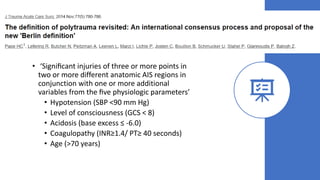
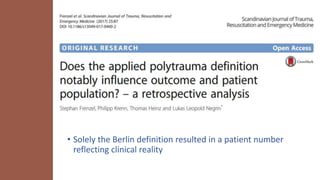
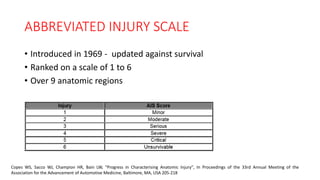
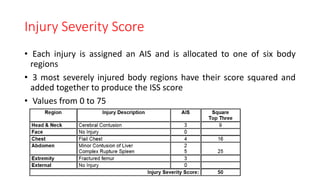
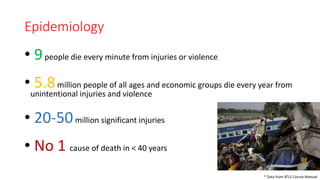
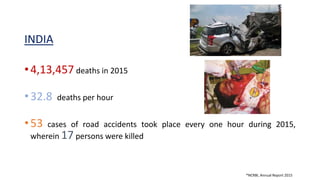
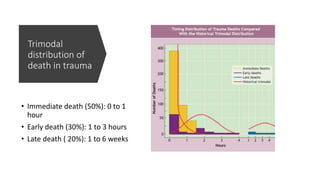
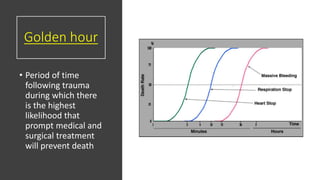
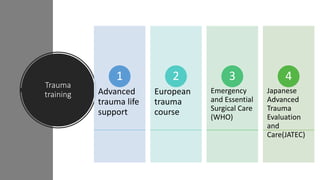
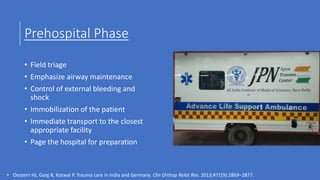
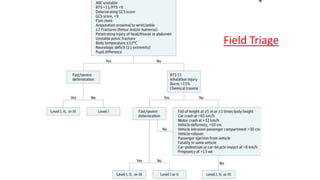
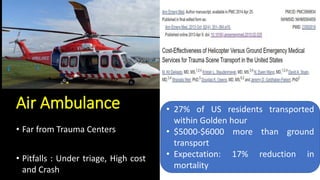
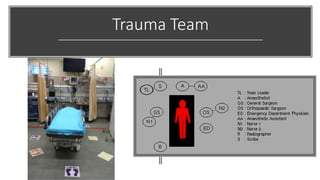
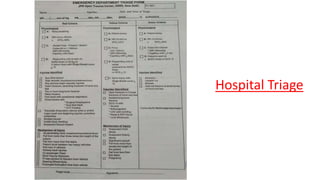
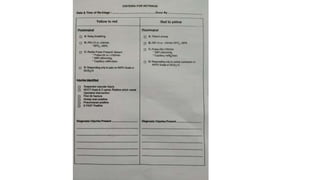
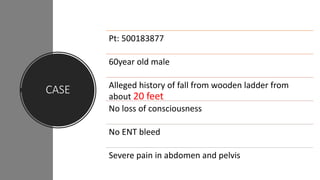
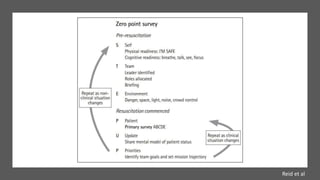
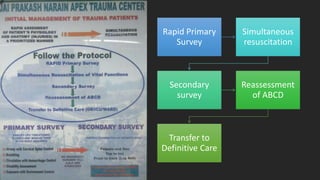
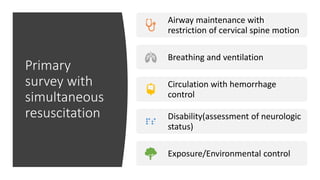
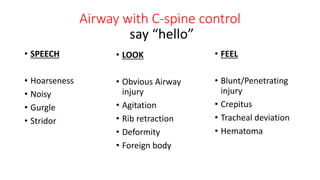
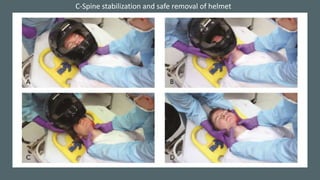
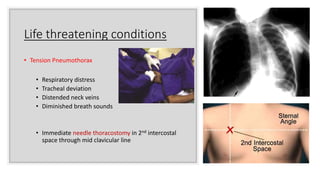
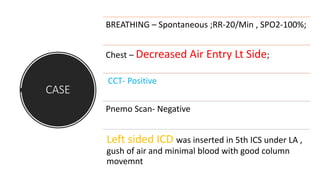
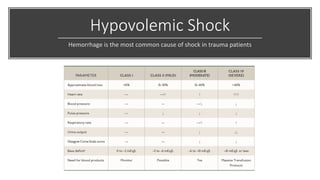
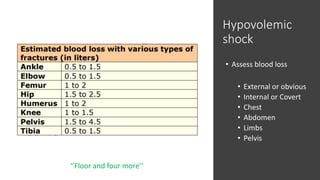
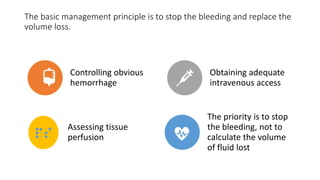
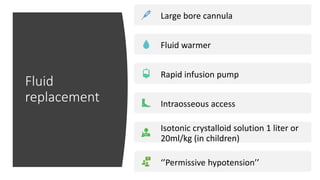
