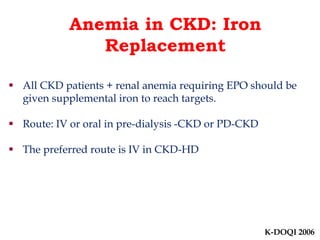
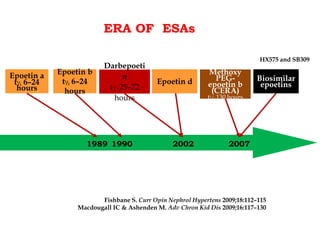
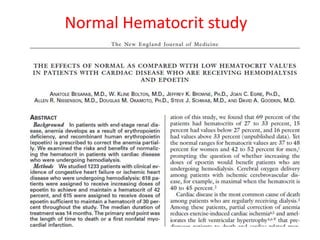
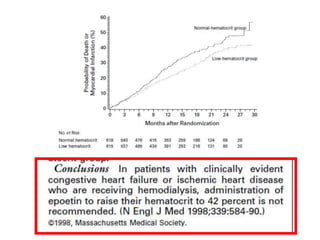
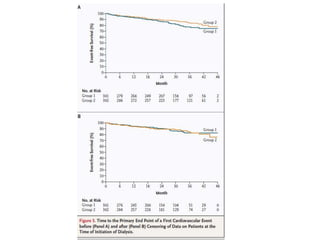
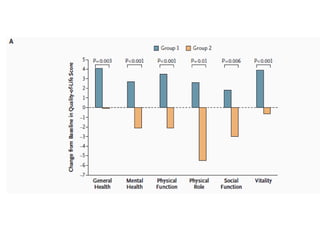
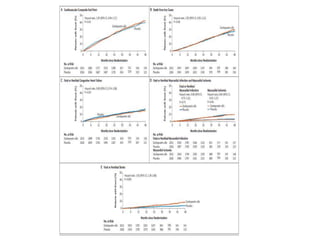
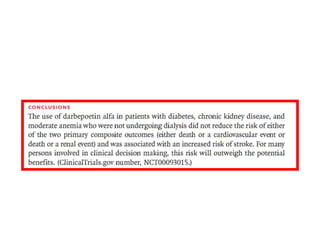
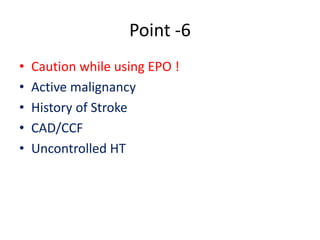
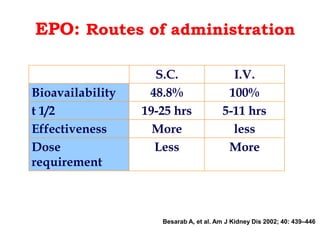
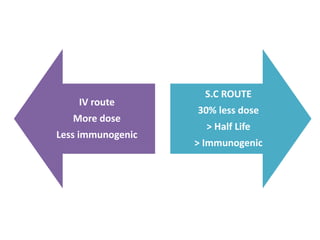
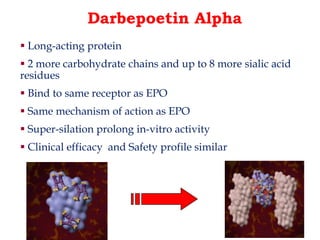
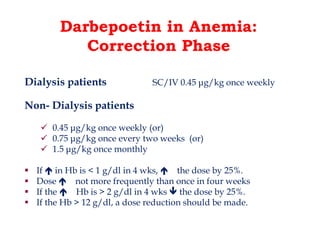
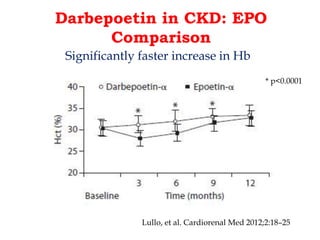
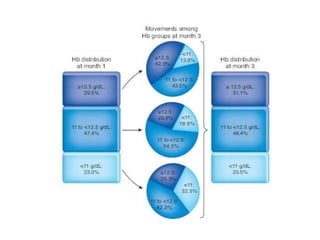
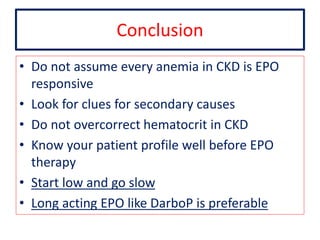
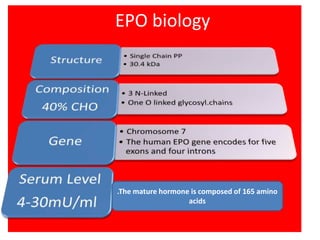
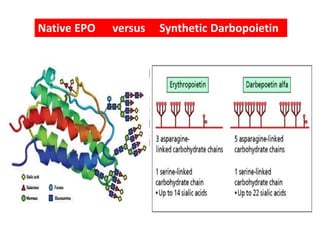
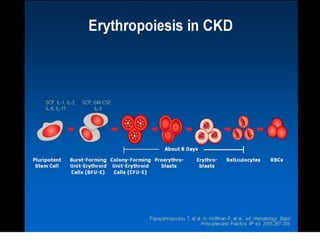
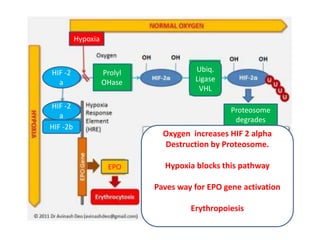
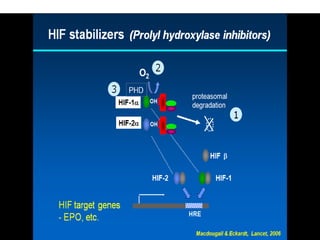
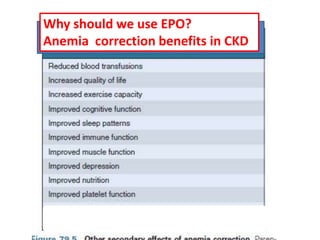
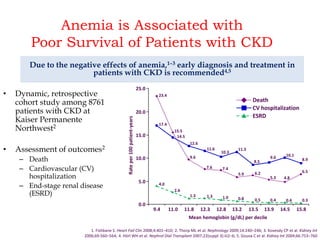
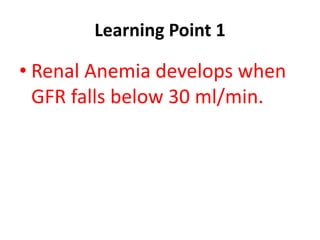
The document discusses the biology and clinical use of erythropoietin (EPO), emphasizing its production in kidneys, management strategies for anemia in chronic kidney disease (CKD), and major clinical trial findings. It highlights the importance of EPO in improving patient outcomes in CKD and the need for careful monitoring and dosing to avoid complications. Additionally, it addresses cautionary notes regarding EPO use in specific patient populations and the advantages of long-acting EPO formulations like darbopoietin.
