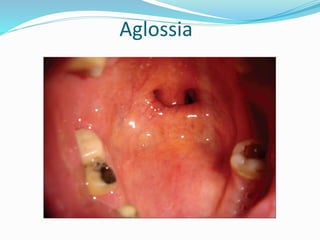
The document describes various normal anatomical structures and abnormalities that can present on the tongue, including different types of papillae, taste buds, and developmental variations. It then discusses many potential clinical findings involving the tongue related to deficiencies, infections, tumors, and other oral diseases. Specific conditions covered in detail include hairy tongue, leukoplakia, geographic tongue, candidiasis, macroglossia, ulcers, deviations and ties. Multiple images are also provided to illustrate key pathologies.