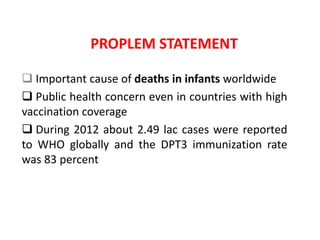
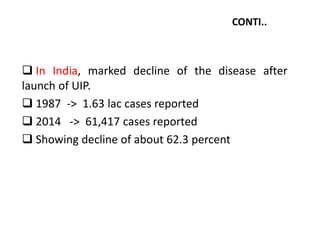
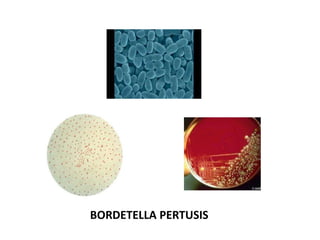
Whooping cough is an infectious disease caused by the Bordetella pertussis bacterium. It is characterized by severe coughing fits that end in a "whooping" sound. It mainly affects young children and can be serious, even life-threatening, especially in infants. Vaccination is the most effective way to prevent whooping cough through active immunization with the DPT vaccine according to national immunization schedules.