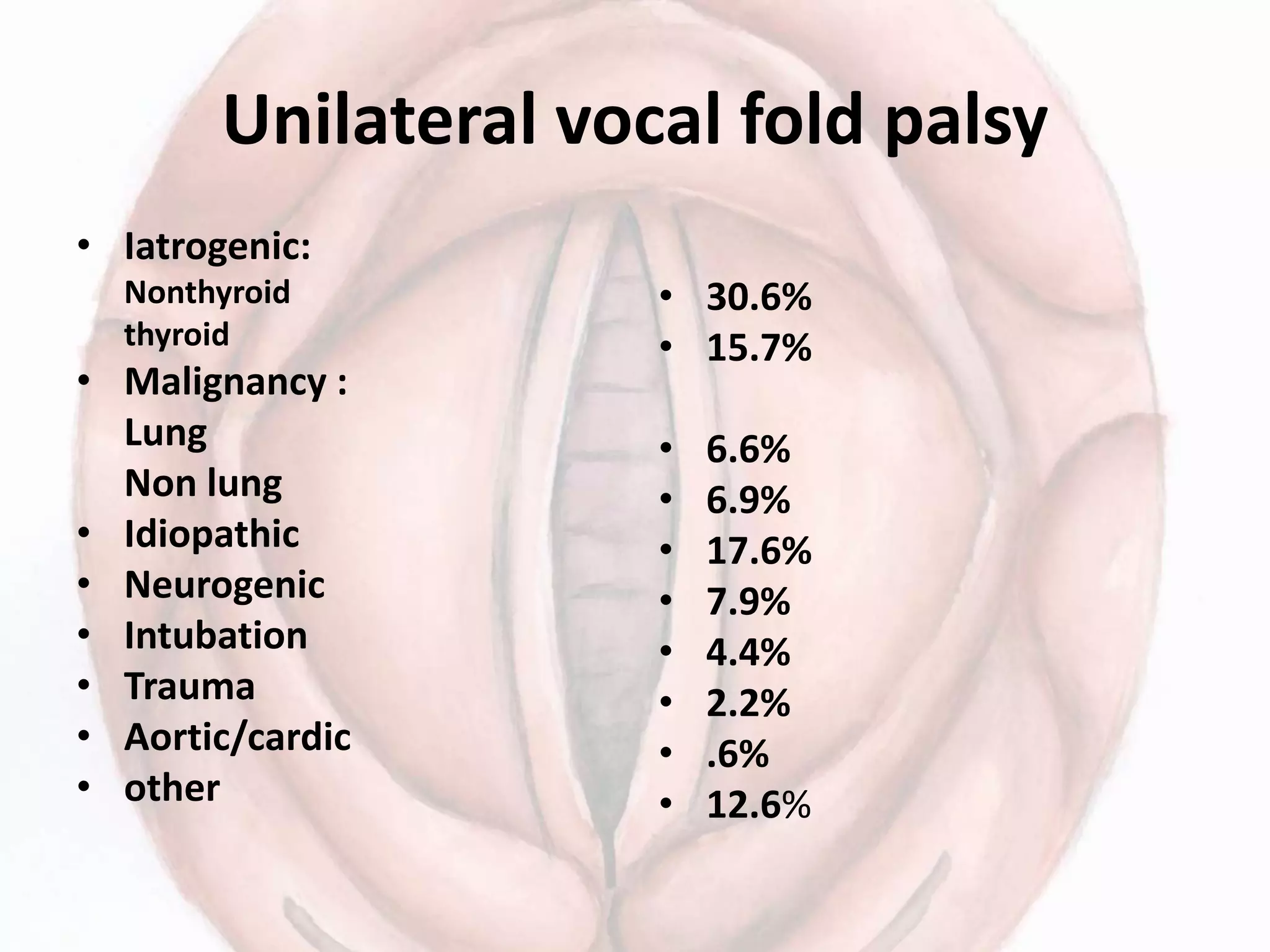
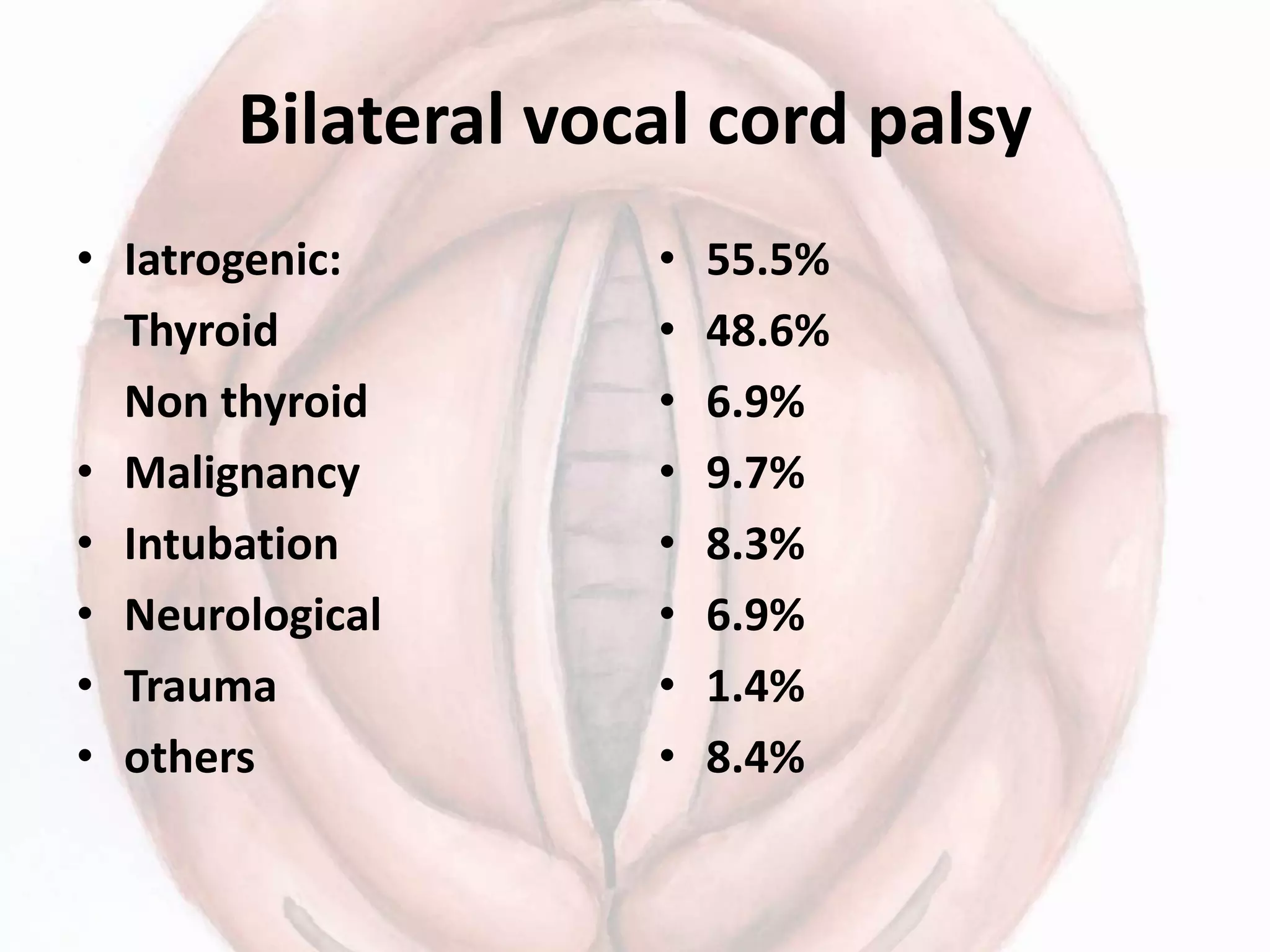
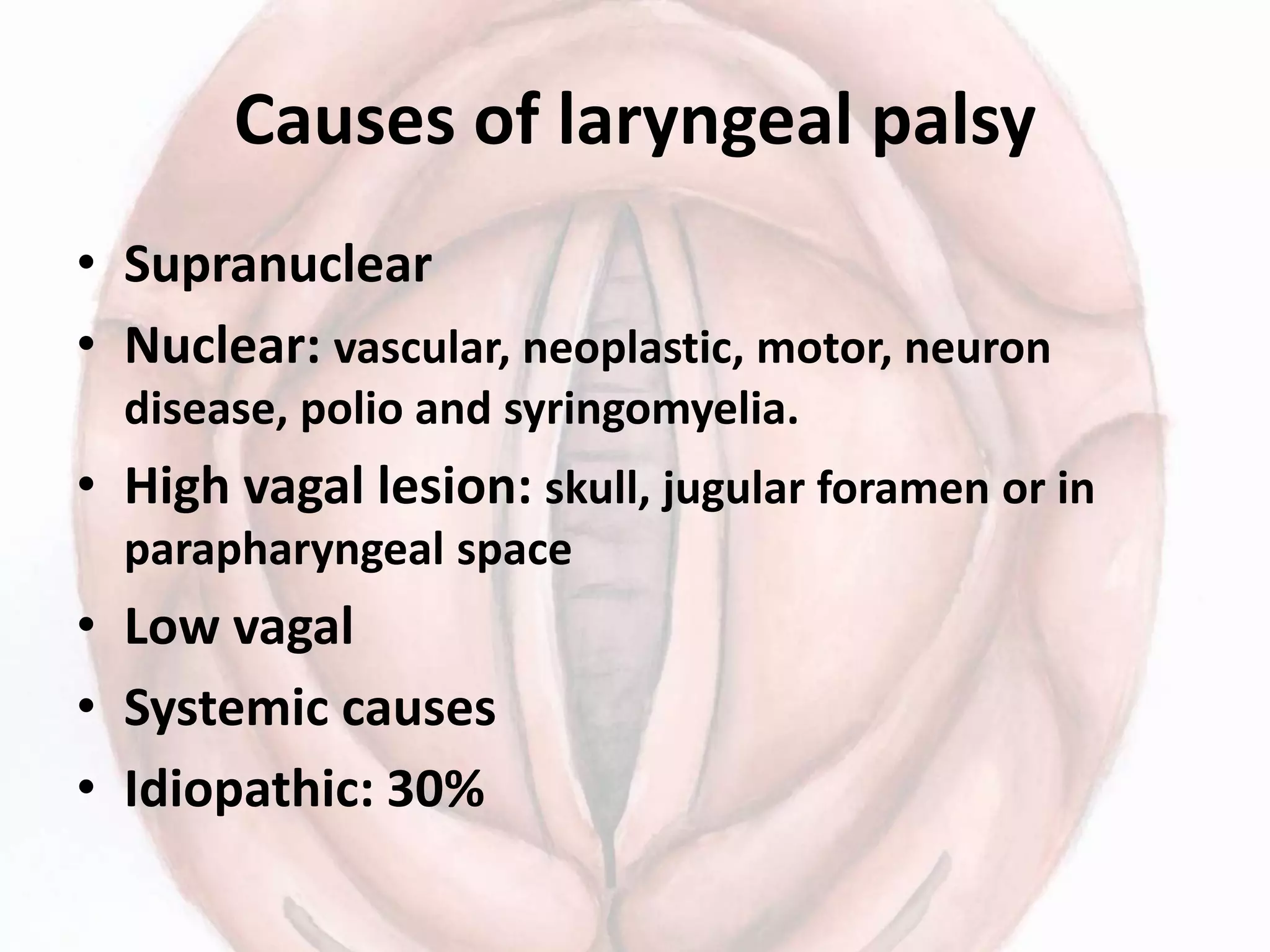
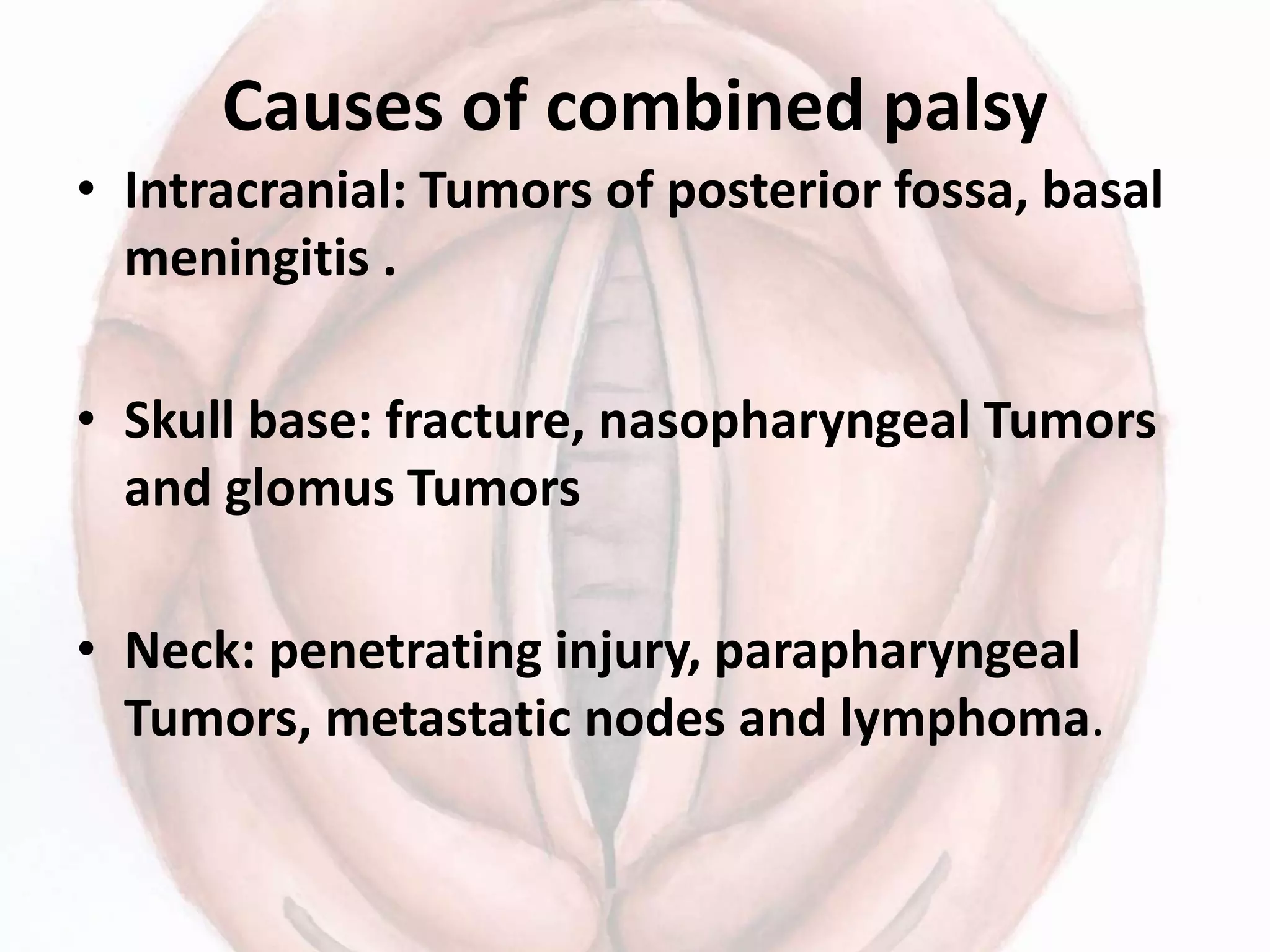
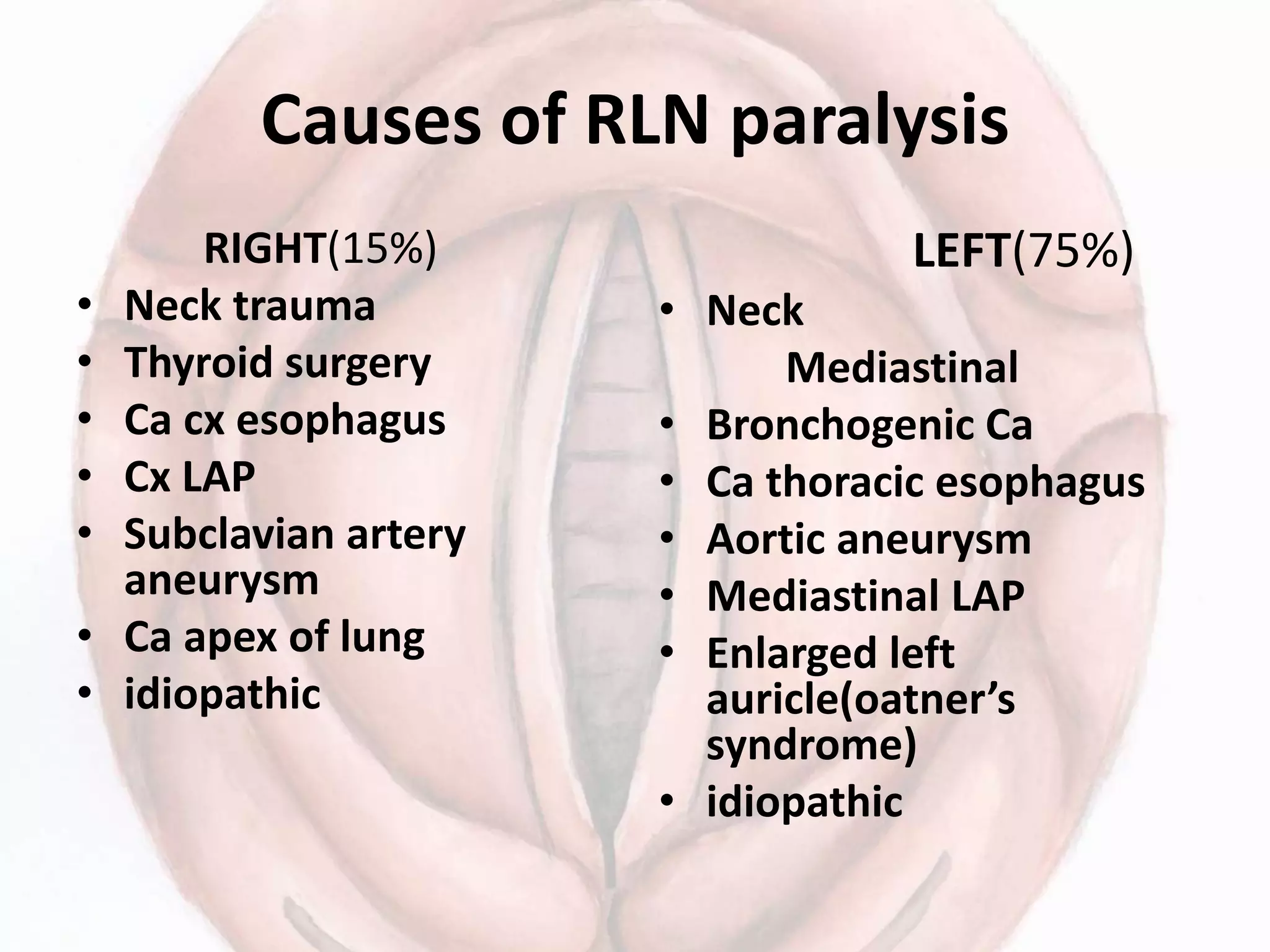
