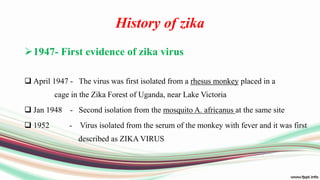
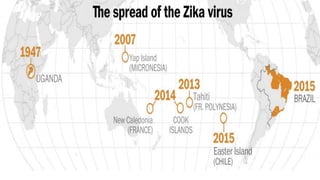
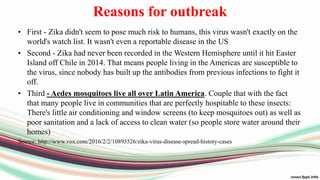
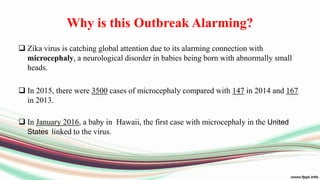
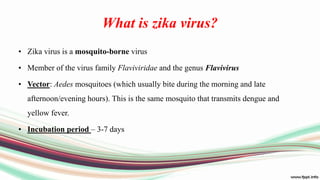
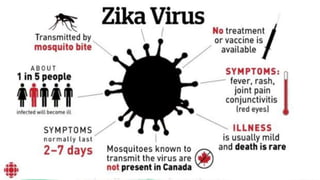
Zika virus was first isolated in 1947 in Uganda. It spread from Africa to Asia between 1951-1981 and caused its first outbreak outside of Africa and Asia on Yap Island in 2007. In 2015, Zika virus emerged in Brazil and has since spread across South and Central America. The main reasons for the outbreak in the Americas include lack of prior exposure or immunity, presence of the Aedes mosquito vector, and living conditions conducive to mosquito breeding. Zika virus is alarming due to its association with microcephaly in babies born to infected mothers and the lack of vaccines or treatments.