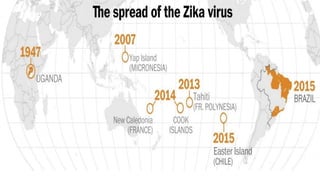
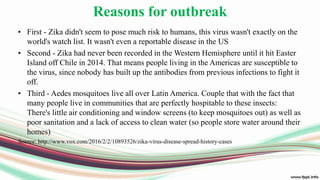
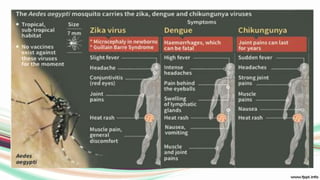
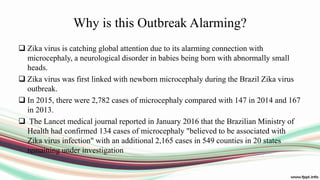
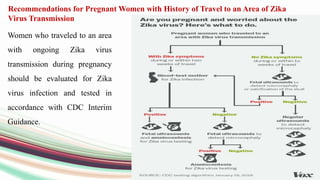
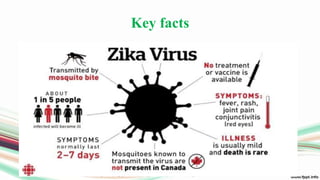
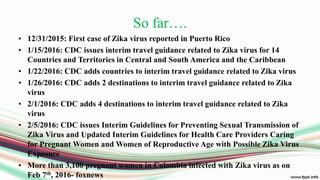
Zika virus is an emerging mosquito-borne virus that is causing an alarming outbreak. It is transmitted primarily through the bite of infected Aedes mosquitoes. The current outbreak in Brazil is alarming because it is linked to a surge in microcephaly cases in newborns. Pregnant women are advised to avoid travel to affected areas due to the risk of maternal-fetal transmission and potential birth defects. Public health officials are working to understand and contain the outbreak.