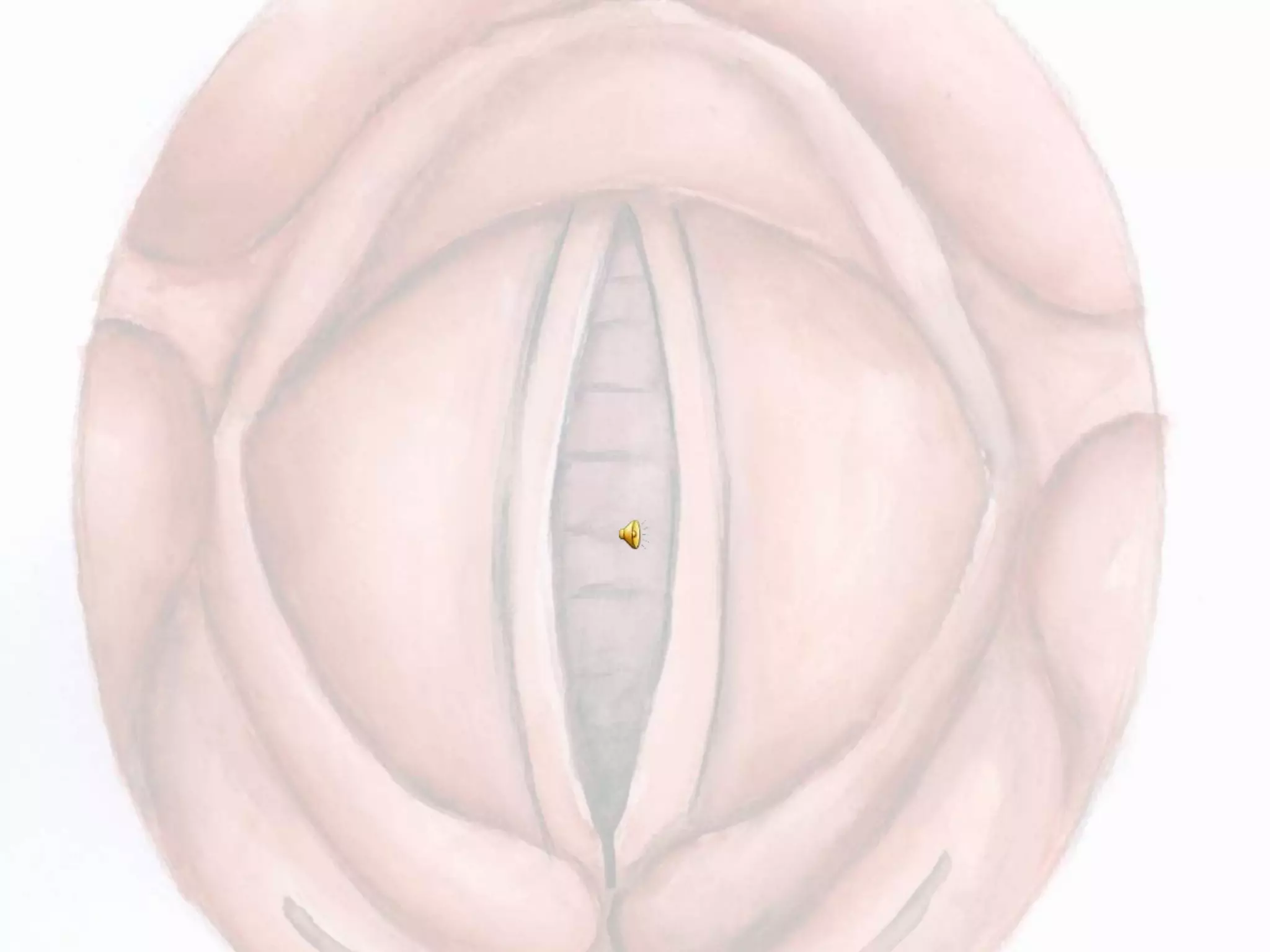
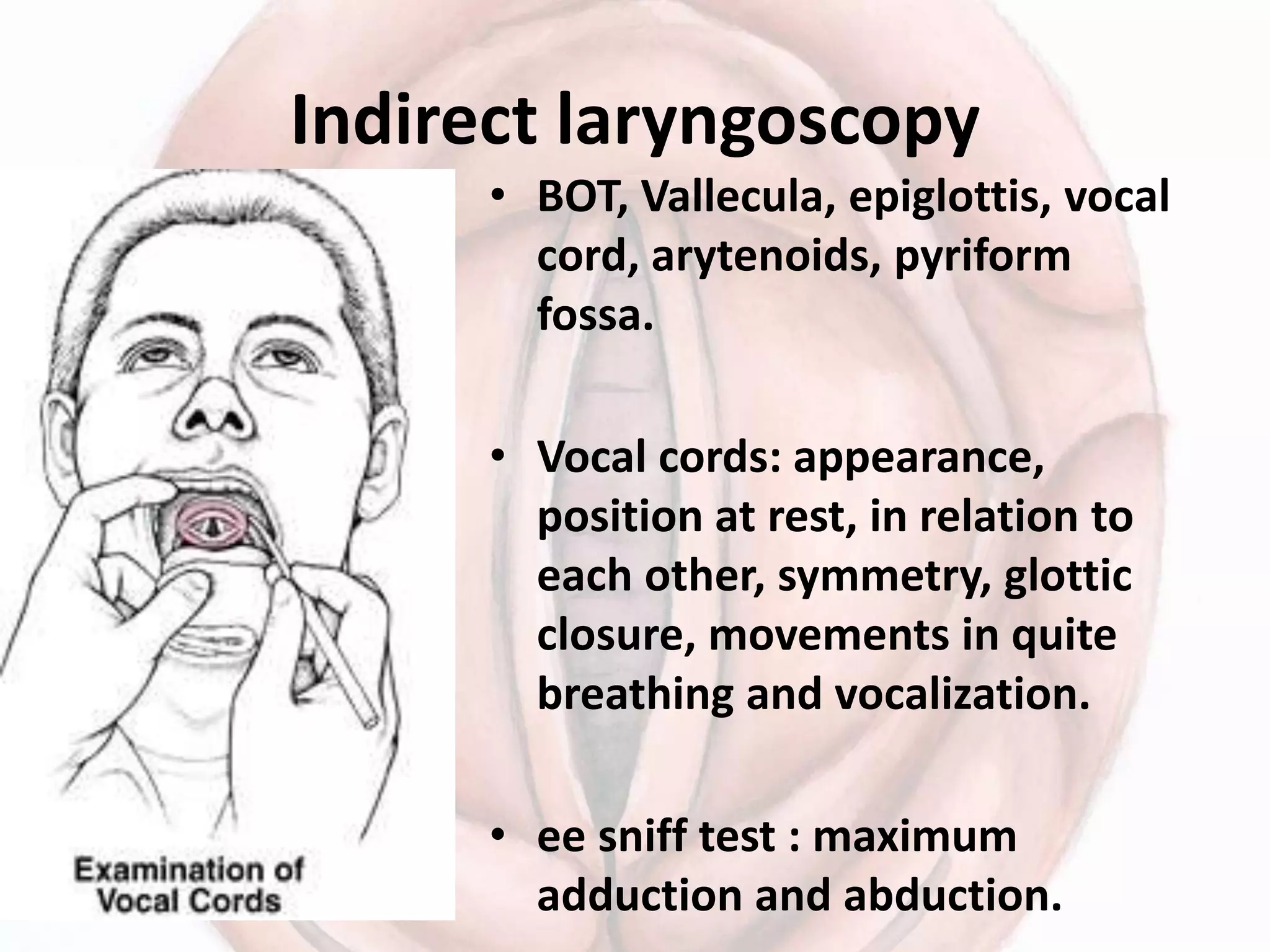
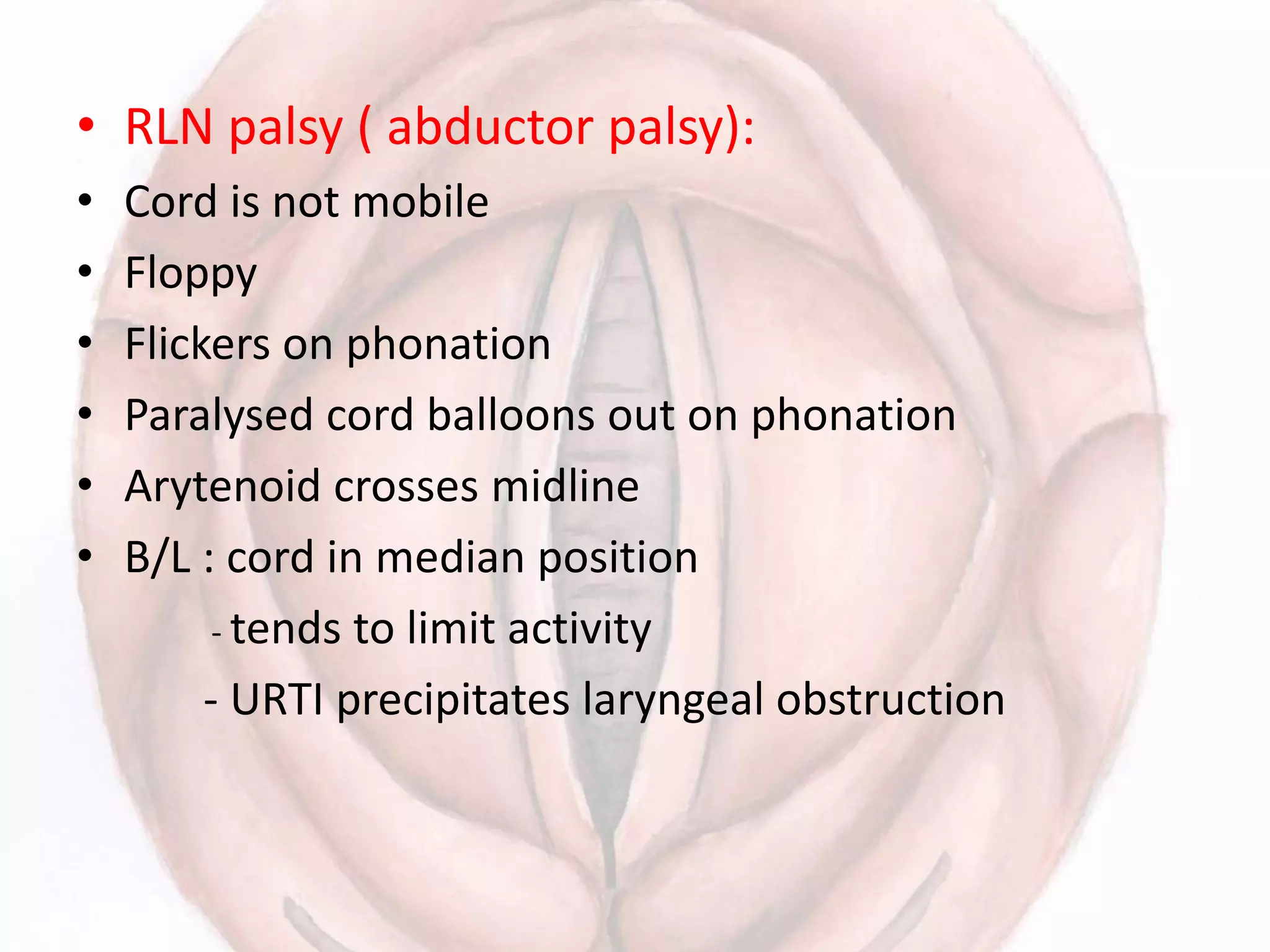
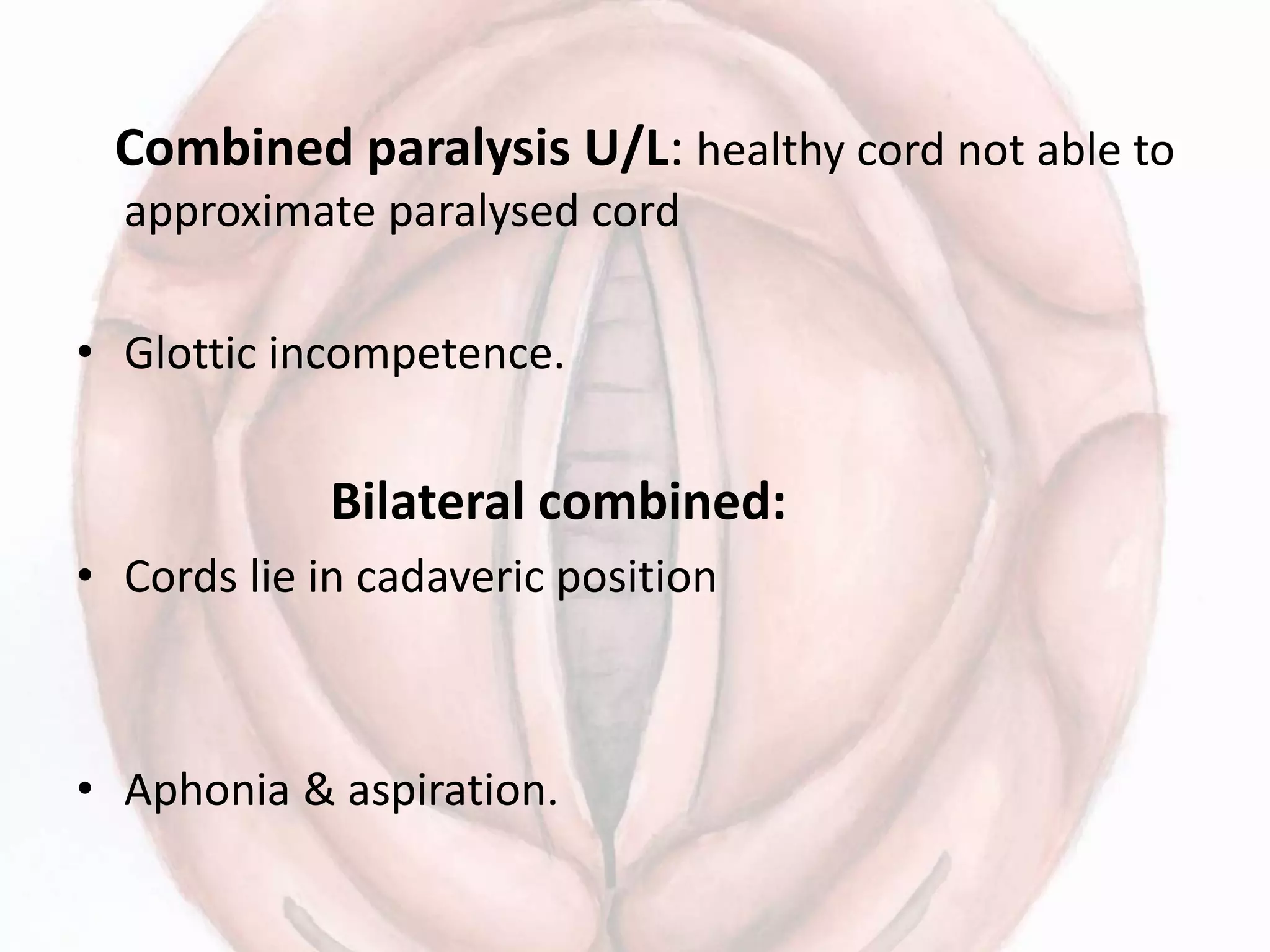
