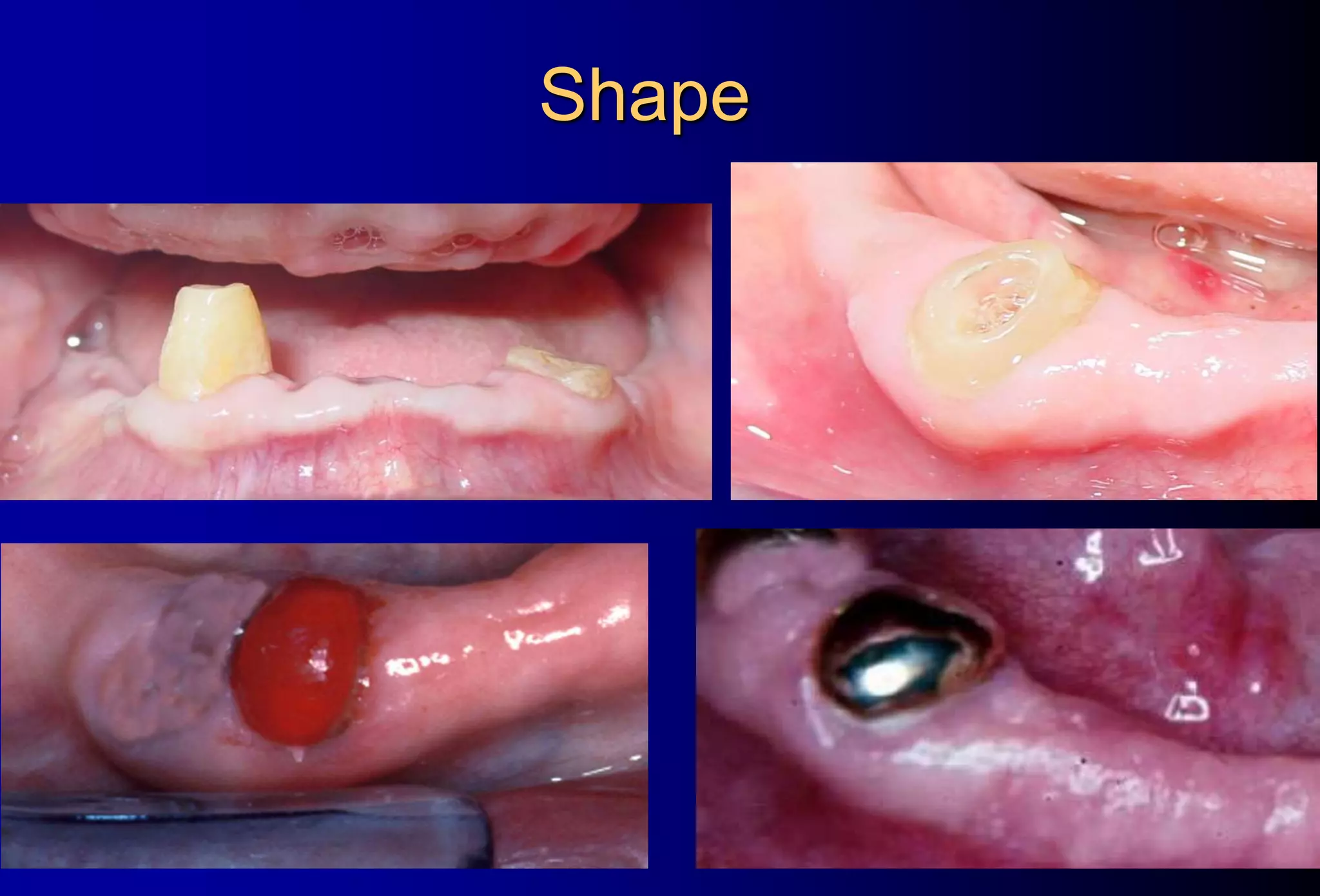
This document provides information on overdentures, including definitions, types, indications, advantages, and disadvantages. An overdenture is a removable dental prosthesis that covers and rests on remaining natural teeth, roots, and/or dental implants. Key advantages discussed are the preservation of remaining teeth and alveolar bone, enhanced support, stability, and retention, improved patient acceptance, and the ability to perform conventional dental procedures. Potential disadvantages include increased risk of caries and periodontal disease of abutment teeth, requiring more interarch space, and being more expensive and time consuming. Factors like adequate bone support, endodontic health, and adequate spacing of teeth are discussed in selecting teeth for overdentures.