Venothromboembolism during pregnancy and puerperium
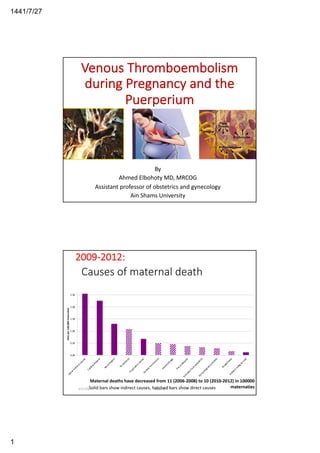
- 1. 27/7/1441 1 Venous Thromboembolism during Pregnancy and the Puerperium By Ahmed Elbohoty MD, MRCOG Assistant professor of obstetrics and gynecology Ain Shams University Causes of maternal death 0.00 0.50 1.00 1.50 2.00 2.50 OtherIndirectcauses Cardiacdisease Neurological Throm bosis PsychiatriccausesGenitaltractsepsis Haem orrhage Pre-eclam psia Am nioticfluid em bolism Earlypregnancydeaths AnaesthesiaIndirectm alignancies Rateper100,000maternities 3/21/20 elbohotySolid bars show indirect causes, hatched bars show direct causes Maternal deaths have decreased from 11 (2006-2008) to 10 (2010-2012) in 100000 maternaties 2009-2012:
- 4. 27/7/1441 4 2013-2015 3/21/20elbohoty7 December 2018 (2014-16) 3/21/20 elbohoty Indirect causes: 56% Direct causes: 44%
- 5. 27/7/1441 5 Causes of maternal death 2015- 2017 in UK 3/21/20 ELBOHOTY 9 Long term sequaelae of VTE •35% venous insufficiency 3-10 years later •65% further DVT / venous insufficiency later life in affected leg vs 22% unaffected 3/21/20 elbohoty
- 6. 27/7/1441 6 VTE increases CV diseases 3/21/20 elbohoty Incidence •Absolute incidence of VTE in pregnancy and the puerperium is 1 per 100 0 person-years •The UK incidence of PE is 1.3 per 10 000 maternities. 3/21/20 elbohoty
- 7. 27/7/1441 7 3/21/20 elbohoty Normal hemostasis • Disruption of vascular endothelial lining allows exposure of blood to • subendothelial connective tissue: • Primary hemostasis (seconds) • Platelet plug formation at site of injury • Stops bleeding from capillaries, small • arterioles and venules • Secondary hemostasis (minutes) • Fibrin formation by reactions of • the plasma coagulation system 3/21/20 elbohoty
- 9. 27/7/1441 9 Coagulation Inhibitors: In addition to the clotting factors there are many substances that inhibits coagulation: -Anti- thrombin III (AT III) -Alpha 2 globulin inhibits Thrombin & factors Xa, XIIa ,XIa and IXa. -Protein C (endothelial cell ) . -Protein S (endothelial cell & platelets ) . 3/21/20 elbohoty 3/21/20 ELBOHOTY 18
- 10. 27/7/1441 10 3/21/20 elbohoty Protein C and Protein C Deficiency • Protein C is a vitamin K dependent glycoprotein produced in the liver • In the activation of protein C, thrombin binds to thrombomodulin, a structural protein on the endothelial cell surface • This complex then converts protein C to activated protein C (APC), which degrades factors Va and VIIIa, limiting thrombin production • For protein C to bind, cleave and degrade factors Va and VIIIa, protein S must be available • Protein C deficiency, whether inherited or acquired, may cause thrombosis when levels drop to 50% or below • Protein C deficiency also occurs with surgery, trauma, pregnancy, OCP, liver or renal failure, DIC,or warfarin
- 11. 27/7/1441 11 3/21/20 elbohoty Pregnancy-Associated Changes in Hemostatic and Fibrinolytic Proteins Increase in Clotting Factors: 20 to 200% increase in levels of fibrinogen and factors II, VII, X, VIII and XII Decrease in Anticoagulant and Fibrinolytic Activity: Protein S levels (free and total) decrease by 40% PAI-1 levels increase two to three-fold in pregnancy 3/21/20 elbohoty
- 12. 27/7/1441 12 v 3/21/20 elbohoty Pathogenesis of VTE in Pregnancy Hyper- coagulability Vascular Damage Venous Stasis 3/21/20 elbohoty
- 13. 27/7/1441 13 3/21/20 elbohoty Thrombosis Hereditary thrombophilia Acquired thrombophilia Surgery traumaImmobility Inflammation Malignancy Estrogens Risk Factors for Thrombosis Atherosclerosis
- 14. 27/7/1441 14 3/21/20 elbohoty Score Risk for VTE • All women should undergo a documented assessment of risk factors for VTE in • prepregnancy • early pregnancy • admitted to hospital • intrapartum • immediately postpartum 3/21/20 elbohoty
- 15. 27/7/1441 15 Time of prophylaxis • Many fatal antenatal VTE events occur in the first trimester and therefore prophylaxis for women with previous VTE should begin early in pregnancy. • The risk for VTE increases with gestational age, reaching a maximum just after delivery. • The relative risk postpartum is five-fold higher compared to antepartum. 3/21/20 elbohoty 3/21/20 elbohoty
- 16. 27/7/1441 16 incidence of VTE per 10,000 deliveries by postpartum week • 9.2 for week 1 • 2.42 for week 2 • 1.43 for week 3 • 0.94 for week 4 • 0.56 for week 5 • 0.11-0.34 for weeks 6-12 3/21/20 elbohoty 3/21/20 elbohoty
- 17. 27/7/1441 17 Evidence •Available evidence does not allow an accurate risk estimation of VTE to be determined from combinations of the different risk factors. •Therefore, as a pragmatic approach to women with risk factors (except previous VTE) 3/21/20 elbohoty Score Risk for VTE • If admitted to hospital antenatally (18-fold increased risk of first VTE) consider thromboprophylaxis. • If prolonged admission (≥ 3 days) or readmission to hospital within the puerperium consider thromboprophylaxis 3/21/20 elbohoty MangementRisk Recommend antenatal high-dose LMWH and at least 6 weeks’ postnatal LMWH or until switched back to oral anticoagulant therapy > 4 antenatally antenatal prophylactic LMWH and at least 6 weeks’ postnatal LMWH 4 antenatally thromboprophylaxis from 28 and at least 6 weeks’ postnatal LMWH weeks 3 antenatally thromboprophylaxis for at least 10 days≥ 2 postnatally
