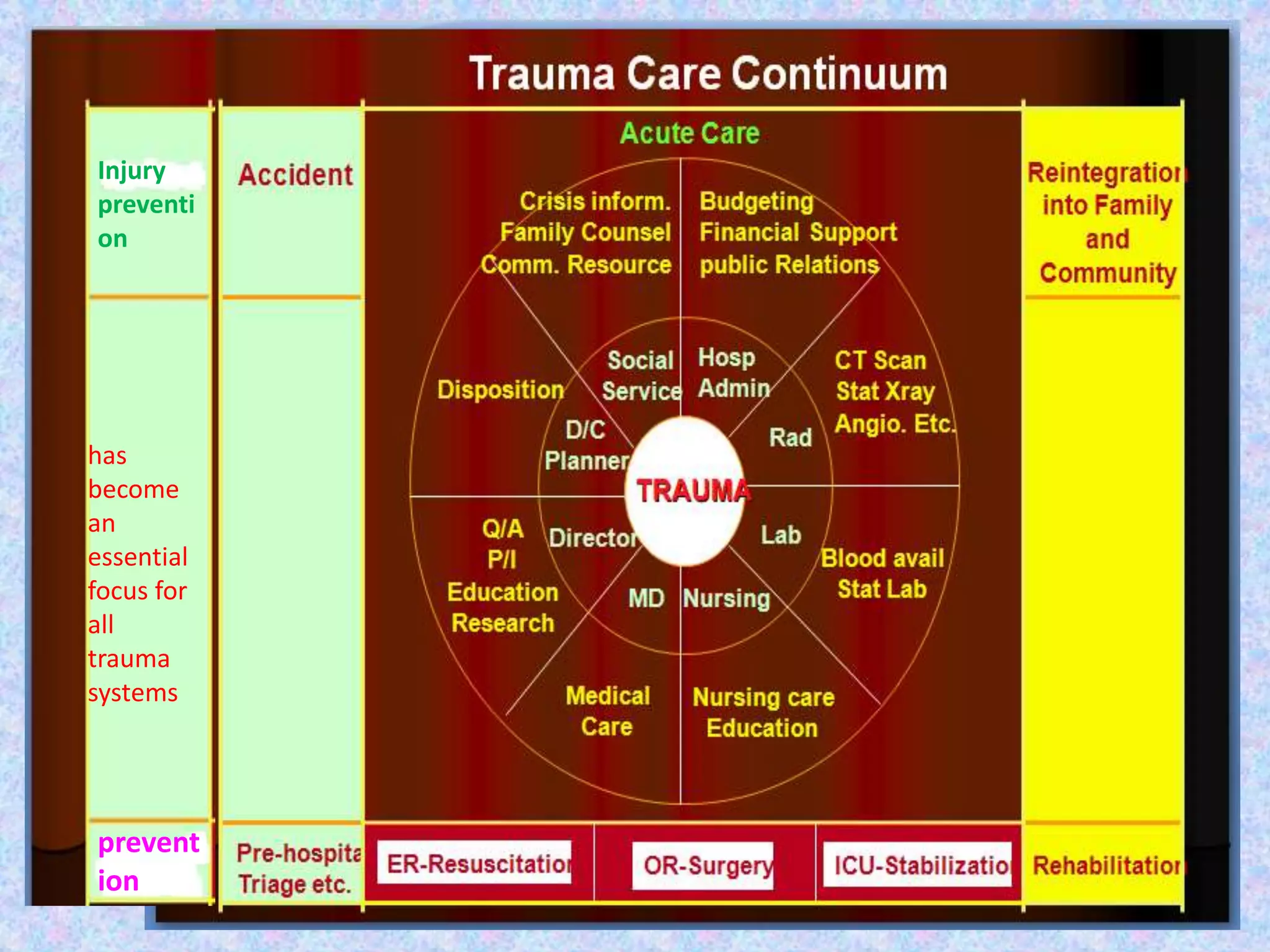
1. Trauma management involves coordinated care across multiple phases including pre-hospital care, acute care in the hospital, and post-hospital rehabilitation.
2. In the hospital, trauma is initially managed by an organized trauma team using an approach focused on treatment before diagnosis and stabilization of vital organs.
3. Further care involves additional phases like damage control surgery to rapidly control bleeding and contamination followed by intensive care, as well as definitive later surgeries once the patient is stabilized. The goal is to prevent death from hemorrhaging, hypothermia, coagulopathy and metabolic acidosis.

























![Advanced life support is provided
[by an organized trauma team]
Early hospital phase:](https://image.slidesharecdn.com/currenttraumamanagtraumasystem-161016213551/75/Current-trauma-manag-trauma-system-33-2048.jpg)