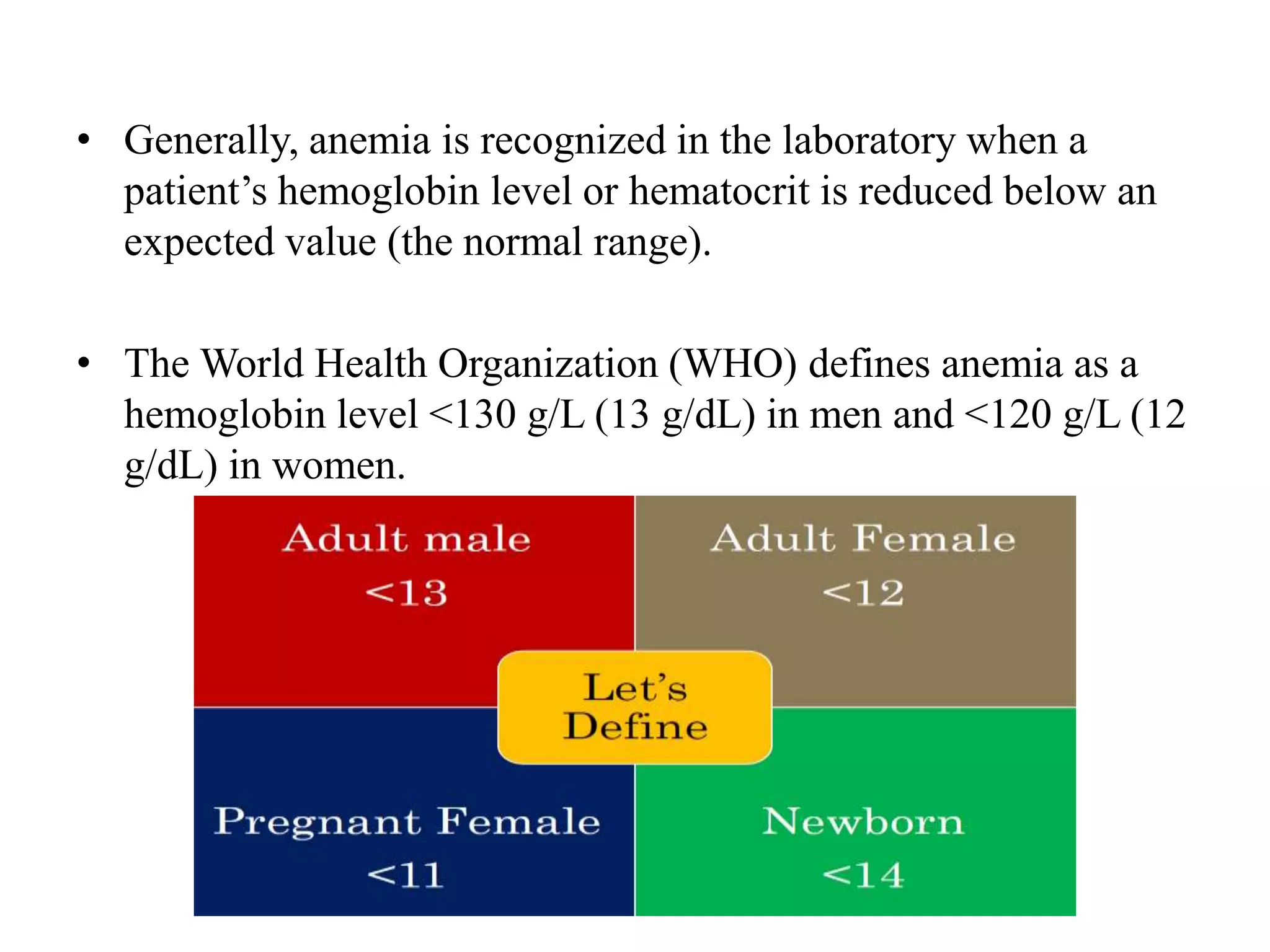
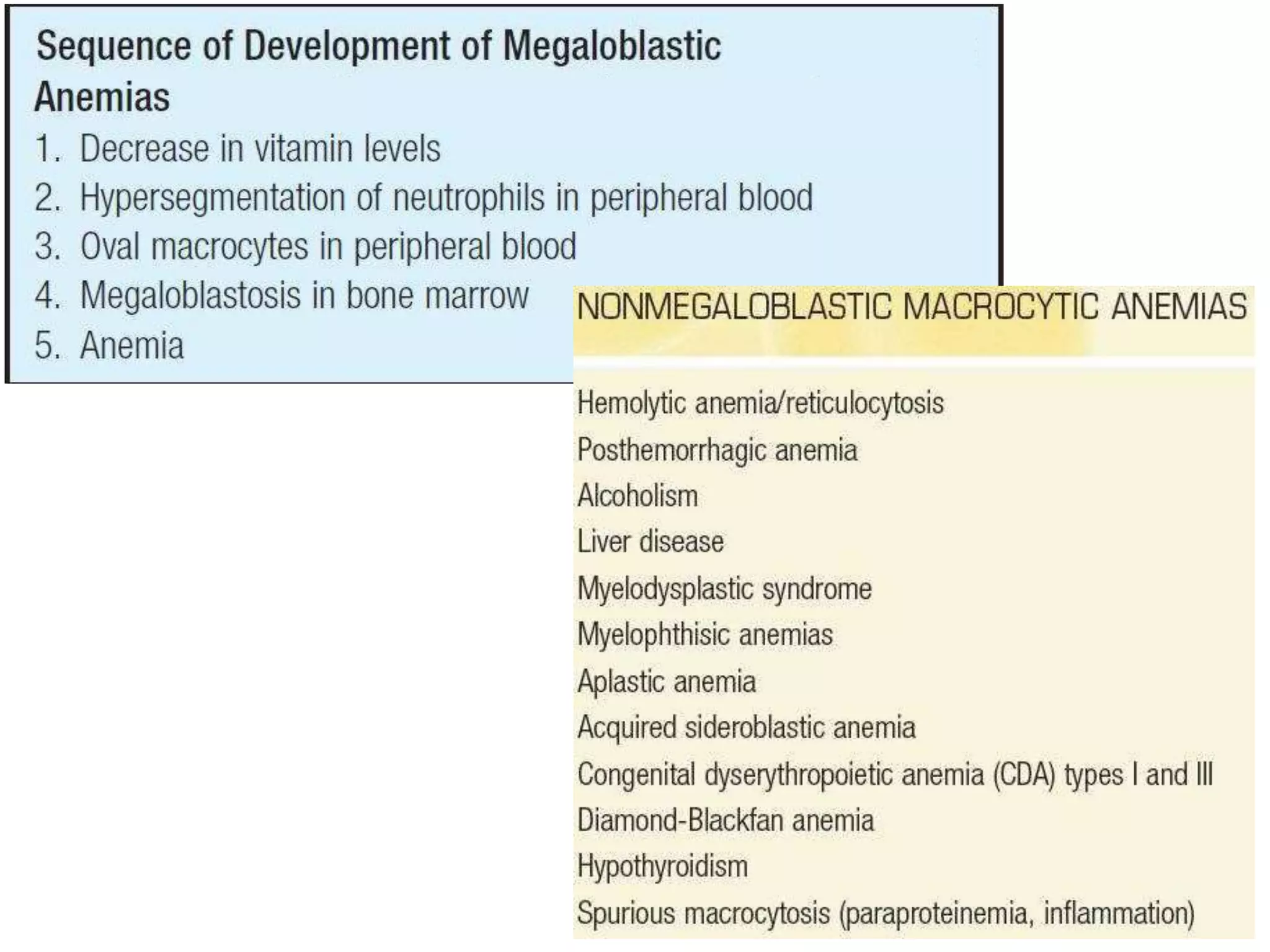
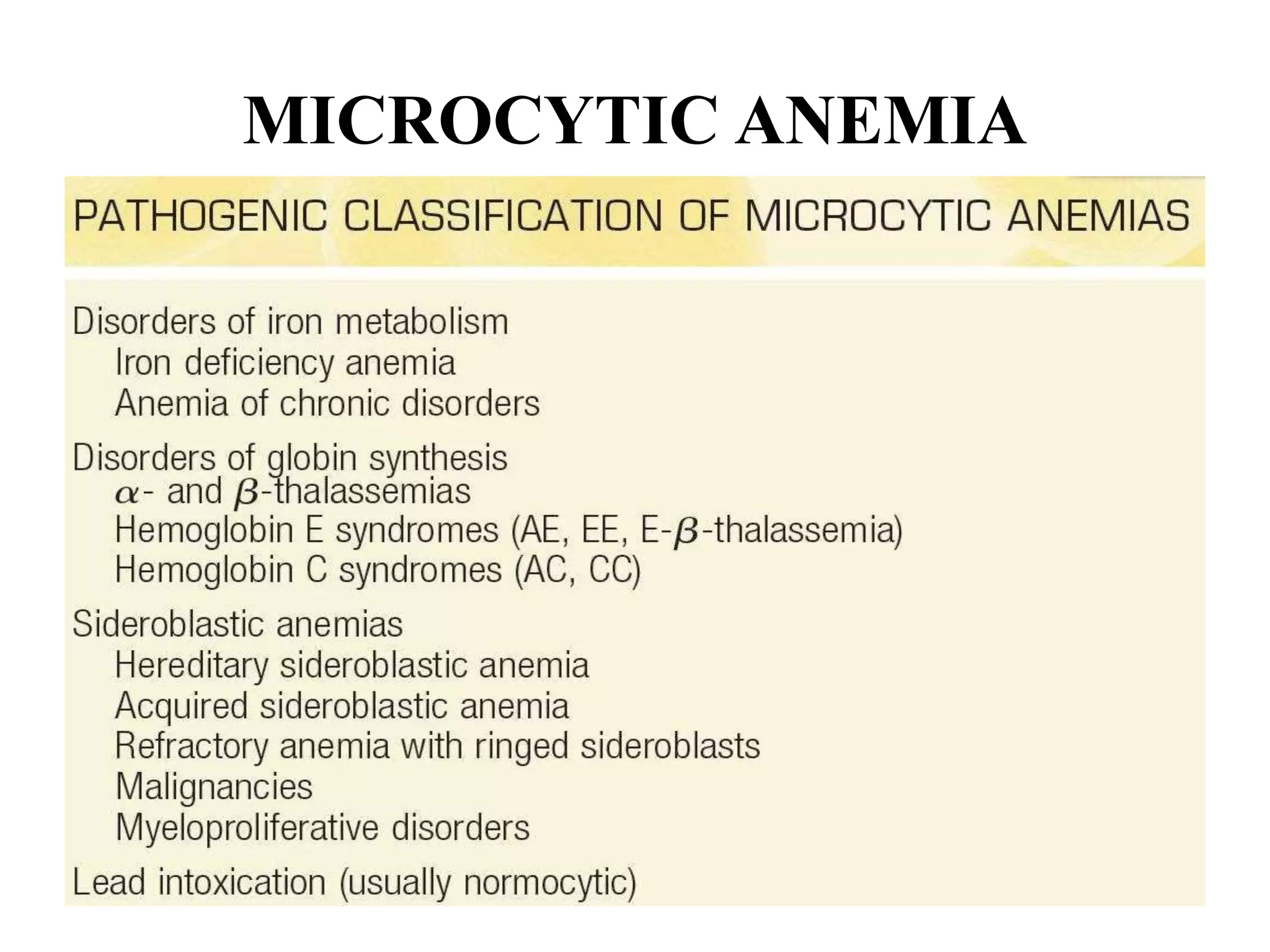
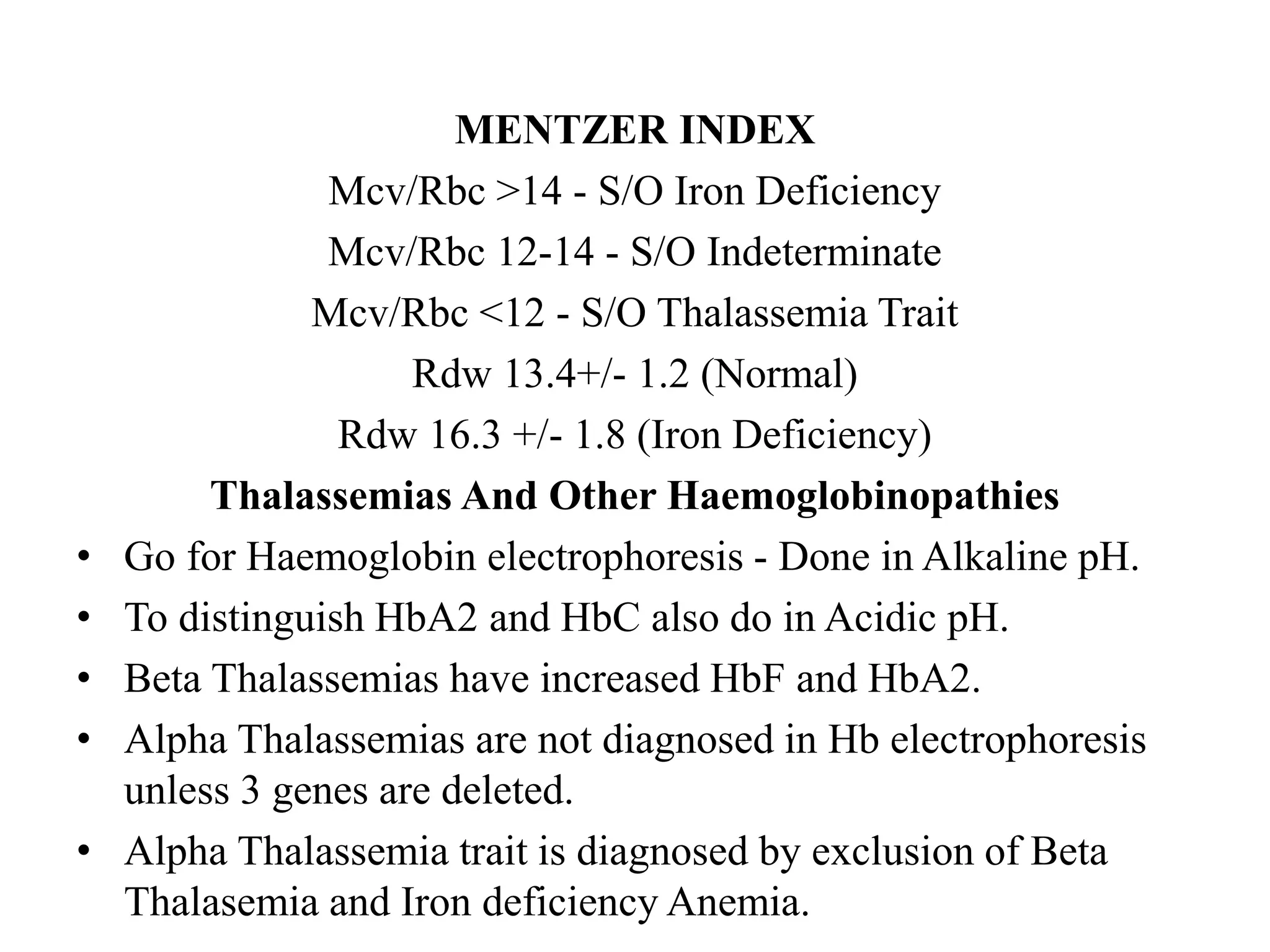