- 18. 27/7/1441 18 > 4 • Previous VTE + • Antithrombin deficiency • APS • Other Thrombophilia • offered thromboprophylaxis with higher dose LMWH (either 50%, 75% or full treatment dose) antenatally and for 6 weeks postpartum or until returned to oral anticoagulant therapy after delivery. • Pregnant women with APS and prior VTE or arterial thromboses should be managed in collaboration with a haematologist and/or rheumatologist with expertise in this area. 3/21/20 elbohoty 4 •Previous VTE (except a single event related to major surgery) •Antithrombin deficiency •OHSS (first trimester only) 3/21/20 elbohoty
- 19. 27/7/1441 19 3 • Previous VTE provoked by major surgery • Known high-risk thrombophilia • protein C & protein S deficiency • homozygous factor V Leiden • homozygous prothrombin gene mutation • compound heterozygotes • Medical comorbidities e.g. cancer, heart failure; active systemic lupus erythematosus, inflammatory polyarthropathy or inflammatory bowel disease; nephrotic syndrome; type I diabetes mellitus with nephropathy; sickle cell disease; current intravenous drug user • Any surgical procedure in pregnancy or puerperium except immediate repair of the perineum, e.g. appendicectomy, postpartum sterilisation • Hyperemesis (during hospital admission) 3/21/20 elbohoty 2 • BMI > 40 • Caesarean section in labour • Thalathemia 3/21/20 elbohoty
- 20. 27/7/1441 20 1 • Family history of unprovoked or estrogen-related VTE in first-degree relative • Asymptomatic low-risk thrombophilia (no VTE) • heterozygous prothrombin gene mutation • heterozygous factor V Leiden • Sickle cell trait • Asymptomatic APS antibodies (NO VTE, NO collagen diseases) • Age (> 35 years) • BMI > 30 but < 40 • Parity ≥ 3 • Smoker • Gross varicose veins • Pre-eclampsia in current pregnancy • ART/IVF (antenatal only) • Multiple pregnancy • Elective caesarean section • Mid-cavity or rotational operative delivery • Prolonged labour (> 24 hours) • PPH (> 1 litre or transfusion) • Preterm birth < 37+0 weeks in current pregnancy • Stillbirth in current pregnancy • Current systemic infection • Immobility, dehydration • Long travel> 4 hours3/21/20 elbohoty Summary 3/21/20 elbohoty
- 21. 27/7/1441 21 Thromboprophylaxis in women with previous VTE and/or thrombophilia 3/21/20 elbohoty Thrombophilia • Inherited • Acquired • Lupus anticoagulant • ß2-glycoprotein antibodies Anticardiolipin antibodies 3/21/20 elbohoty
- 22. 27/7/1441 22 Inherited thrombophilias: • Activated protein C (APC) resistance • factor V Leiden mutation • Prothrombin G20210A mutation • Antithrombin deficiency • Protein C deficiency • Protein S deficiency • Factor XIII mutation Hereditary 3/21/20 elbohoty
- 23. 27/7/1441 23 Screening Evaluation to detect thrombophilia • Test for Factor V Leiden • Genetic test for prothrombin gene mutation 20210A • Functional assay of antithrombin III • Functional assay of protein C • Functional assay of protein S • Testing for Anti-phospholipid antibody syndrome : Clotting test for lupus anticoagulant ( mixing studies, DRVVT, STACLOT-LA) /ELISA for cardiolipin antibodies. A complete hypercoagulability work – up as above is recommended in strongly thrombophilic patients. Antithrombin deficiency • 70-90% life-time risk of VTE • prevalence 1/3000 • accounts for 2-20% of VTE in pregnancy • > 50 fold increase risk of VTE in pregnancy • 50% risk of VTE per pregnant patient 3/21/20 elbohoty
- 24. 27/7/1441 24 Anticoagulation in Antithrombin deficiency • It should be undertaken in collaboration with a haematologist with expertise in thrombosis in pregnancy with anti-Xa monitoring and the potential for antithrombin replacement at initiation of labour or prior to caesarean section. • If anti-Xa levels are measured, a test that does not use exogenous antithrombin should be used and 4-hour peak levels of 0.5–1.0 iu/ml aimed for. • Heparins may not be as effective in antithrombin deficiency as their mode of action is antithrombin-dependent. 3/21/20 elbohoty Factor VLeiden mutation 30% life-time risk of VTE for homozygos prevalence > 5 % in European population 10-fold increase risk of VTE in pregnancy Risk of VTE in asympt. heterozygotes= 0.2% Risk of VTE in homozygotes= 16 to 17% 3/21/20 elbohoty
- 25. 27/7/1441 25 ProthrombinG20210A mutation 30% life-time risk of VTE for homozygos prevalence 2 % in European population 15-fold increase risk of VTE in pregnancy Risk of VTE in heterozygotes = 0.5% Risk of VTE in homozygotes = 15% Risk with compound heterozygotes = 4-10% 3/21/20 elbohoty Protein C Deficiency: Life-time risk of VTE > 30% Prevalence is 0.2-0.5% > 20-fold increased risk of VTE Risk of VTE in pregnancy is 4% 3/21/20 elbohoty
- 26. 27/7/1441 26 Protein S Deficiency • Life-time risk of VTE > 30% • Prevalence of primary deficiency is 0.08%; of acquired deficiency is 7% • > 20-fold increase risk of VTE • Risk of VTE in pregnancy is 4% 3/21/20 elbohoty Hyperhomocystinemia in Thrombophilia § In the past, homocysteine levels were recommended in thrombophilic patients. § Measurement of fasting total plasma homocysteine is no longer recommended § There are no data supporting a change in the duration or type of therapy for a patient with hyperhomocysteinemia and a past history of VTE, since hyperhomocysteinemia may be a marker of thrombotic disease rather than a cause. § Results from the Leiden MEGA study indicate that the presence of methylenetetrahydrofolate reductase (MTHFR) mutation which mildly increases homocysteine levels, is not associated with an increased risk for venous thrombosis. § Hence, there is no clinical rationale for measurement of plasma homocysteine levels or for assaying for presence of the MTHFR mutation when screening for the risk of VTE.