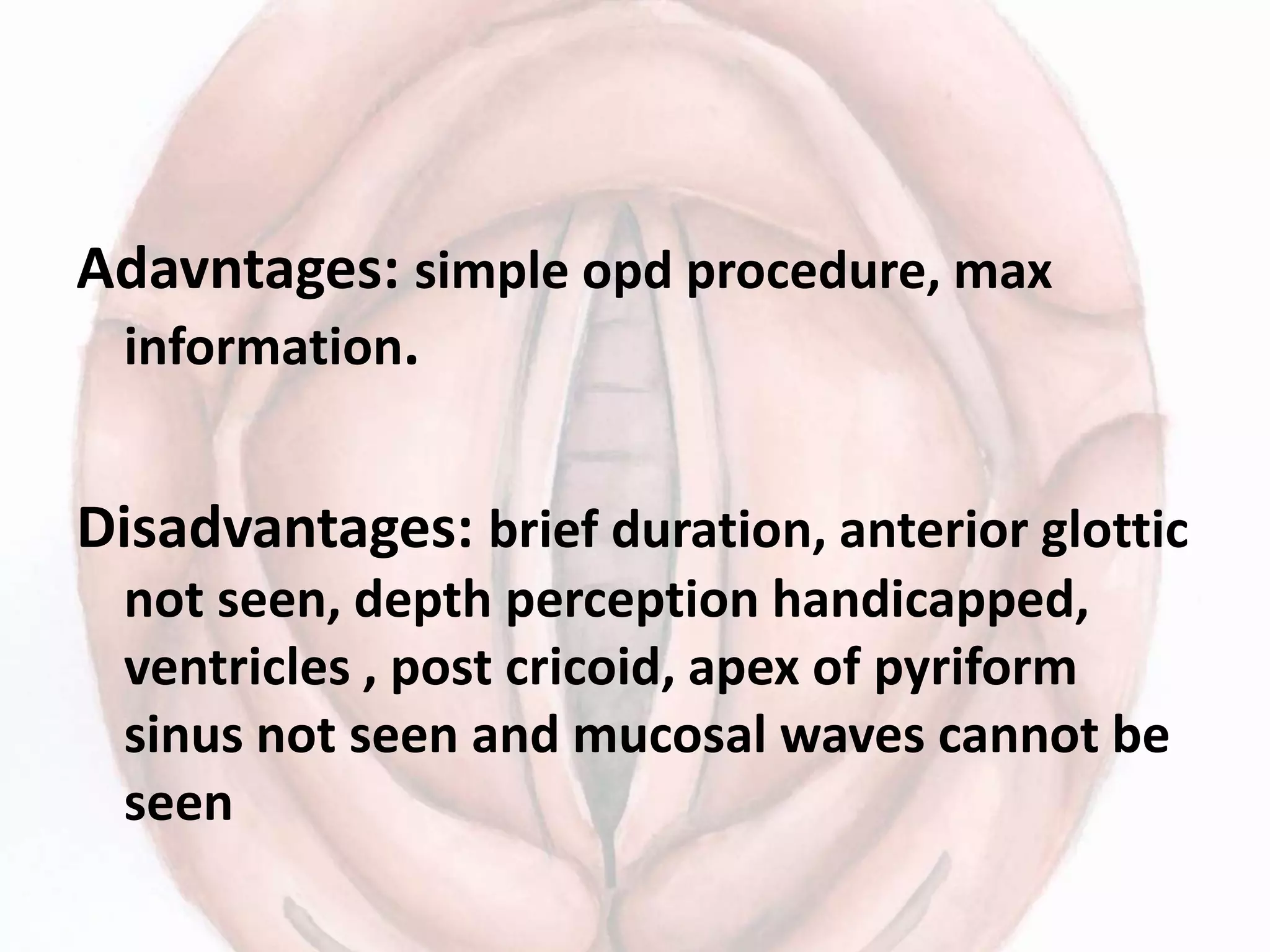
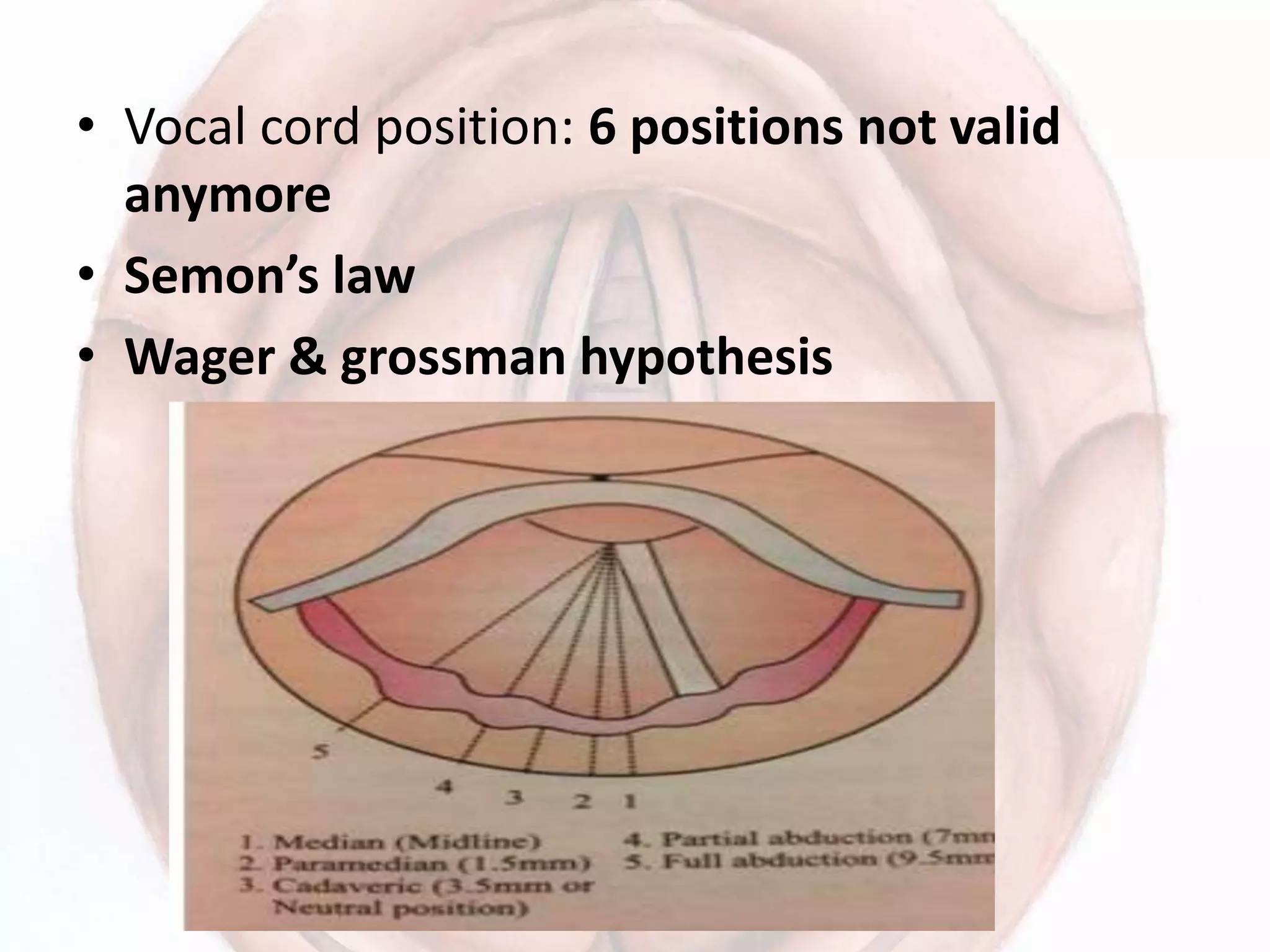
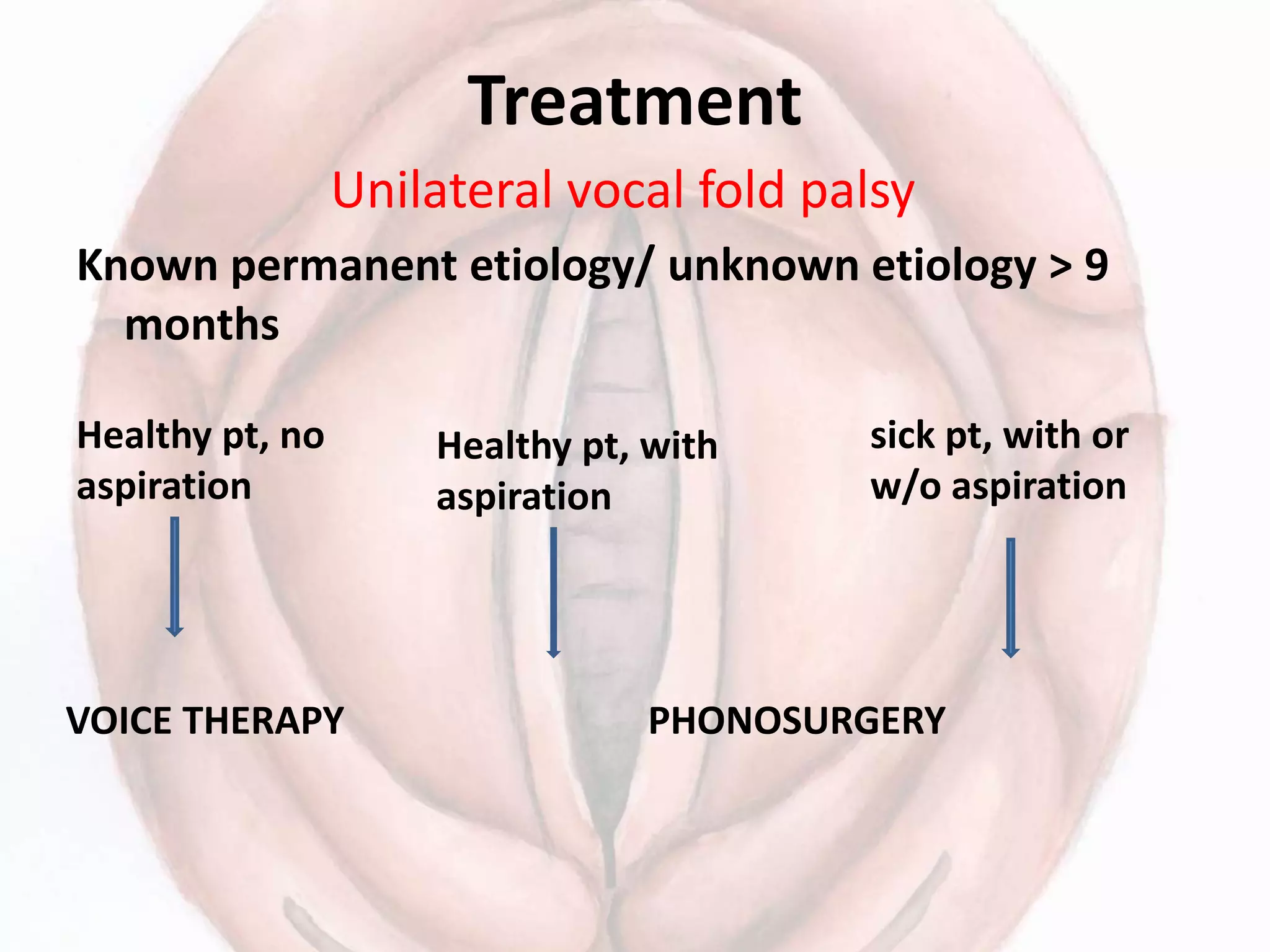
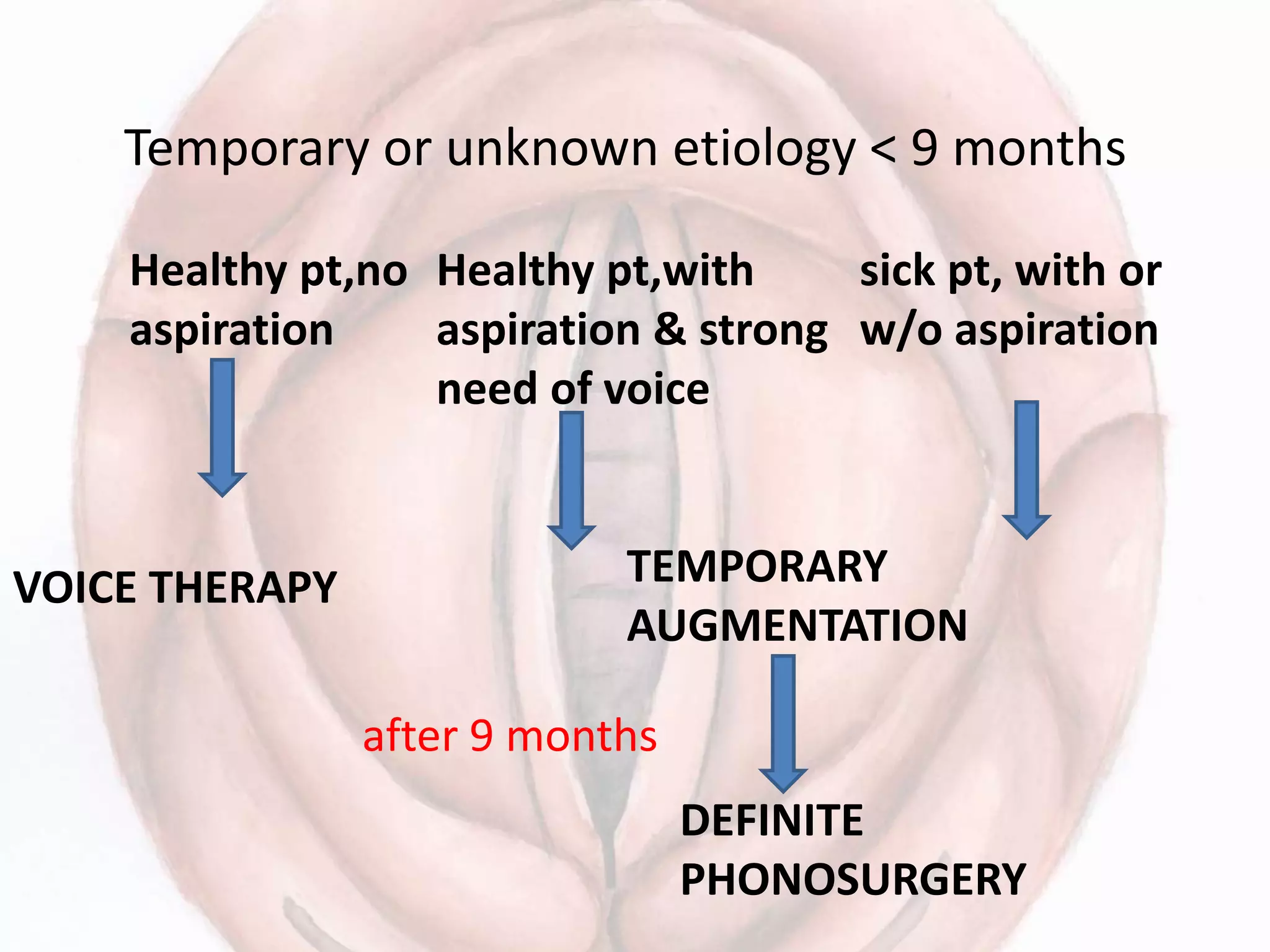
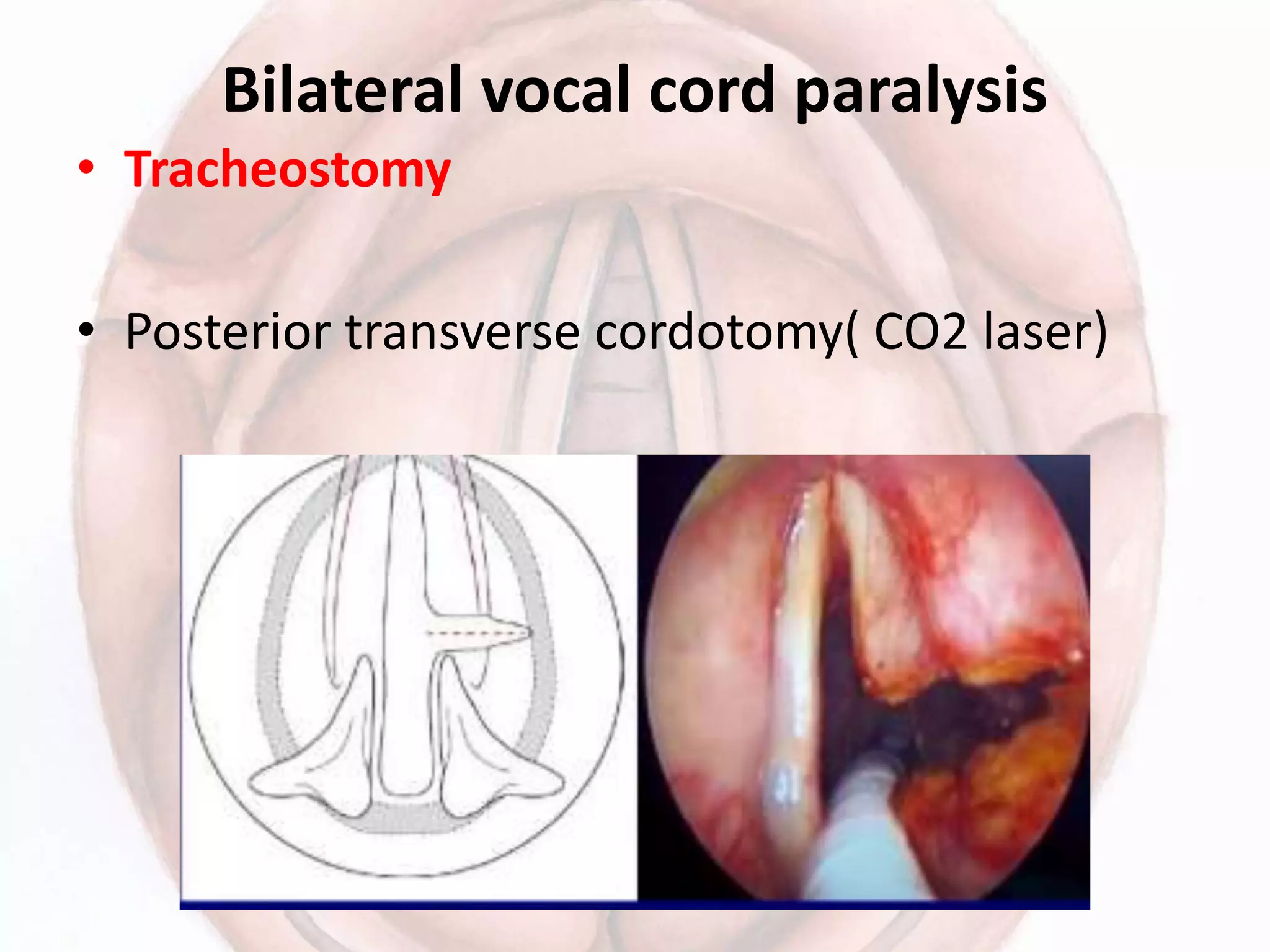
