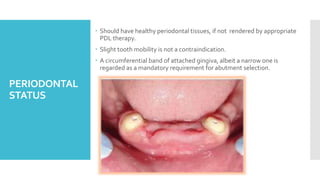
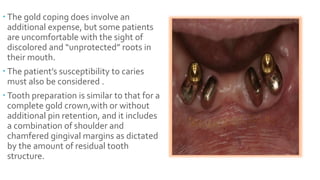
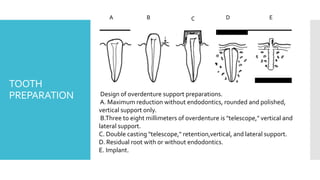
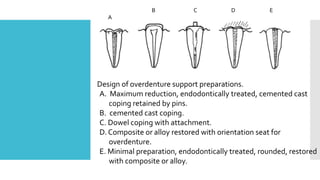
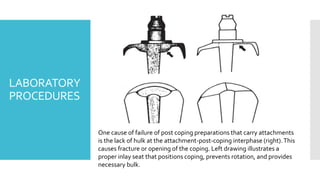
The document discusses tooth-supported overdentures, emphasizing their role in preventive prosthodontics and addressing issues of occlusal stability and esthetics in patients with compromised dental arches. It outlines the advantages and disadvantages of overdentures, selection of abutment teeth, preparation and impression techniques, and attachment systems, highlighting both the technical challenges and long-term benefits of this therapy. The use of overdentures can lead to favorable outcomes, especially with advancements like osseointegration for better stability.