- 27. 27/7/1441 27 Previous recurrent VTE • Advice from a clinician with expertise in haemostasis and pregnancy. • Some women may require higher doses of LMWH. • Women on long-term warfarin or other oral anticoagulants should be counselled about the risks of these agents to the fetus and advised to stop their oral anticoagulant therapy and change to LMWH as soon as pregnancy is confirmed, ideally within 2 weeks of the missed period and before the sixth week of pregnancy. • Women not on warfarin or other oral anticoagulants should be advised to start LMWH as soon as they have a positive pregnancy test. 3/21/20 elbohoty Testing for thrombophilia • Prior to testing; women should be counselled regarding the implications for themselves and family members of a positive or negative result. • The results should be interpreted by clinicians with specific expertise in the area. 3/21/20 elbohoty
- 28. 27/7/1441 28 •A family history of an unprovoked or estrogen- provoked VTE in a first-degree relative when aged under 50 years. •A family history of VTE and either antithrombin deficiency or where the specific thrombophilia has not been detected should be tested for antithrombin deficiency. •Women with an unprovoked VTE should be tested for the presence of antiphospholipid antibodies. 3/21/20 elbohoty ` 3/21/20 elbohoty
- 29. 27/7/1441 29 3/21/20 elbohoty Which agents should be used for thromboprophylaxis? • Anti-embolism stockings • Low-molecular-weight heparin (LMWH) • Unfractionated heparin • Hepranoids • Warfarin • Oral thrombin and Xa inhibitors • Aspirin • Dextran 3/21/20 elbohoty
- 30. 27/7/1441 30 Anti-embolism stockings • The use of properly applied anti-embolism stockings (AES) of appropriate size and providing graduated compression with a calf pressure of 14–15 mmHg is recommended in pregnancy and the puerperium for women who are 1. More than four risk factors antenatally 2. More than two risk factors postnatally 3. Previous VTE 4. Hospitalised and have a contraindication to LMWH. 5. Women travelling long distance for more than 4 hours. 3/21/20 elbohoty Low-molecular-weight heparin (LMWH) • LMWHs are the agents of choice for antenatal and postnatal thromboprophylaxis. • Doses of LMWH are based on weight (booking or most recent weight can be used to guide dosing). • It is only necessary to monitor the platelet count if the woman has had prior exposure to unfractionated heparin (UFH). • Monitoring of anti-Xa levels is not required when LMWH is used for thromboprophylaxis. • Doses of LMWH should be reduced in women with renal impairment. • LMWH is safe in breastfeeding. 3/21/20 elbohoty
- 31. 27/7/1441 31 Doses 3/21/20 elbohoty Contraindications/cautions to LMWH use • Known bleeding disorder (e.g. haemophilia, von Willebrand’s disease or acquired coagulopathy) • Active antenatal or postpartum bleeding • Women considered at increased risk of major haemorrhage (e.g. placenta praevia) • Thrombocytopenia (platelet count < 75 × 109/l) • Acute stroke in previous 4 weeks (haemorrhagic or ischaemic • Severe renal disease (glomerular filtration rate [GFR] < 30 ml/minute/1.73m2) • Severe liver disease (prothrombin time above normal range or known varices) • Uncontrolled hypertension (blood pressure > 200 mmHg systolic or > 120 mmHg diastolic)3/21/20 elbohoty
- 32. 27/7/1441 32 Unfractionated heparin • In women at very high risk of thrombosis, UFH may be used peripartum in preference to LMWH where there is an increased risk of haemorrhage or where regional anaesthetic techniques may be required as it has a shorter half-life than LMWH and there is more complete reversal of its activity by protamine sulfate. • So, for example, if no LMWH has been given for 24 hours but the woman has not yet delivered and there is concern about delaying further doses of anticoagulants, a prophylactic dose of 5000 iu subcutaneously of UFH could be used and repeated every 12 hours until LMWH can be resumed after delivery.3/21/20 elbohoty •The required interval between a prophylactic dose of UFH and regional analgesia or anaesthesia is less (4 hours) than with LMWH (12 hours) and there is less concern regarding neuraxial haematomas with UFH. •The platelet count should be monitored every 2–3 days from days 4–14 or until heparin is stopped as any exposure to UFH is associated with an increased risk of HIT. 3/21/20 elbohoty
- 33. 27/7/1441 33 Heparin side effects • In most of cases are minor 40% of women • local skin reactions (pain, itching, swelling, bruising) • an increased risk of bleeding • heparin-induced thrombocytopenia • osteopenia or osteoporotic fractures • precluding epidural analgesia if not discontinued in time. Danaparoid • Potential use of danaparoid should be in conjunction with a consultant haematologist with expertise in haemostasis and pregnancy. • Danaparoid is a heparinoid that is mostly used in patients intolerant of heparin, either because of HIT or a skin allergy to heparins. • There were no adverse fetal outcomes attributed to danaparoid. • The half-life of danaparoid is long (24 hours) and regional anaesthesia should be avoided in women receiving it for thromboprophylaxis. • Breastfeeding would be safe while on danaparoid since little if any appears in breast milk and oral absorption is unlikely. 3/21/20 elbohoty