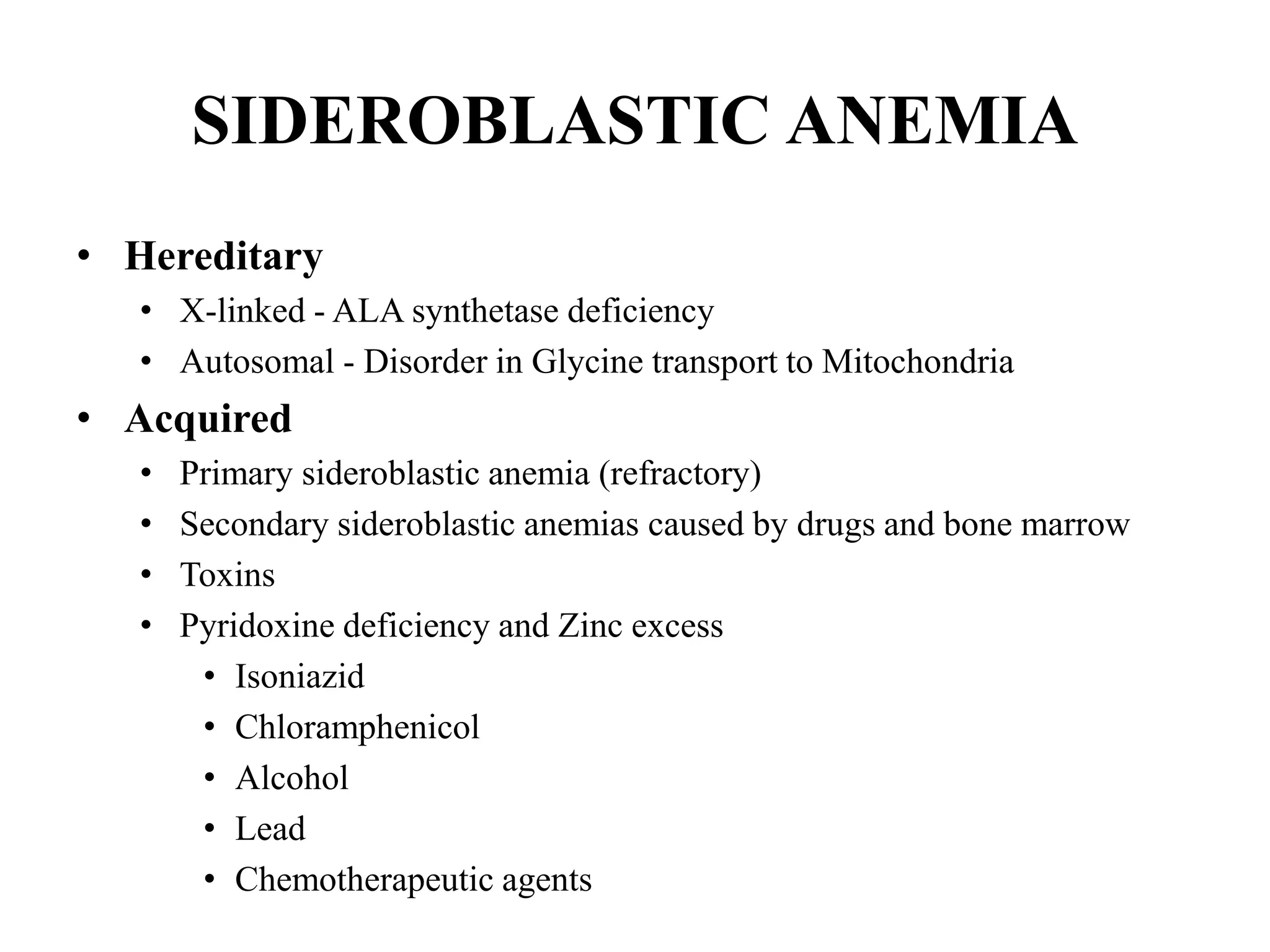
This case involves a 12-year-old female presenting with weakness, lethargy, and inability to work for 2 months. She had her first menstrual period last month that lasted 20 days and is currently having heavy bleeding on her 15th day of this period. On examination, she has pallor and a heart murmur. Laboratory tests show microcytic anemia. The presentation is suggestive of iron deficiency anemia likely due to heavy menstrual bleeding given her family history of menorrhagia. Further workup is needed to confirm the etiology and guide treatment.




























