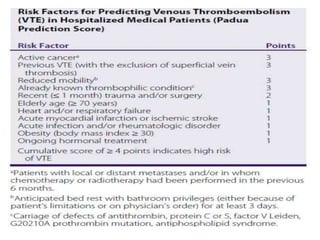
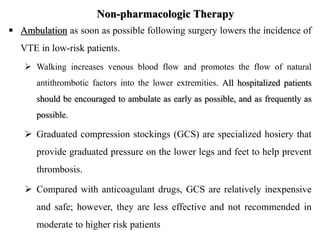
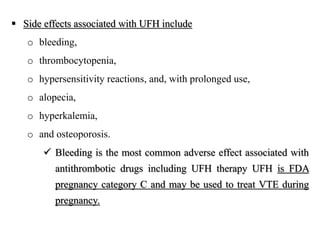
Venous thromboembolism (VTE) manifests as deep vein thrombosis (DVT) or pulmonary embolism (PE) from thrombus formation in the venous circulation. Risk factors include immobilization, surgery, trauma, cancer, and genetic hypercoagulable states. Symptoms are nonspecific so objective tests like ultrasound or CT scan are needed to diagnose. Prevention involves pharmacologic methods like blood thinners or compression stockings, and non-pharmacologic methods like early ambulation. Treatment consists of acute blood thinners followed by long-term oral anticoagulants to prevent recurrence, with duration depending on provoking factors.






![Laboratory Tests
The initial laboratory evaluation should include complete
blood count (CBC) with differential, coagulation studies (such
as prothrombin time [PT]/international normalized ratio [INR],
activated partial thromboplastin time [aPTT]), serum
chemistries with renal and liver function.
Serum concentrations of D-dimer, a by-product of thrombin
generation, will be elevated in an acute event.
A negative D-dimer in a patient with low clinical
probability of DVT can be used to rule out DVT.](https://image.slidesharecdn.com/thrombosis-1-221224223229-84905763/85/Thrombosis-1-pptx-8-320.jpg)