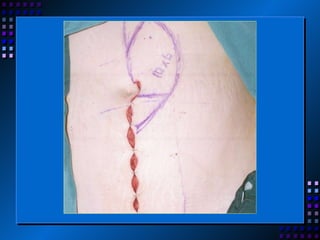
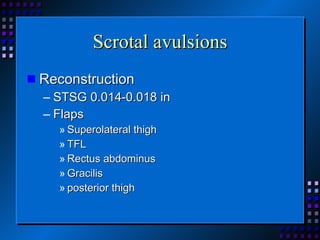
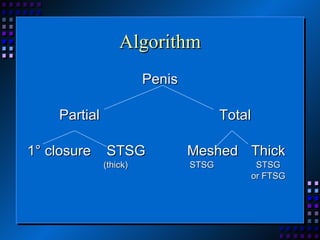
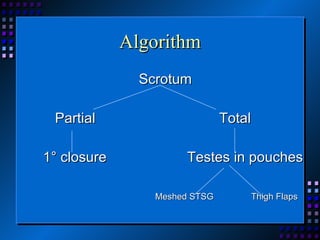
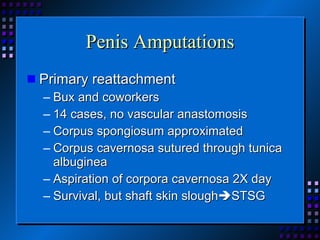
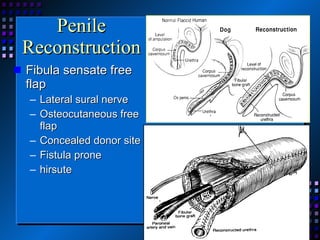
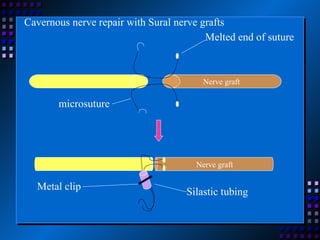
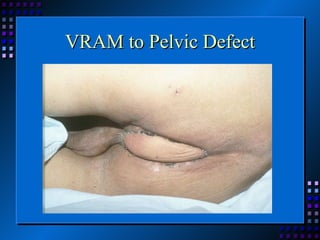
This document provides an overview of vaginal and genitourinary reconstruction techniques. It discusses the embryology and anatomy of the genital tract. It then covers various congenital defects including vaginal agenesis, ambiguous genitalia, and bladder exstrophy. Surgical techniques for vaginal reconstruction include serial dilation, bowel flaps, local flaps, and the McIndoe technique using a skin graft. Acquired defects from cancer or trauma can be addressed with skin grafts or flaps from the vulva, vaginal vault, penis, or scrotum. Goals of reconstruction include wound coverage and restoration of function.