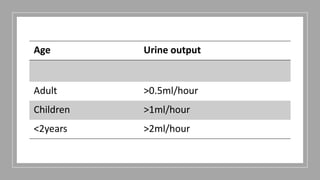
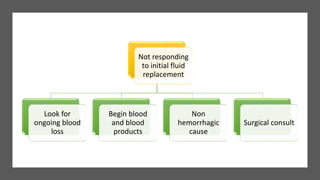
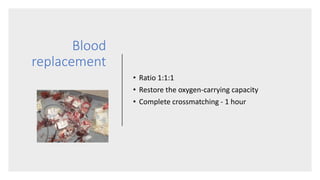
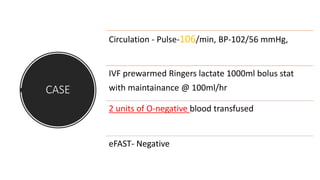
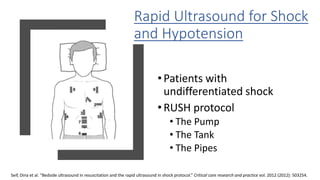
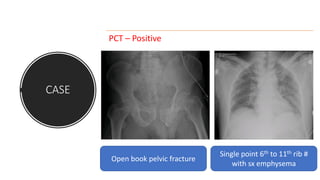
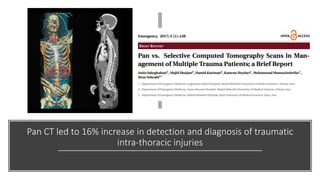
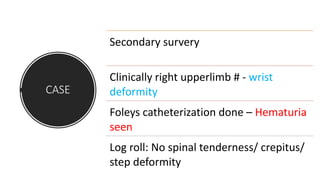
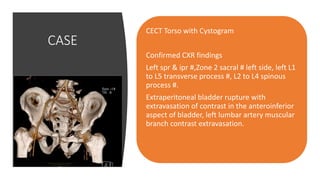
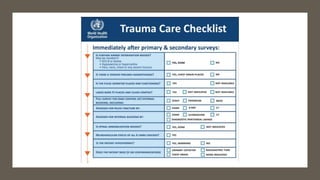
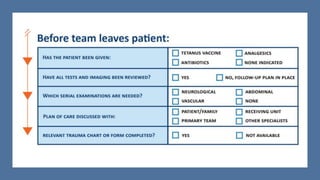
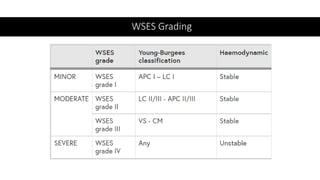
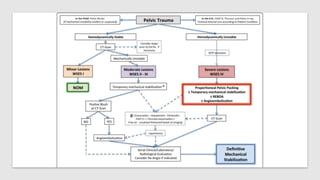
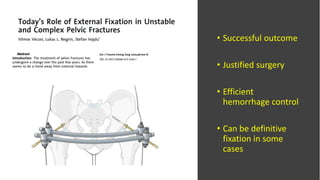
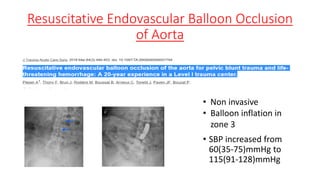
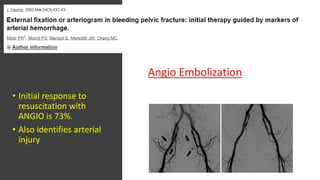
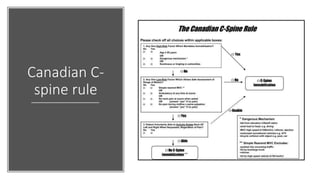
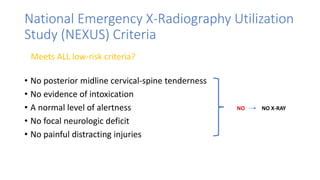
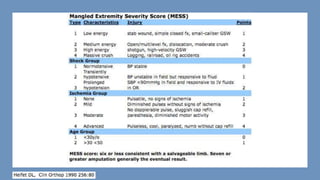
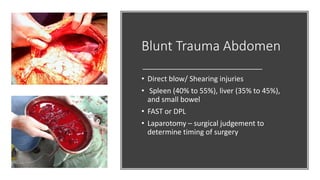
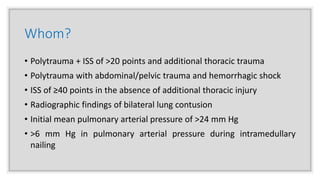
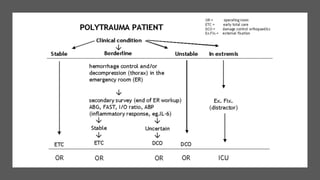
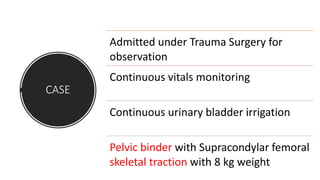
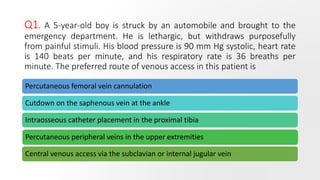
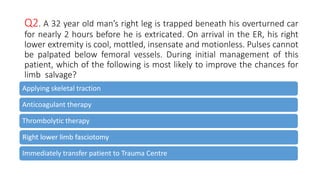
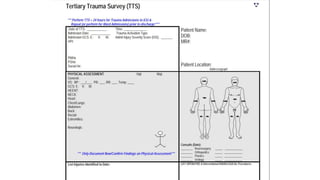
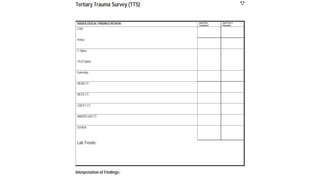