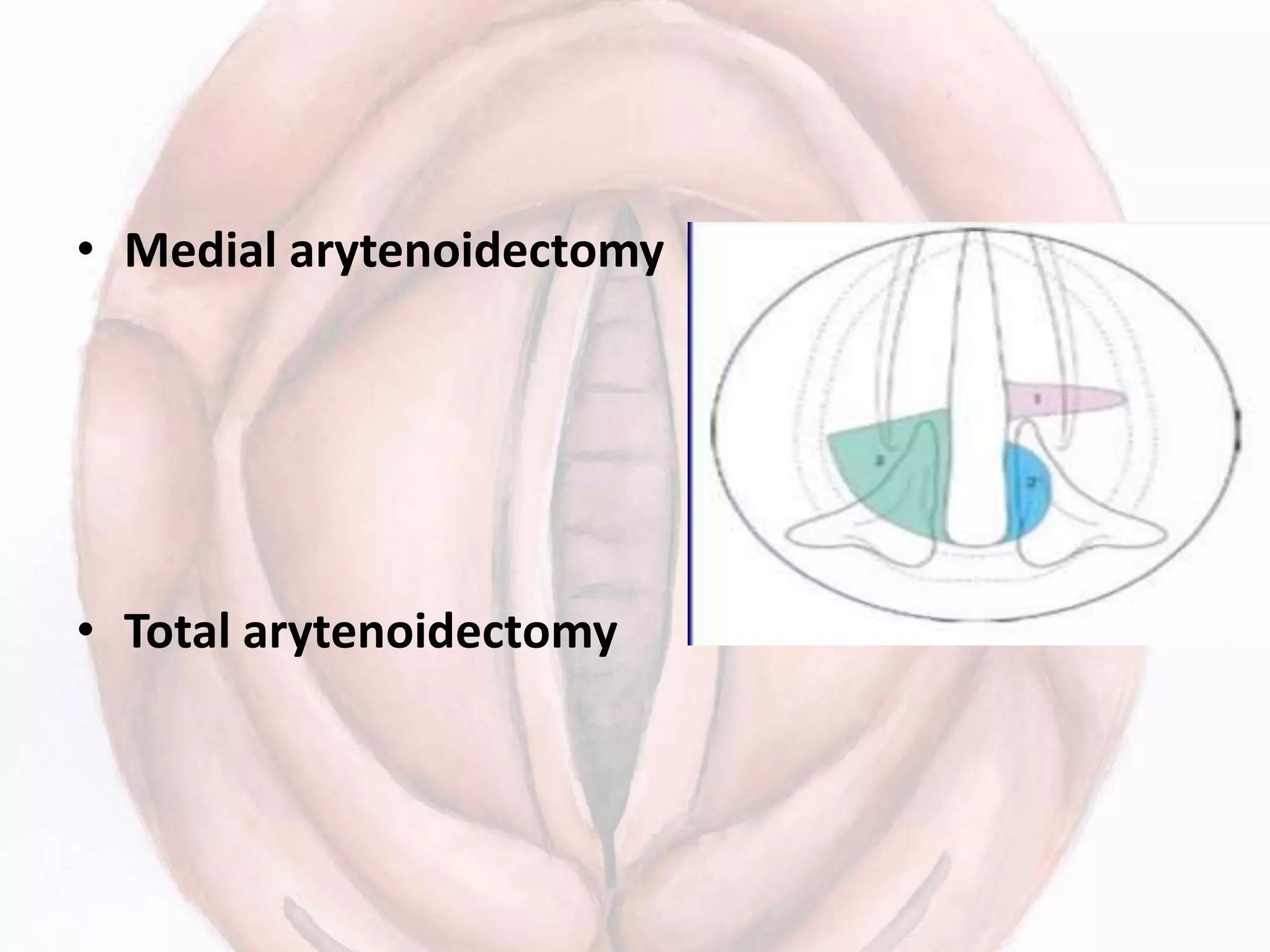
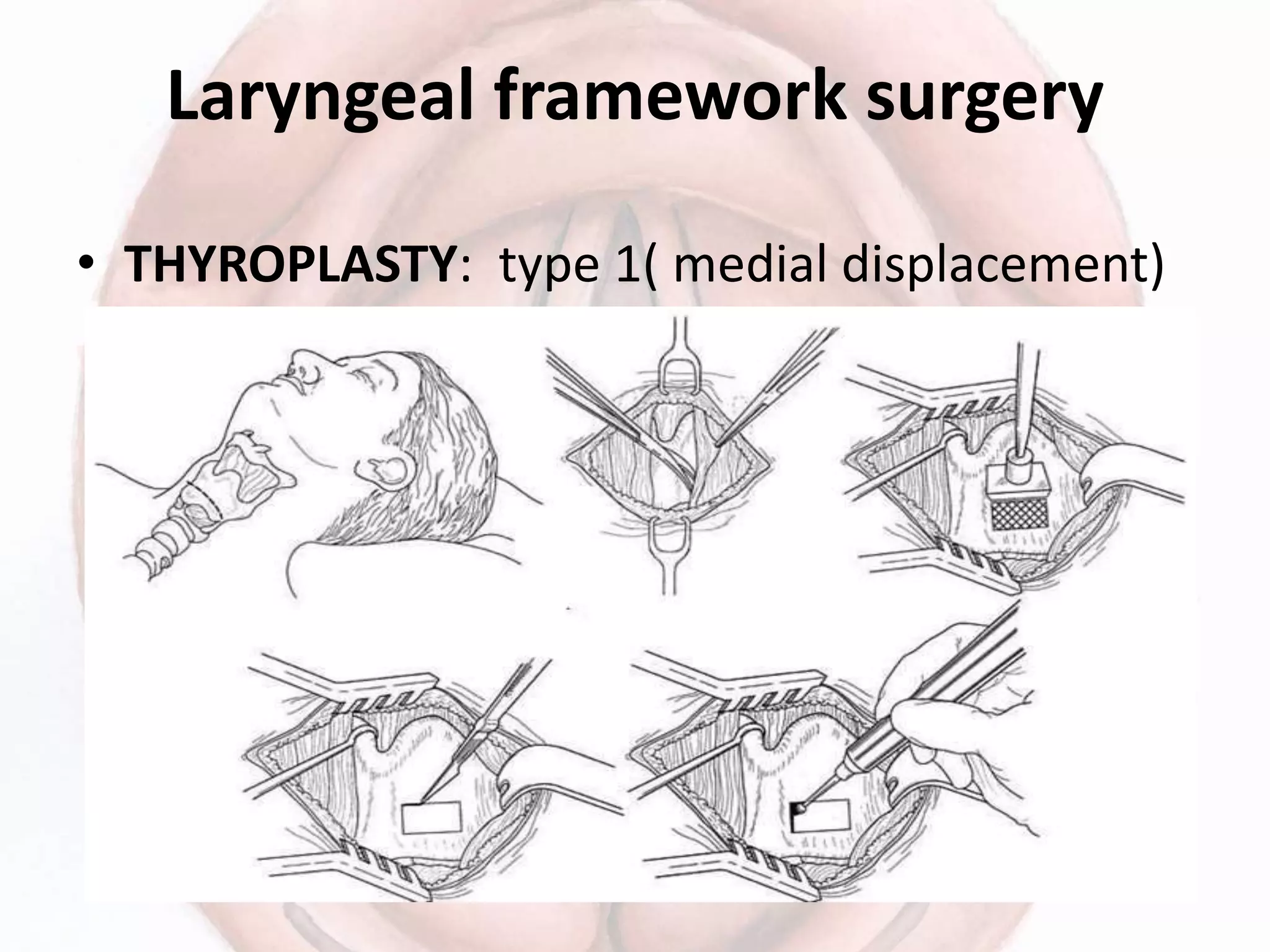
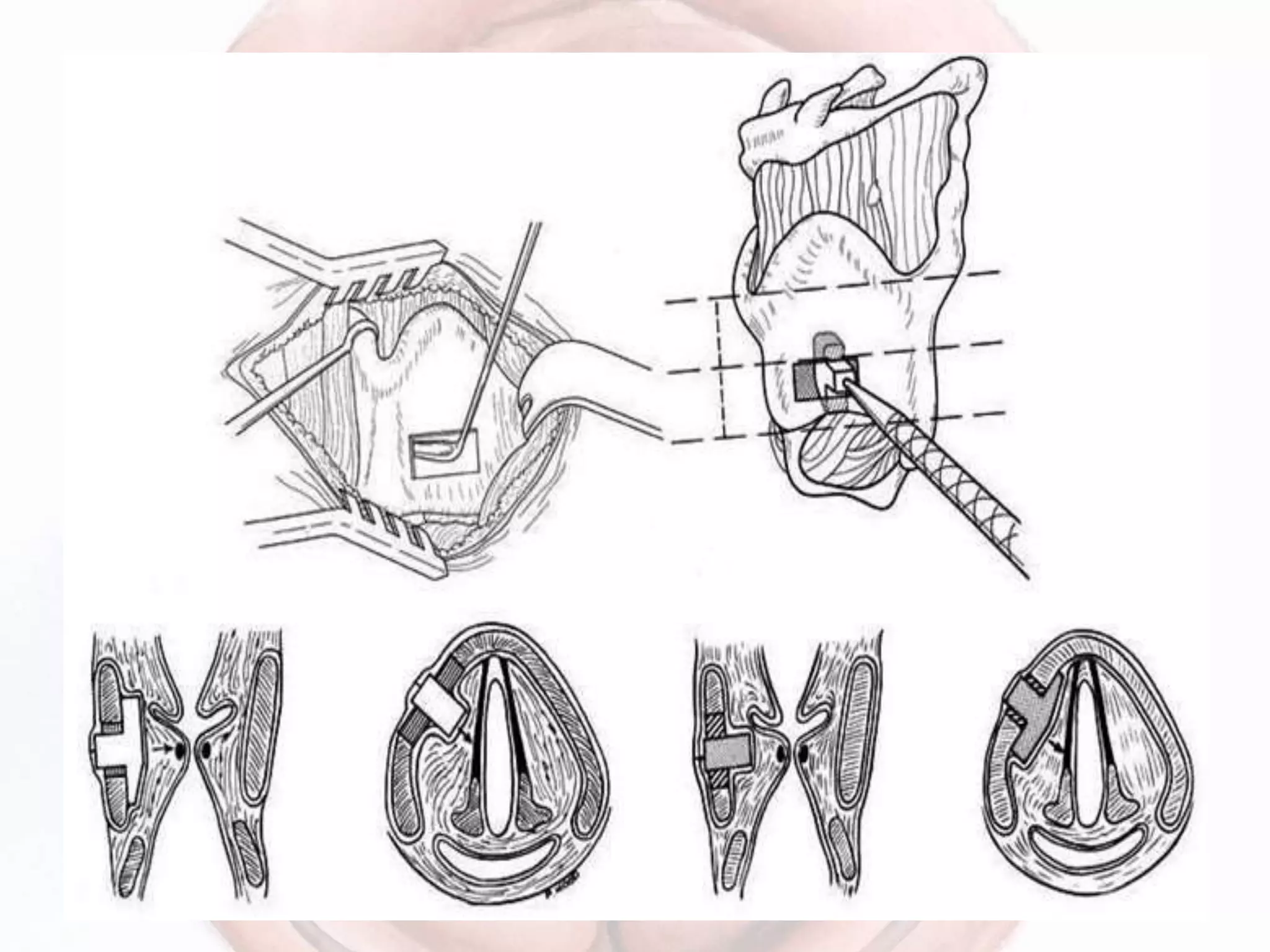
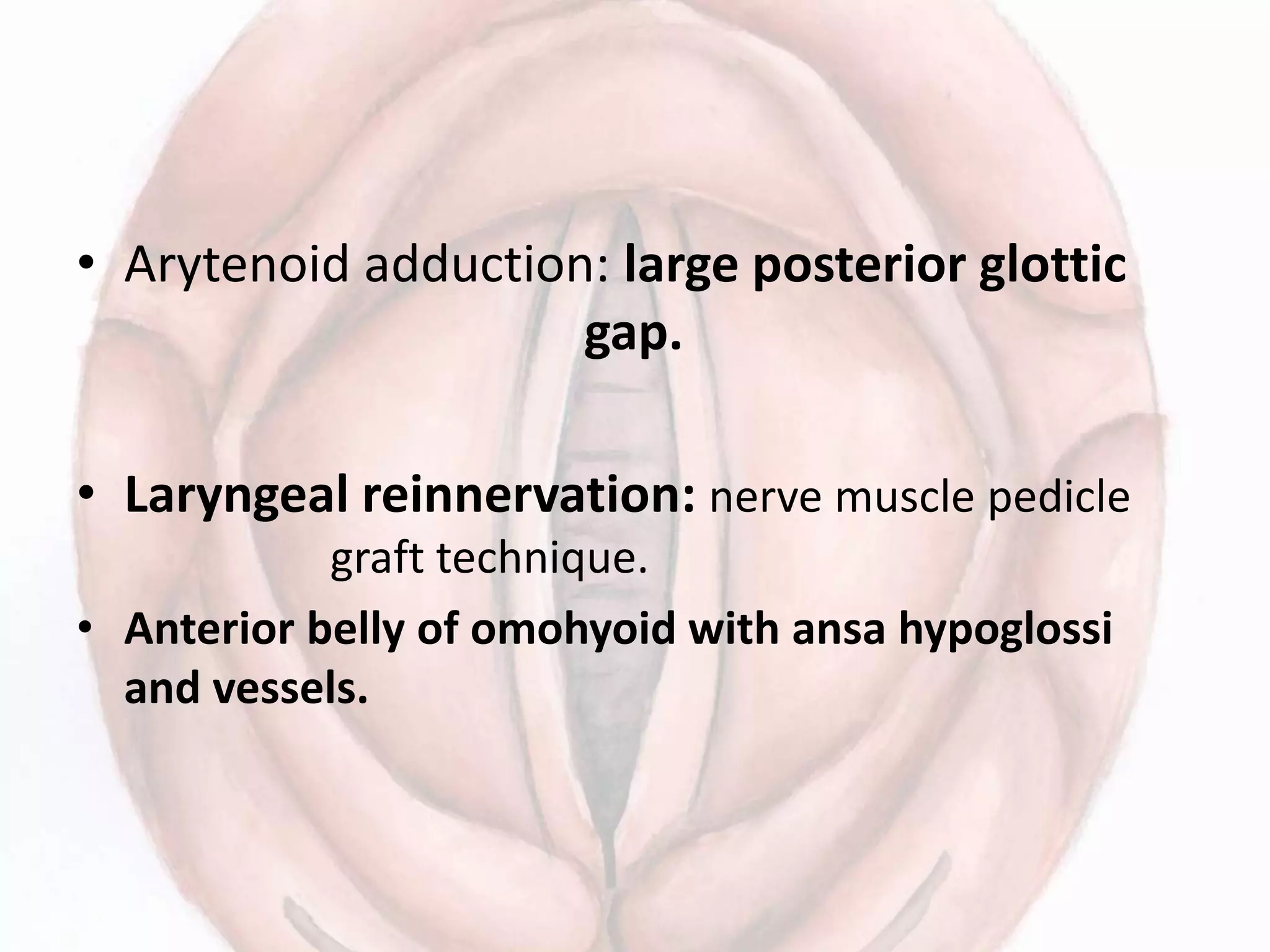
This document provides information on the approach to patients presenting with vocal cord paralysis. It discusses the epidemiology, causes, examination findings, investigations, and treatment options. Regarding unilateral vocal cord paralysis, the most common etiologies are iatrogenic (e.g. thyroid surgery), malignancy, and idiopathic. Bilateral paralysis is often due to thyroid surgery or intubation. Examination involves assessing voice quality and cord mobility. Investigations aim to identify underlying causes, and may include imaging, biopsies, and electromyography. Treatment depends on severity and chronicity, and may involve voice therapy, temporary augmentation, or phonosurgery like thyroplasty. Bilateral paralysis requires airway management