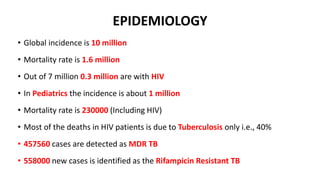
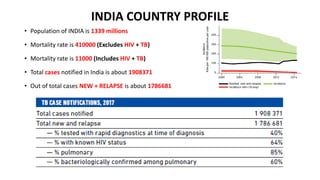
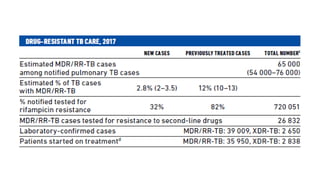
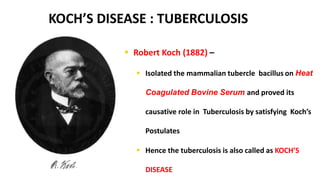
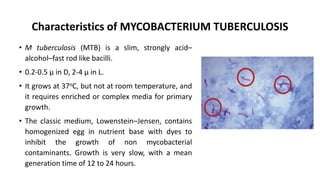
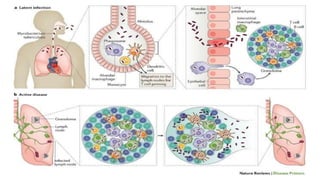
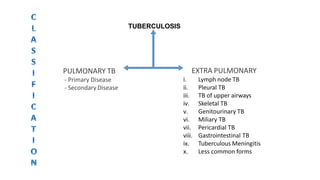
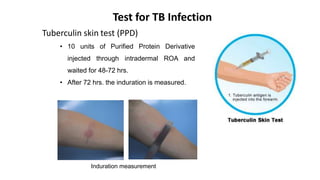
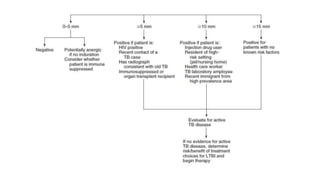
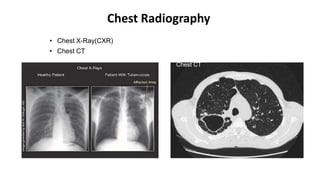
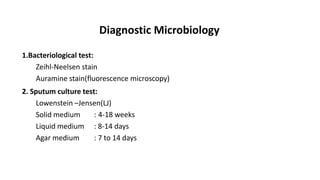
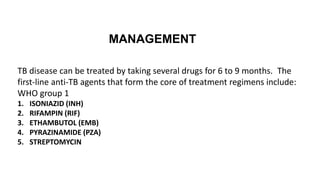
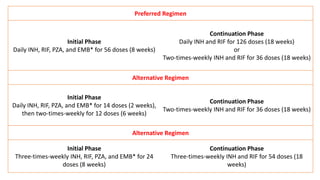
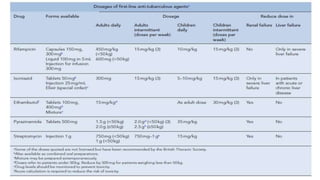
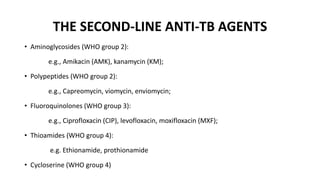
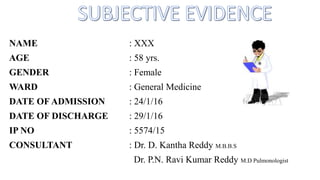
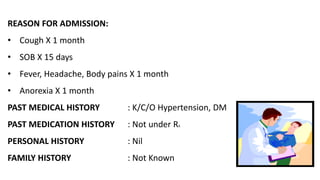
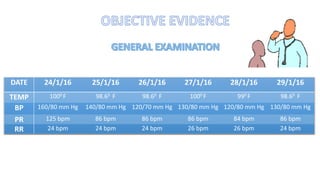
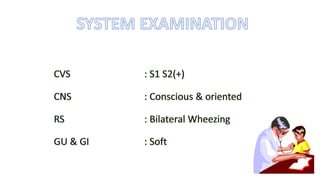
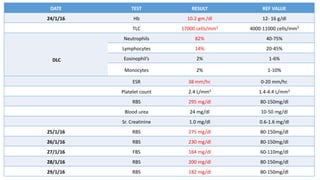
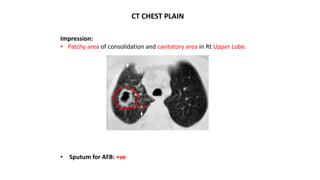
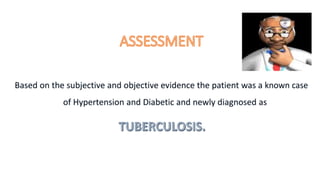
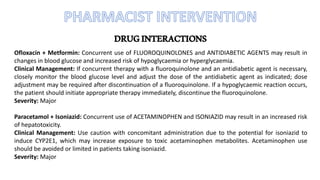
The document provides information on tuberculosis including its definition, epidemiology, etiology, pathophysiology, classification, clinical presentation, diagnosis, management, and a sample case presentation. Tuberculosis is defined as an infectious disease caused primarily by Mycobacterium tuberculosis that usually affects the lung parenchyma. It discusses trends in global and India-specific TB incidence and mortality. Etiology and characteristics of M. tuberculosis are explained. The pathophysiology, types of TB, and typical clinical signs and symptoms are summarized. Diagnosis involves medical history, physical exam, tuberculin skin test, chest X-ray, microbiological tests, and blood tests. Management outlined first and second-line anti-TB drug reg