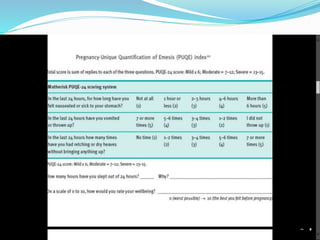
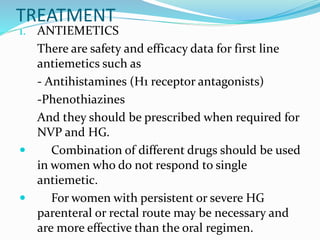
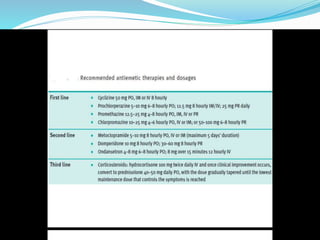
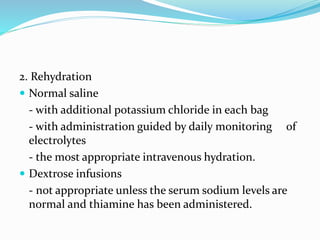
Nausea and vomiting in pregnancy (NVP), including hyperemesis gravidarum (HG), are common conditions affecting up to 80% of pregnant women. NVP diagnosis is based on symptoms in the first trimester without other causes, while HG diagnosis requires weight loss of over 5%, dehydration, and electrolyte imbalance. Treatment involves antiemetics, rehydration, nutritional support, and monitoring for complications like dehydration. Recurrence is common, so management involves lifestyle changes, early antiemetic use, and multidisciplinary support in severe cases.