- 34. 27/7/1441 34 Fondaparinux • Fondaparinux should be reserved for women intolerant of heparin compounds. • Fondaparinux use in pregnancy should be in conjunction with a consultant haematologist with expertise in haemostasis and pregnancy. • Fondaparinux is a synthetic pentasaccharide that acts through inhibition of factor Xa via antithrombin. • It is licensed in the UK for the prevention and treatment of VTE outside pregnancy • There is limited experience of its use in pregnancy but it has been used in the setting of heparin intolerance with no reported hypersensitivity reactions or adverse effects on the fetus. • No adverse effects were observed in the newborns. It does not seem necessary to alter the dose in pregnancy. • It is unknown whether fondaparinux is excreted in breast milk but oral absorption seems unlikely. • The half-life of fondaparinux is long (18 hours) and 36–42 hours should pass following the previous dose before it becomes acceptable to consider regional anaesthesia.3/21/20 elbohoty Warfarin • Warfarin use in pregnancy is restricted to the few situations where heparin is considered unsuitable, e.g. some women with mechanical heart valves. • Women receiving long-term anticoagulation with warfarin can be converted from LMWH to warfarin postpartum when the risk of haemorrhage is reduced, usually 5–7 days after delivery. • Warfarin is safe in breastfeeding. 3/21/20 elbohoty
- 35. 27/7/1441 35 Antenatal risks • Warfarin crosses the placenta leading to an increased risk of congenital abnormalities including a characteristic warfarin embryopathy in approximately 5% of fetuses exposed between 6 and 12 weeks of gestation • hypoplasia of nasal bridge • congenital heart defects • Ventriculomegaly • agenesis of the corpus callosum • stippled epiphyses. • It is dose-dependent with a higher incidence in women taking greater than 5 mg/ day. • It also increase the risk of spontaneous miscarriage, stillbirth, neurological problems in the baby and fetal and maternal haemorrhage. 3/21/20 elbohoty Postnatal risks • Warfarin can be safely used following delivery from day 5 and in breastfeeding mothers, although it requires close monitoring and visits to an anticoagulant clinic and carries an increased risk of postpartum haemorrhage and perineal haematoma compared with LMWH. • It is not appropriate for those women requiring only 10 days’ postpartum prophylaxis. However, it is appropriate for those on maintenance warfarin outside pregnancy. 3/21/20 elbohoty
- 36. 27/7/1441 36 Oral thrombin and Xa inhibitors • Non-vitamin K antagonist oral anticoagulants (NOACs) should be avoided in pregnant women & women who are breastfeeding. • such as dabigatran, rivaroxaban and apixaban work through direct inhibition of thrombin or factor Xa. • The effects last approximately 8–12 hours, but factor Xa activity does not return to normal within 24 hours so once- daily dosing is possible. • If an invasive procedure or surgical intervention is required, Xarelto 20 mg should be stopped at least 24 hours before the intervention, if possible and based on the clinical judgement of the physician. 3/21/20 elbohoty Low-dose aspirin • Aspirin is not recommended for thromboprophylaxis in obstetric patients. 3/21/20 elbohoty
- 37. 27/7/1441 37 Dextran • Dextran should be avoided antenatally and intrapartum because of the risk of anaphylactoid reaction. • Although dextran may reduce the risk of postoperative DVT outside pregnancy, the evidence is weak, it is less effective than LMWH and it appears to increase the risk of bleeding. • Anaphylaxis to dextran has been associated with uterine hypertonus, fetal distress, fetal neurological abnormalities and death. 3/21/20 elbohoty When should thromboprophylaxis be started? • Antenatal thromboprophylaxis for those with previous VTE should begin as early in pregnancy as practical. • Women without previous VTE and without particular first trimester risk factors or admission to hospital, but with four other risk factors, should be considered for antenatal prophylaxis throughout pregnancy. • Women without previous VTE and without particular first trimester risk factors or admission to hospital, but with three other risk factors, can start antenatal prophylaxis at 28 weeks of gestation. 3/21/20 elbohoty
- 38. 27/7/1441 38 What are the first trimester risk factors for VTE and how should they be managed? • Women admitted with hyperemesis should be considered for thromboprophylaxis with LMWH and can discontinue thromboprophylaxis when the hyperemesis resolves. • Women with ovarian hyperstimulation syndrome should be considered for thromboprophylaxis with LMWH in the first trimester. • Women with an IVF pregnancy and three other risk factors should be considered for thromboprophylaxis with LMWH starting in the first trimeste 3/21/20 elbohoty When should thromboprophylaxis be interrupted for delivery? • Women receiving antenatal LMWH should be advised that if they have any vaginal bleeding or once labour begins they should not inject any further LMWH. • They should be reassessed on admission to hospital and further doses should be prescribed by medical staff. • Regional techniques should be avoided if possible until at least 12 hours after the previous prophylactic dose of LMWH. • LMWH should not be given for 4 hours after use of spinal anaesthesia or after the epidural catheter has been removed and the catheter should not be removed within 12 hours of the most recent injection.3/21/20 elbohoty
