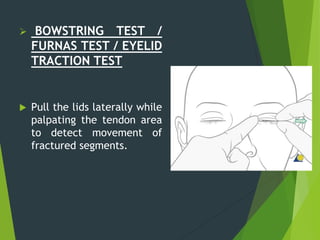
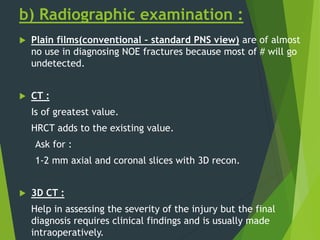
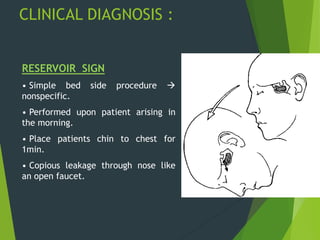
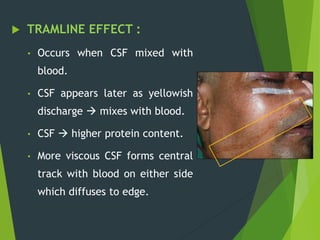
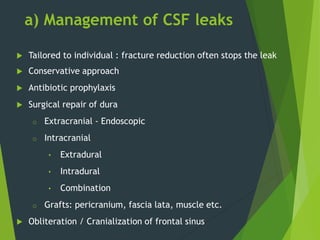
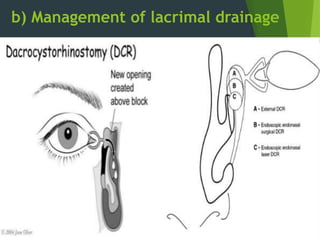
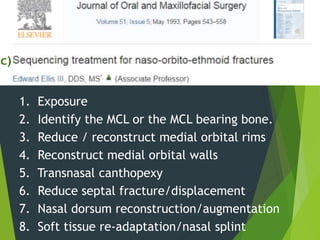
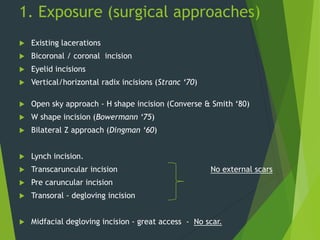
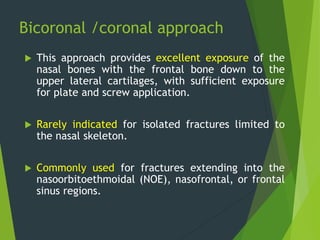
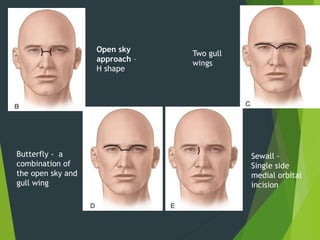
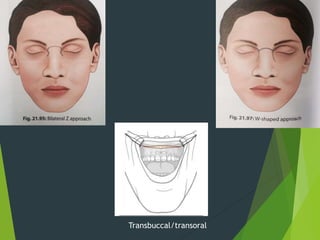
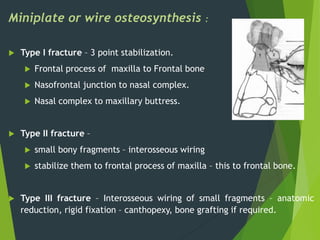
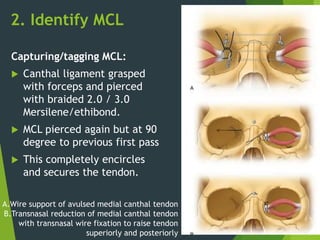
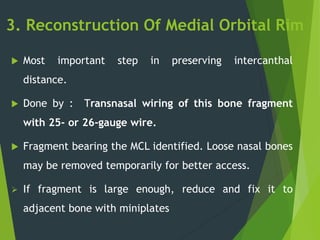
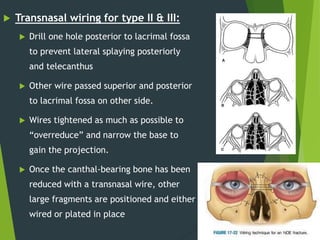
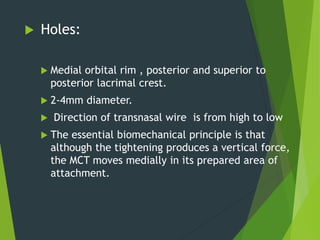
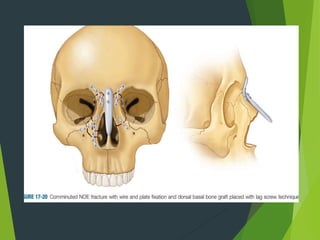
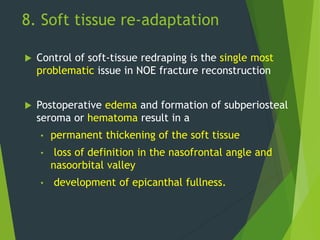
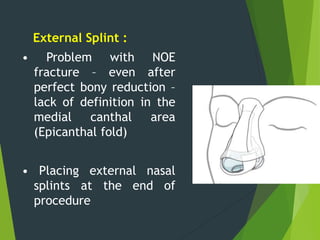
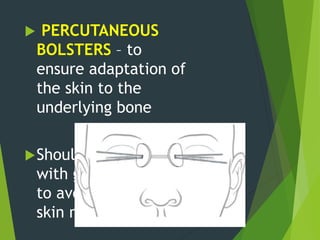
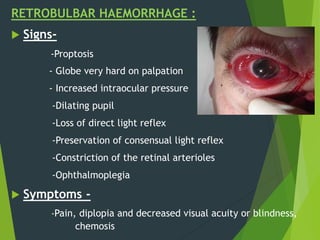
The document discusses naso-orbito-ethmoidal (NOE) fractures, their anatomy, classification, diagnosis, and treatment. NOE fractures are a spectrum of injuries involving the nose, orbits, and adjacent structures, and they can lead to various complications, including cerebrospinal fluid leaks and associated non-facial injuries. The document emphasizes the importance of a multidisciplinary approach for diagnosis and management, highlighting both open and closed treatment techniques to ensure effective care.