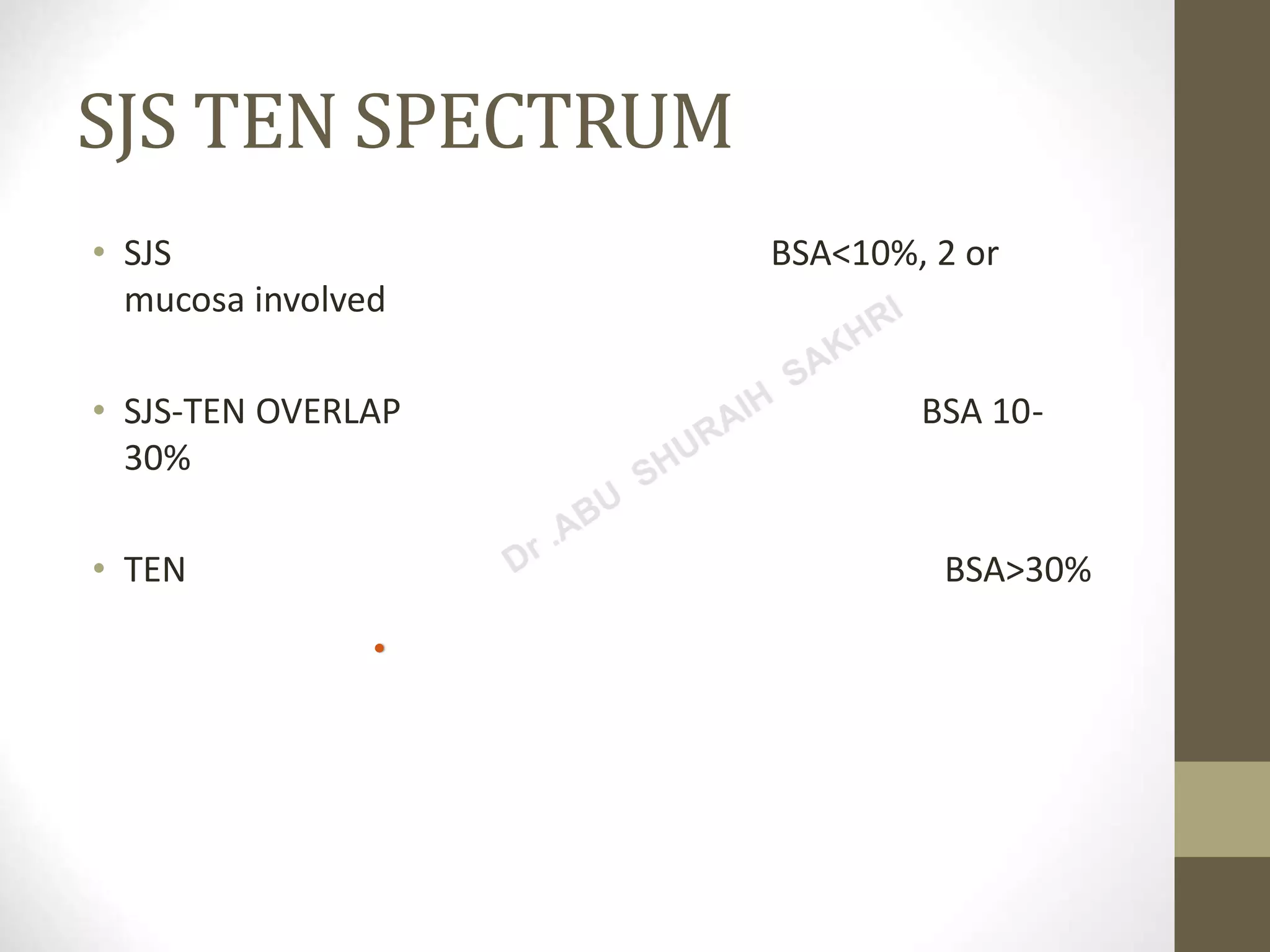
This document summarizes different types of urticaria (hives), angioedema, drug eruptions, and erythema multiforme. It describes the characteristics of acute and chronic urticaria, physical urticaria, urticarial vasculitis, and contact urticaria. It also discusses erythema multiforme, Stevens-Johnson syndrome/toxic epidermal necrolysis spectrum, fixed drug eruptions, exanthematous drug eruptions, and drug hypersensitivity syndrome. Treatment options are provided for many of these conditions.