- 39. 27/7/1441 39 • When a woman presents while on a therapeutic regimen of LMWH, regional techniques should be avoided if possible for at least 24 hours after the last dose of LMWH. • The first thromboprophylactic dose of LMWH should be given as soon as possible after delivery provided there is no postpartum haemorrhage and regional analgesia has not been used. • In some women, particularly those on high-dose prophylactic or treatment doses of LMWH, there may be an indication for induction of labour to help plan thromboprophylaxis around delivery and facilitate a 24-hour window between the last dose of LMWH and regional analgesia. • If LMWH precludes regional techniques (in, for example, the woman who presents in spontaneous labour within 12 hours of taking a LMWH dose), alternative analgesia such as opiate-based intravenous patient-controlled analgesia can be offered.3/21/20 elbohoty Guidance for regional block in patients taking drugs affecting haemostasis 3/21/20 elbohoty
- 40. 27/7/1441 40 Women at high risk of haemorrhage • Risks: • major antepartum haemorrhage • Coagulopathy • progressive wound haematoma • suspected intra-abdominal bleeding and postpartum haemorrhage • Management: • Anti-embolism stockings (AES), foot impulse devices or intermittent pneumatic compression devices. • Thromboprophylaxis should be started or reinstituted as soon as the immediate risk of haemorrhage is reduced (Unfractionated heparin (UFT) may also be considered). • If a woman develops a haemorrhagic problem while on LMWH the treatment should be stopped and expert haematological advice sought. 3/21/20 elbohoty Example • If LMWH is routinely prescribed at 6 p.m., this allows for an elective caesarean section the next morning, removal of the epidural catheter before 2 p.m. and a first postnatal dose of LMWH at 6 p.m. the same day. 3/21/20 elbohoty
- 41. 27/7/1441 41 Thromboembolic Disease in Pregnancy and the Puerperium: Acute Management 3/21/20 elbohoty 3/21/20 elbohoty
- 42. 27/7/1441 42 • 40 years P5 BMI 33 pregnant at 30 weeks was admitted because of Acute pyelonephritis. On the 2nd day of admission: pain, swelling and redness in the left calf muscles. • What is the appropriate management: • A. perform D dimer & LL duplex • B. Start HMWH prohylactic dose& do LL duplex • C. Start HMWH therapeutic dose& do LL duplex • D Start LMWH prohylactic dose and do LL duplex • E. . Start LMWH therapeutic dose and do LL duplex 3/21/20 elbohoty • You Started LMWH therapeutic dose and ordered LL duplex and the result was normal and you suspected cellulitis what is your next step: a. contiue therpeutic b. contiue therpeutic and repeat LL duplex c. stop therpeutic and repeat LL duplex d. Shift to prphylactic e. Shift to prphylactic and repeat LL duplex 3/21/20 elbohoty
- 43. 27/7/1441 43 • 40 years P5 BMI 33 pregnant at 30 weeks was admitted because of Acute pyelonephritis. On the 2nd day of admission: swelling and redness in the left calf muscles and sudden onset of dyspnea and chest pain. • What is the appropriate management: • A. perform D dimer & LL duplex • B. Start HMWH prohylactic dose& do LL duplex • C. Start LMWH therapeutic dose& do LL duplex • D Start LMWH therapeutic dose and do CTPA on chest • E. Start LMWH therapeutic dose and do V/Q scan 3/21/20 elbohoty • 40 years P5 BMI 33 pregnant at 30 weeks was admitted because of Acute pyelonephritis. On the 2nd day of admission: sudden onset of dyspnea and chest pain and examination of lower limbs was unremarkable • What is the appropriate management: • A. perform D dimer & LL duplex • B. Start HMWH prohylactic dose& do LL duplex • C. Start LMWH therapeutic dose& do LL duplex • D Start LMWH therapeutic dose and do CTPA on chest • E. . Start LMWH therapeutic dose and do V/Q scan 3/21/20 elbohoty
- 44. 27/7/1441 44 Suggestive symptoms and signs of DVT: • unilateral leg pain(reflecting extension of thrombus into the pelvic vessels and/or development of a collateral circulation) • swelling, tenderness • increased temperature • pitting oedema • prominent superficial veins • Lower abdominal pain 3/21/20 elbohoty Suggestive symptoms and signs of PE: • Breathlessness, chest pain, haemoptysis, collapse, tachycardia, hypotension, tachypnoea, raised jugular venous pressure, focal signs in chest, hypoxia/cyanosis • A low-grade pyrexia and leucocytosis can occur with VTE 3/21/20 elbohoty
- 45. 27/7/1441 45 DD • Collapse 3/21/20 elbohoty 3/21/20 elbohoty
- 46. 27/7/1441 46 3/21/20 elbohoty Chest pain 3/21/20 elbohoty
- 48. 27/7/1441 48 Management on suspicion • Any woman with symptoms and/or signs suggestive of VTE should have • treatment with low-molecular-weight heparin (LMWH) given until the diagnosis is excluded by objective testing, unless treatment is strongly contraindicated. • objective testing performed expeditiously • blood should be taken for a full blood count, coagulation screen, urea and electrolytes, and liver function tests. • Performing a thrombophilia screen prior to therapy is not recommended. 3/21/20 elbohoty Investigation and initial management of suspected DVT in pregnancy and the puerperium 3/21/20 elbohoty
- 49. 27/7/1441 49 Investigations for the diagnosis of an acute DVT • Compression duplex ultrasound • If ultrasound is negative: • a low level of clinical suspicion, anticoagulant treatment can be discontinued. • a high level of clinical suspicion exists, anticoagulant treatment should be discontinued but the ultrasound should be repeated on days 3 and 7. • When iliac vein thrombosis is suspected (back and buttock pain and swelling of the entire limb), Doppler ultrasound of the iliac vein, magnetic resonance venography or conventional contrast venography may be considered 3/21/20 elbohoty on days 3 and 7 Lower Ext Doppler Exam 3/21/20 elbohoty Doppler U/S demonstrating non-compressible femoral vein with central clot.
