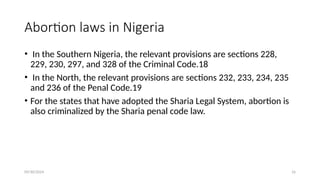
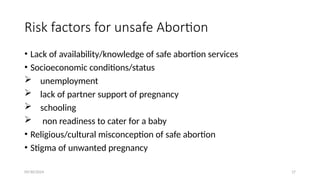
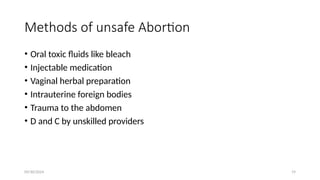
The document discusses the prevalence and risks of unsafe abortions, especially in Nigeria, where strict laws limit access to safe procedures, leading to significant maternal morbidity and mortality. It outlines factors contributing to unsafe abortions, including socioeconomic conditions, cultural misconceptions, and a lack of awareness of available services. The text also emphasizes the importance of prevention strategies, such as health education, improved access to contraceptive methods, and potential reforms in abortion legislation to reduce related health risks.

![09/30/2024 38
References
• Bamniya A, Verma S. The study of knowledge, attitude and practice about abortion and
technology at the tertiary centre in the region of Mewar, Rajasthan, India. Int J
ReprodContraception, Obstet Gynecol. 2018;7(8):3320–4.
• Ganatra B, Tunçalp Ö, Johnston HB, Johnson BR, Gülmezoglu AM, Temmerman M.From
concept to measurement: Operationalizing WHO’s definition of unsafe abor1.Ganatra B,
Tunçalp Ö, Johnston HB, Johnson BR, Gülmezoglu AM, Temmerman M.From concept to
measurement: Operationalizing WHO’s definition of unsafe abortion.Vol. 92, Bulletin. Bull
World Health Organ [Internet]. 2014;92(3):155. [cited 2020 04 23].Available from: doi:
http://dx.doi.org/10.2471/BLT.14.136333](https://image.slidesharecdn.com/unsafeabortion3-1-240930154520-8063c3de/85/Unsafe-Abortion-And-post-abortion-care-38-320.jpg)