![• Anemia associated with
appropriately increased
erythrocyte production
• Posthemorrhagic anemia
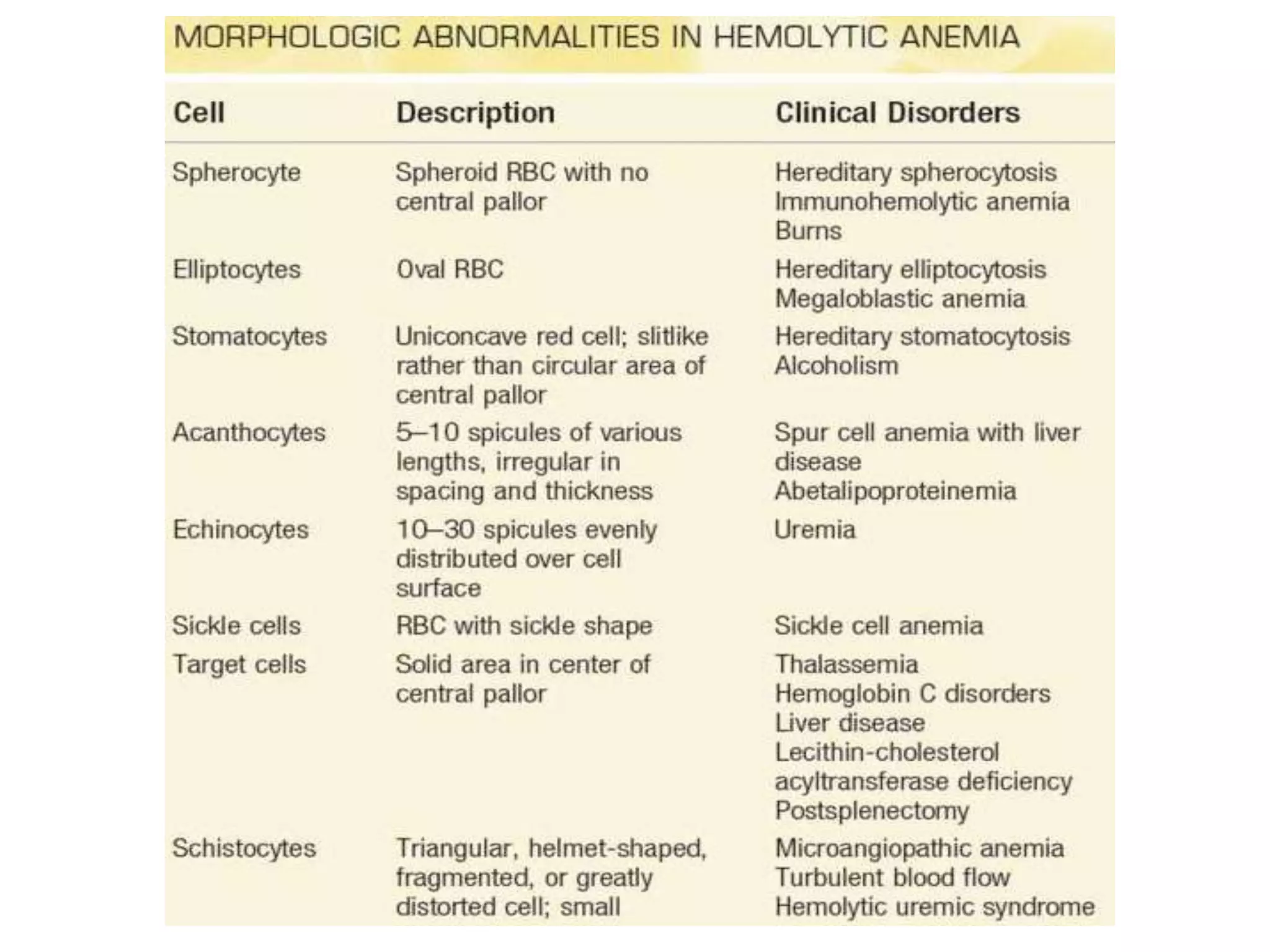
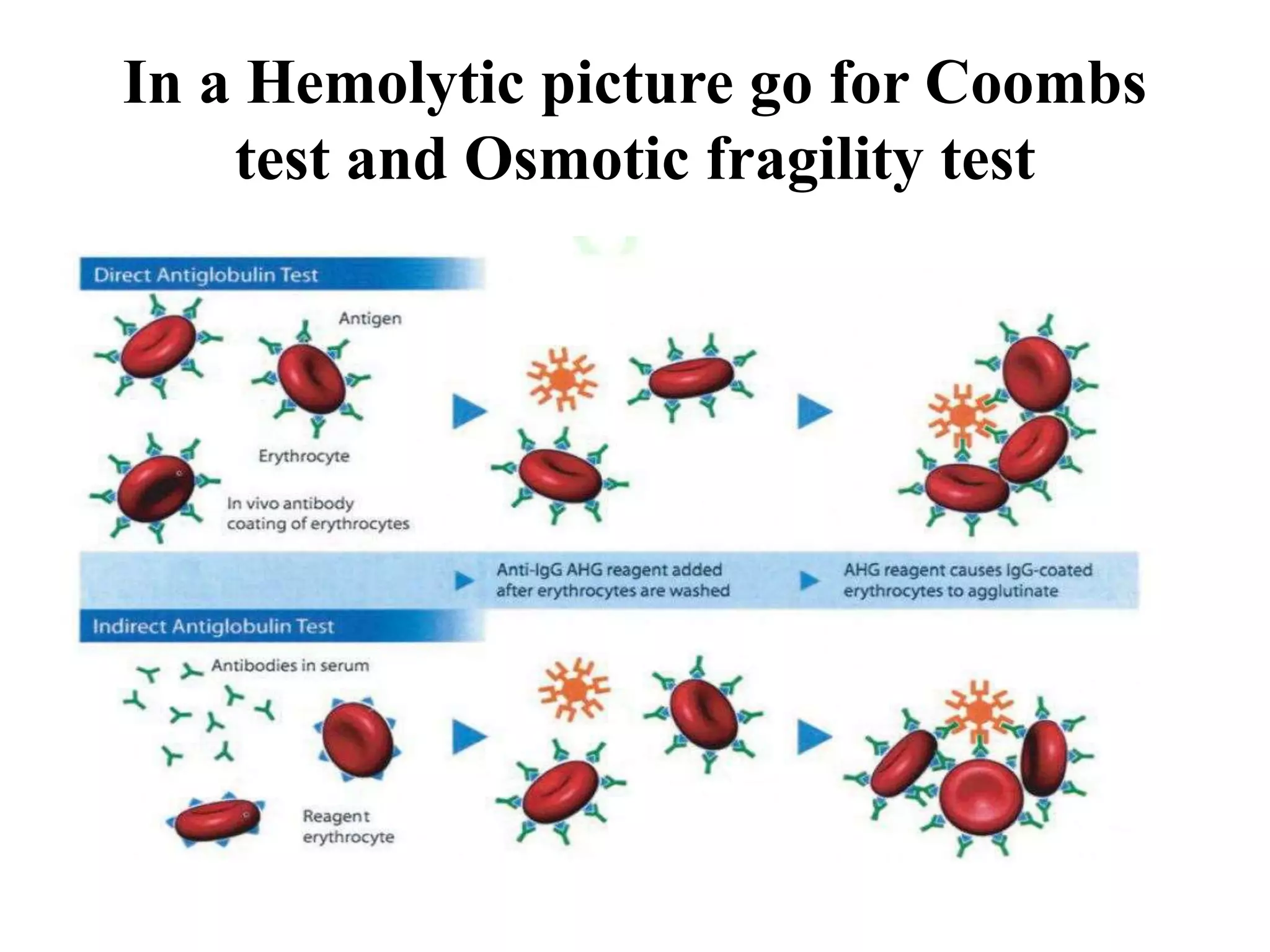
• Hemolytic anemia
• Decreased erythropoietin
secretion
• Renal: anemia of renal
insufficiency