- 50. 27/7/1441 50 3/21/20 elbohoty Upper extremity DVT • 11% of all DVTs in general population • Most case reports in pregnancy are following ART • Incidence after ART: 1/1200 cycles • 30% of cases not preceded by OHSS • Mean gestational age at presentation: 7 weeks • Diagnosis by ultrasound • Bilateral disease in 14% 3/21/20 elbohoty
- 51. 27/7/1441 51 Untreated DVT • If DVT remains untreated, 15–24% of these patients will develop PE. • PE during pregnancy may be fatal in almost 15% of patients, and in 66% of these, death will occur within 30 minutes of the embolic event. 3/21/20 elbohoty Diagnosis of VTE in pregnancy 3/21/20 elbohoty
- 52. 27/7/1441 52 Investigations for the diagnosis of an acute pulmonary embolism (PE) • Women presenting with symptoms and signs of an acute PE should have an electrocardiogram (ECG) and a chest X-ray (CXR) performed. • When the chest X-ray is abnormal and there is a clinical suspicion of PE, CTPA should be performed • For who have symptoms and signs of DVT, compression duplex ultrasound should be performed. If compression ultrasonography confirms the presence of DVT, no further investigation is necessary and treatment for VTE should continue. • For who have not any symptoms and signs of DVT, a ventilation/perfusion (V/Q) lung scan or a computerised tomography pulmonary angiogram (CTPA) should be performed. 3/21/20 elbohoty investigation and initial management of suspected PE in pregnancy and the puerperium 3/21/20 elbohoty
- 54. 27/7/1441 54 CXR • Chest X-ray (CXR) may identify other pulmonary disease such as pneumonia, pneumothorax or lobar collapse. • While the CXR is normal in over half of pregnant patients with objectively proven PE, abnormal features caused by PE include atelectasis, effusion, focal opacities, regional oligaemia or pulmonary oedema. 3/21/20 elbohoty Arterial Blood Gases Analysis • ABG analysis showed that only 10% had arterial P O2 levels less than 60 mmHg and 2.9% had oxygen saturation levels less than 90% • A respiratory alkalosis (PCO2 < 35mmHg). HOWEVER: • Other etiologies are more likely to lower the PO2 than is PE chronic obstructive pulmonary disease [COPD], pneumonia, CHF affect oxygen exchange more than PE. • 15% of patients with PE have a normal PO2 (>95%). 3/21/20 elbohoty
- 55. 27/7/1441 55 Electrocardiogram • the ECG was abnormal in 41% of women with acute PE; the most common abnormalities were • T wave inversion (21%) • S1Q3T3 pattern (15%) and right bundle branch block (18% during pregnancy and 4.2% in the puerperium) (Right Strain Pattern ) • Sinus tachycardia • Given the increasing incidence of ischaemic heart disease in pregnancy, the ECG may also be helpful in identifying alternative diagnoses. VQ versus CTPA
- 56. 27/7/1441 56 Ventilation / Perfusion Scanning • Good PPV (high probability scan) • Good NPV (normal scan) • Poor P/NPV (low, intermediate scans) 3/21/20 elbohoty Q V Q V / / • A Q scanning is probably the safest for the mother & fetus with a ventilation scan being performed only if the perfusion scan is abnormal. • Treatment should be continued when the V/Q scan reports a 'medium' or 'high' probability of PTE. 3/21/20 elbohoty
- 57. 27/7/1441 57 •Alternative or repeat testing should be carried out where V/Q scan or CTPA is normal but the clinical suspicion of PE remains. Anticoagulant treatment should be continued until PE is definitively excluded. •Women with suspected PE should be advised that, compared with CTPA, V/Q scanning may carry a slightly increased risk of childhood cancer but is associated with a lower risk of maternal breast cancer; in both situations, the absolute risk is very small. 3/21/20 elbohoty recent diagnosis • A SPECT scan is a type of nuclear imaging test, which means it uses a radioactive substance and a special camera to create 3-D pictures using gamma rays 3/21/20 elbohoty
- 58. 27/7/1441 58 massive pulmonary embolism (PE) • acute PE with any of the following sustained hypotension • systolic blood pressure < 90 mm Hg for ≥ 15 minutes or requiring inotropic support not due to a cause other than PE, such as arrhythmia, hypovolemia, sepsis, or left ventricular dysfunction • persistent profound bradycardia (heart rate < 40 beats per minute with signs or symptoms of shock) • pulselessness 3/21/20 elbohoty Massive life-threatening PE in pregnancy and the puerperium • Collapsed, shocked women who are pregnant or in the puerperium should be assessed and manged by a team of experienced clinicians including the on-call consultant obstetrician and other multidisciplinary team including senior physicians, obstetricians and radiologists. • The on-call medical team should be contacted immediately. • An urgent portable echocardiogram or CTPA within 1 hour of presentation should be arranged. 3/21/20 elbohoty
- 59. 27/7/1441 59 Cardiac Imaging in PE Normal PA Pressures Systolic Pressure 25mmHg Diastolic Pressure 10mmHg Mean PAP 20mmHg RV Failure (no prior CPD) Mean PAP > 40mmHg RV Strain (no prior CPD) Mean PAP 30-40mmHg with decreased CO 3/21/20 elbohoty Treatment • Intravenous unfractionated heparin is the preferred, initial treatment in massive PE with cardiovascular compromise. • If massive PE is confirmed, or in extreme circumstances prior to confirmation, immediate thrombolysis should be considered. • Women should be managed on an individual basis regarding: • intravenous unfractionated heparin • thrombolytic therapy or • thoracotomy and surgical embolectomy. 3/21/20 elbohoty