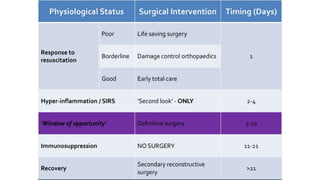
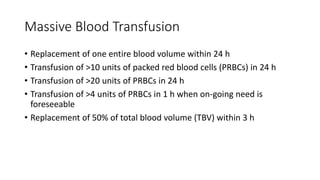
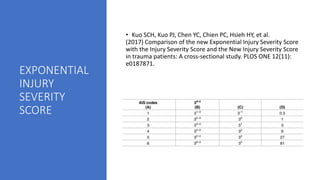
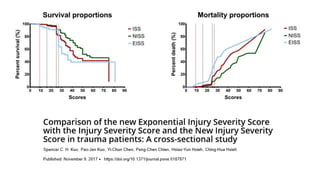
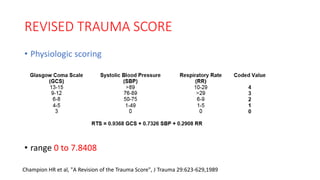
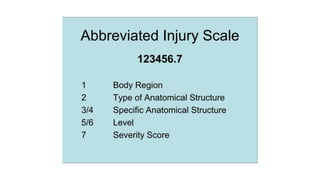
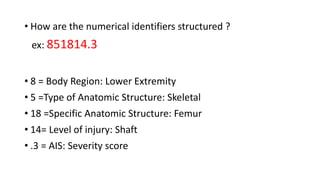
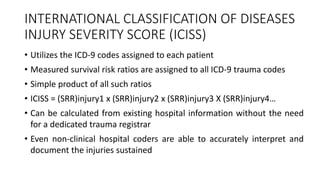
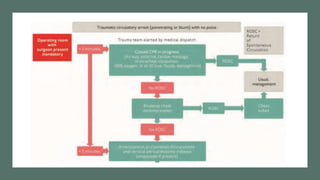
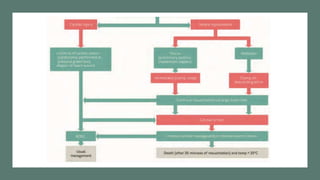
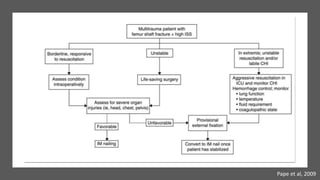
The document discusses resuscitation principles and advances in polytrauma management, highlighting key definitions and scoring systems like the Injury Severity Score (ISS) and Abbreviated Injury Scale (AIS). It covers the epidemiology of trauma, mechanisms of injury, and the importance of the 'golden hour' for patient outcomes, as well as the roles of trauma teams, emergency care protocols, and the significance of proper triage and resuscitation techniques. Additionally, it touches on management strategies for various types of trauma and injuries, emphasizing the need for timely and effective intervention to reduce mortality rates.