![Focus of my talk
• Biology of Erythropoietin [EPO]
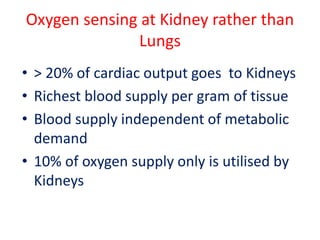
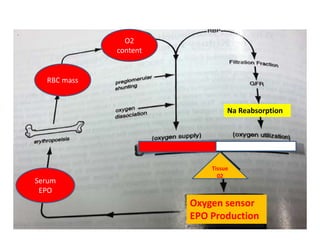
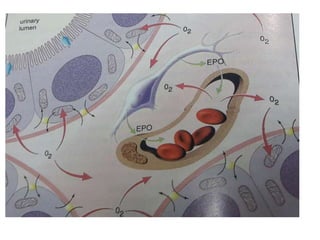
• Why EPO should come from Kidneys? Why
not Lungs ?
• Practical aspects of usage of EPO in clinic
• Major clinical trials
• Use / Abuse of EPO
• Conclusion](https://image.slidesharecdn.com/epo-141203195507-conversion-gate01/85/Erythropoetin-From-Bench-to-Bedside-2-320.jpg)
![Bioengineered EPO possible only with mammalian cell lines
due to addtion of Sugar moiety
[Unlike Insulin for which bacteria can be utilised]](https://image.slidesharecdn.com/epo-141203195507-conversion-gate01/85/Erythropoetin-From-Bench-to-Bedside-4-320.jpg)
![Focus of my talk
• Biology of Erythropoietin [EPO]
• Why EPO is produced in Kidneys
• Practical aspects of usage of EPO in clinic
• Major clinical trials
• Cautionary notes
• Conclusion](https://image.slidesharecdn.com/epo-141203195507-conversion-gate01/85/Erythropoetin-From-Bench-to-Bedside-12-320.jpg)

![Point 3
• Pure Renal anemia is
• Normocytic
• Normochromic
Either a low[Fe] or high MCV[B12,F]
Low MCH or MCHC strongly
suggest other contributory factors
[ Iron def or hemoglobinopathy]](https://image.slidesharecdn.com/epo-141203195507-conversion-gate01/85/Erythropoetin-From-Bench-to-Bedside-30-320.jpg)