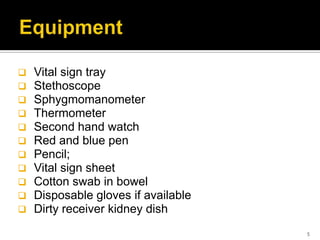
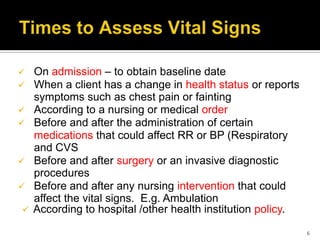
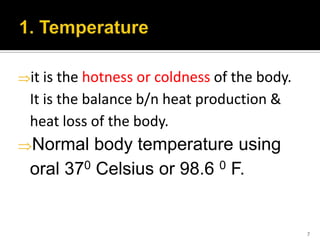
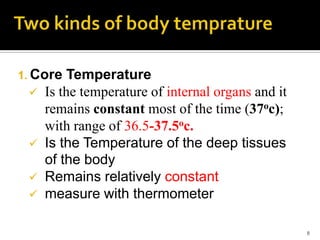
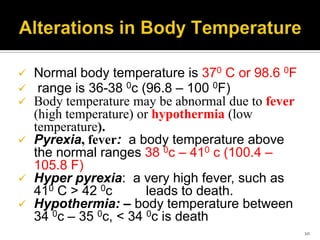
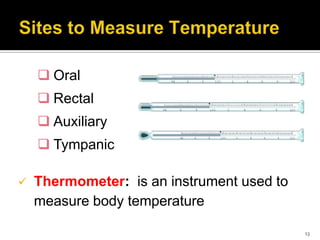
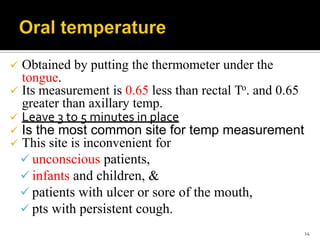
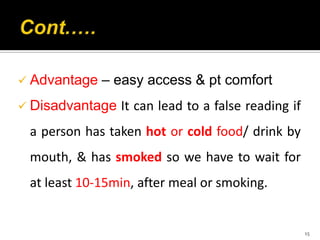
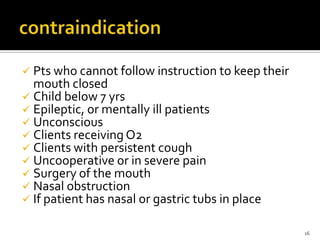
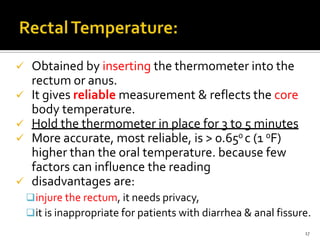
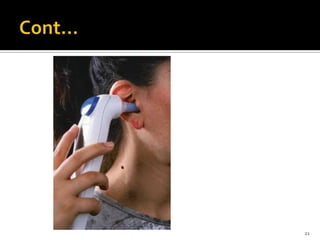
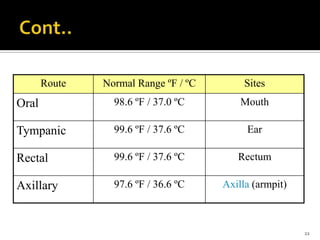
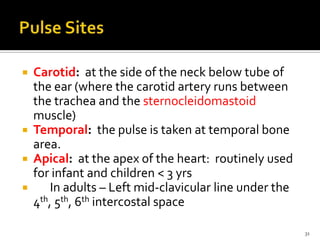
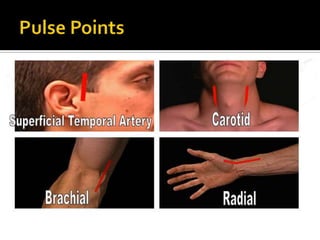
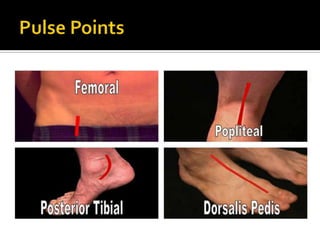
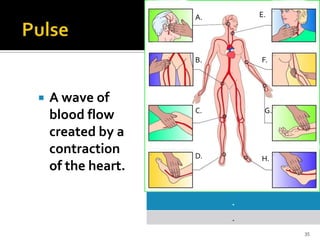
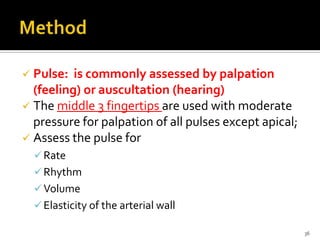
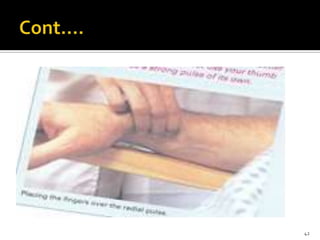
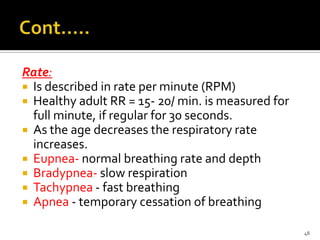
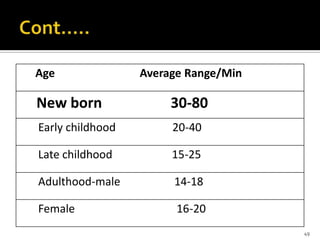
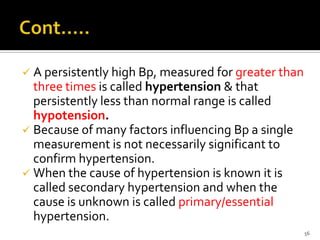
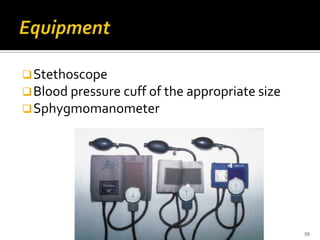
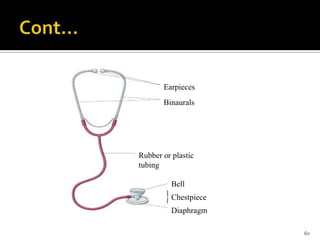
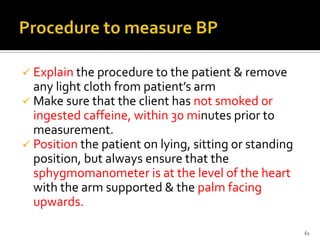
This document provides information on procedures for assessing and documenting vital signs, including temperature, pulse, respiration, and blood pressure. It describes how to measure each vital sign, normal ranges, factors that can influence readings, and equipment used. Temperature can be taken orally, rectally, axillary or via tympanic membrane. Pulse is assessed by palpation or auscultation. Respiratory rate is observed by chest or abdominal movement. Blood pressure is measured using a sphygmomanometer and stethoscope. Vital signs are documented to monitor patients' physiological status and identify changes requiring medical attention.