• Hepatic: anemia of liver disease
• Anemia of endocrine deficiency
• Protein-calorie malnutrition
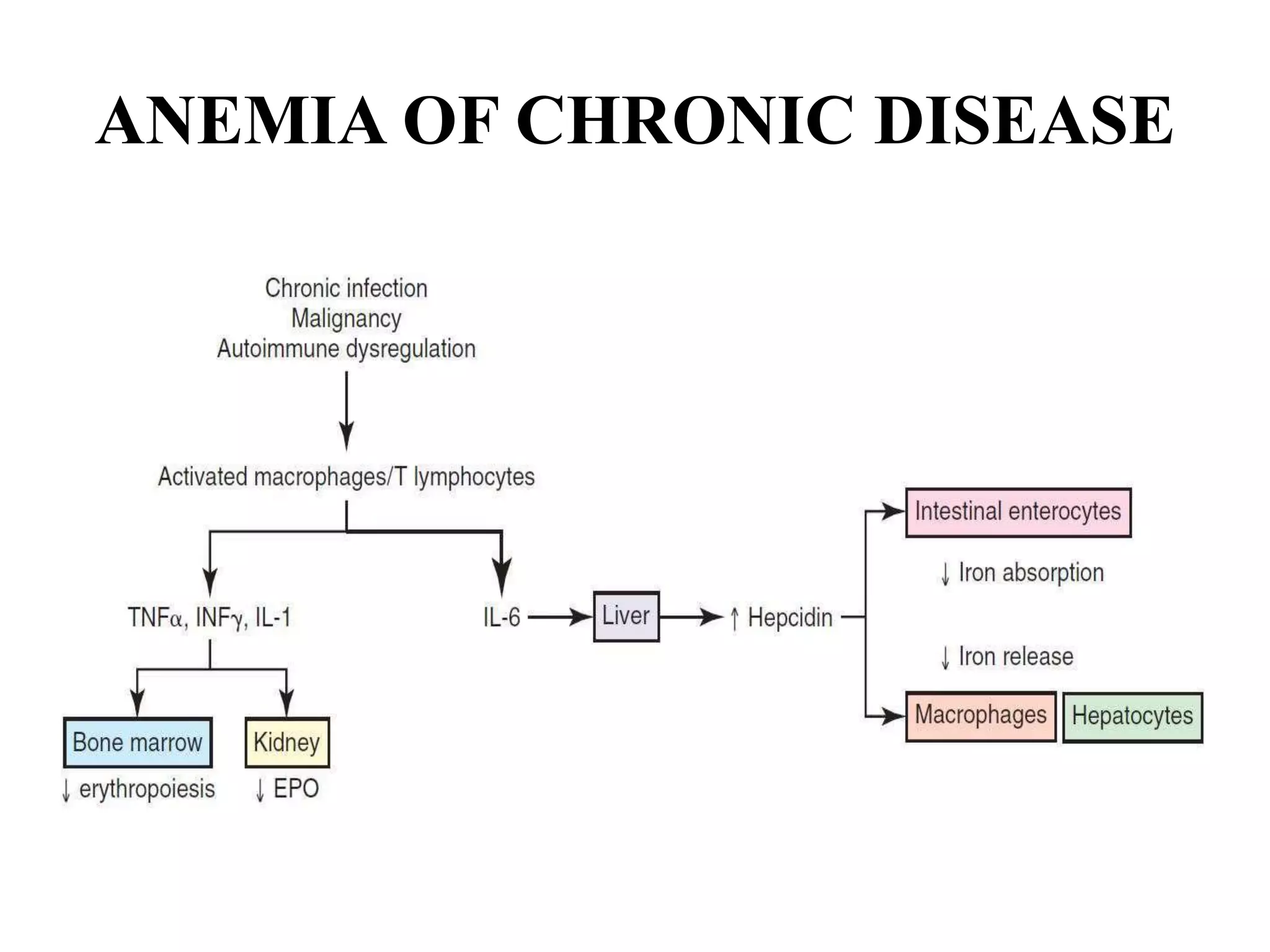
• Anemia of chronic disorders
• Anemia with impaired
marrow response
• Red blood cell aplasia
• Acquired pure red cell aplasia
in adults
• Transient aplastic crises
associated with hemolysis
• Aplastic anemia (pancytopenia)
• Bone marrow infiltrative
disorders
• Leukemia
• Myeloma
• Myelodysplastic anemias
• Congenital dyserythropoietic
anemia ([CDA] type II)](https://image.slidesharecdn.com/approachtoacaseofanemia-210208182405/75/approach-to-anemia-37-2048.jpg)