The document discusses toe to thumb transfer as an option for thumb reconstruction. It provides details on:
- The anatomy of the toe making it suitable for transfer, including its skeletal structure, tendons, skin, and nerves
- The history of toe to thumb transfer, including early experiments and the first microsurgical procedure
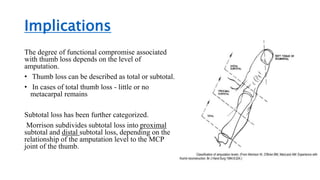
- Causes of thumb loss that may require reconstruction
- Preoperative assessment and considerations for candidates, including smoking cessation
- Surgical technique for both hand and toe dissection to prepare the structures for microvascular anastomosis