- 60. 27/7/1441 60 Evidence for use of thrombolysis during the pregnancy 3/21/20 elbohoty Additional therapies for VTE • In the initial management of DVT, the leg should be elevated and a graduated elastic compression stocking applied to reduce oedema. • Mobilisation with graduated elastic compression stockings should be encouraged. • Consideration should be given to the use of a temporary inferior vena cava filter in the peripartum period for patients with iliac vein VTE to reduce the risk of PE or in patients with proven DVT and who have recurrent PE despite adequate anticoagulation. 3/21/20 elbohoty
- 61. 27/7/1441 61 Maintenance treatment of DVT or PE? • Treatment with therapeutic doses of subcutaneous LMWH should be employed during the remainder of the pregnancy and for at least 6 weeks postnatally and until at least 3 months of treatment has been given in total. • Women should be taught to self-inject LMWH and arrangements made to allow safe disposal of needles and syringes. • Outpatient follow-up should include clinical assessment and advice with monitoring of blood platelets and peak anti-Xa levels if appropriate. • Pregnant women who develop heparin-induced thrombocytopenia or have heparin allergy and require continuing anticoagulant therapy should be managed with an alternative anticoagulant under specialist advice.3/21/20 elbohoty USE of intravenous HMWH • Massive PE • Women at high risk of haemorrhage and in whom continued heparin treatment until the risk factors for haemorrhage have resolved. • Acute DVT at term as it is more easily manipulated. 3/21/20 elbohoty
- 62. 27/7/1441 62 Manipulations of LMWH before the delivery • The woman on LMWH for maintenance therapy should be advised that once she is in established labour or thinks that she is in labour, she should not inject any further heparin. • Where delivery is planned, either by elective caesarean section or induction of labour, LMWH maintenance therapy should be discontinued 24 hours prior to planned delivery. • Regional anaesthetic or analgesic techniques should not be undertaken until at least 24 hours after the last dose of therapeutic LMWH. • LMWH should not be given for 4 hours after the use of spinal anaesthesia or after the epidural catheter has been removed, and the epidural catheter should not be removed within 12 hours of the most recent injection. 3/21/20 elbohoty • In patients receiving therapeutic doses of LMWH, wound drains (abdominal and rectus sheath) should be considered at caesarean section and the skin incision should be closed with interrupted sutures to allow drainage of any haematoma. 3/21/20 elbohoty
- 63. 27/7/1441 63 Postnatal anticoagulation • Therapeutic anticoagulant therapy should be continued for the duration of the pregnancy and for at least 6 weeks postnatally and until at least 3 months of treatment has been given in total. • Postpartum warfarin should be avoided until at least the fifth day and for longer in women at increased risk of postpartum haemorrhage. • Women should be offered a choice of LMWH or oral anticoagulant for postnatal therapy after discussion about the need for regular blood tests for monitoring of warfarin, particularly during the first 10 days of treatment. • No data on NOACs in breast feeding • Before discontinuing treatment the continuing risk of thrombosis should be assessed. 3/21/20 elbohoty Prevention of post-thrombotic syndrome • Women should be advised that prolonged use of LMWH (more than 12 weeks) is associated with a significantly lower chance of developing post-thrombotic syndrome. 3/21/20 elbohoty
- 64. 27/7/1441 64 3/21/20 elbohoty Lower doses of LMWH should be employed if the creatinine clearance is less than 30 ml/minute (enoxaparin and dalteparin) or less than 20 ml/minute with tinzaparin. 3/21/20 elbohoty
- 65. 27/7/1441 65 Upper limb DVT • Management of upper extremity DVT needs to be on an individual patient basis and should include management of any underlying condition. • Patients with upper extremity DVT without underlying risk factors (such as antiphospholipid antibodies) do not require prolonged (more than 3-6 months) anticoagulant treatment. 3/21/20 elbohoty superficial thrombophlebitis • Patients with clinical signs of superficial thrombophlebitis affecting the proximal long saphenous vein should have an ultrasound scan to exclude concurrent dvt. • Patients with superficial thrombophlebitis should have anti- embolism stockings and can be considered for treatment with prophylactic doses of lmWh for up to 30 days or fondaparinux for 45 days. • if LMWH is contraindicated, 8-12 days of oral nsaids should be offered. • Patientswithsuperficialthrombophlebitisat,orextendingtowa rds,thesapheno-femoral junction can be considered for therapeutic anticoagulation for 6-12 weeks.3/21/20 elbohoty
- 68. 27/7/1441 68 Antiphospholipid Antibodies • It was originally thought that aPL is directed against negatively charged phospholipid, but it is now clear that they target plasma proteins with affinity to these phospholipids. • The main antigens involved are • b2-glycoprotein (b2GPI) also known as apolipoprotein H • Prothrombin, • Many more antigenic target have been described 3/21/20 elbohoty A multisystemic disease, characterized by venous or arterial thromboses, or certain obstetric complications, & the presence of antiphospholipid antibodies (APAs) APAs are a heterogeneous group of autoantibodies that bind to negatively charged phospholipids, phospholipid-binding protein, or a combination of the two. Lupus anticoagulant (LA), anticardiolipin antibodies (aCL) & anti-beta 2 glycoprotein 1 (anti-β2GP1) antibodies are the main types. occurs in isolation as a primary APS in > 50% of the cases, or associated with other autoimmune diseases, most often with systemic lupus erythemathosus (SLE). occurs > in young women of fertile age (rarely in children, and only 12% of all APS occur after 50 years of age)
- 69. 27/7/1441 69 Pathophysiology & Aetiology Multiple mechanisms are responsible for the varying clinical manifestations. • b2GPI antibody disrupt normal coagulation mechanisms in several ways • Direct cellular effects caused by bound b2GPI-antibody complexes • Activation of platelets • Endothelial cells & monocytes activation • Leading to induction of tissue factor expression • Interference of haemostatic factors • Resistance to activated protein C • Reduction in fibrinolysis 3/21/20 elbohoty 3/21/20 elbohoty
- 70. 27/7/1441 70 3/21/20 elbohoty 3/21/20 elbohoty Multiple Strokes in a Young Woman (Brain MRI) Occlusion of Right Middle Cerebral Artery In a 3 Years Old Child with Severe Headache and Hemiparesis With aCL Antibodies +
- 71. 27/7/1441 71 3/21/20 elbohoty Digital Necrosis and Gangrene Livedo reticularis 3/21/20 elbohoty
- 72. 27/7/1441 72 Livedo reticularis with necrotic finger tips in Antiphospholipid syndrome 3/21/20 elbohoty Prevalence • The syndrome occurs most commonly in young to middle- aged adults. • Women are more frequently affected • Female to male ratio is 5:1 • There is NO racial predominance for primary APS, although a higher prevalence of SLE occur in the black & Hispanic populations. 3/21/20 elbohoty
- 73. 27/7/1441 73 1. Primary antiphospholipid syndrome APS occurs in the absence of any other related disease. 2. Secondary antiphospholipid syndrome APS occuring in the context of other autoimmune diseases, such as systemic lupus erythematosus (SLE). 3. Catastrophic antiphospholipid syndrome In rare cases, APS leads to rapid organ failure due to generalised thrombosis; this is termed (CAPS) and is associated with a high risk of death. APS morbidity • APS is the most common cause of acquired thrombophilia. Prevalence in general population: 2-1% • 15-20% of all DVT with or without PE. • 1/3 of new strokes in patients < 50 years age. • 10-15% women with recurrent pregnancy losses. • APS: significant proportion of thromboembolic disease and pregnancy loss in SLE. • APL Abs present in 30-40% SLE. One third of those patients have clinical manifestations of APS. • aCL positivity may precede a more severe form of SLE. 3/21/20 elbohoty
- 74. 27/7/1441 74 Epidemiology of antiphospholipid antibodies • in the normal population: 2 - 12 % prevalence increases with age and chronic disease • in SLE: 30 - 40 % LAC: 11-30% aCL: 24-86% • 15-20% of all DVT with or without PE. • 1/3 of new strokes in patients < 50 years age. • 10-15% women with recurrent pregnancy losses. 3/21/20 elbohoty Clinical Features • Diagnosis of APS is made by finding at least 1 of the clinical criteria plus at least 1 of the laboratory criteria. • Provided the combination of the clinical criteria & the laboratory criteria is not < 12 weeks or > 5 years. • Clinical criteria: • Vascular thrombosis • Pregnancy morbidity • Laboratory criteria: • Lupus anticoagulant • Anti-cardiolipin antibody (IgG &/or IgM) • Anti-b2-glycoprotein I antibody (IgG &/or IgM) 3/21/20 elbohoty
- 75. 27/7/1441 75 In Pregnancy IUGRRecurrent miscarriage Preeclampsia Placental abruption In addition: Arterial / Venous thrombosis Premature delivery or fetal death Obstetric Complications • Pregnancy loss • About 15 % of women with recurrent pregnancy loss, defined as ≥ 3 first trimester miscarriages, have detectable aPL. • These women have a potential 90% risk of further fetal loss if left untreated. • The diagnostic criteria for APS suggest that evaluation should begin after the 3rd consecutive early miscarriage, defined by less than 10 weeks of gestation. • However, in practice, evaluation after 2 miscarriages is often initiated. 3/21/20 elbohoty
- 76. 27/7/1441 76 Obstetric Complications • Late complications of aPL in pregnancy • These relate to placental insufficiency caused by aPL. • Gestational hypertension/preeclampsia occurs in 30–50% of untreated women with known APS. • This falls to 10% with effective treatment. • By contrast, there is no increase in aPL incidence in general obstetric patients representing with preeclampsia. • HELLP syndrome may occur usually associated with preeclampsia/eclampsia; • This seems to occur earlier than in women without APS, often in the 2nd trimester. 3/21/20 elbohoty Obstetric Complications • Other clinical manifestations • In addition to thrombosis & obstetric morbidity, there are additional clinical manifestations that are no included in the official definition of APS. 3/21/20 elbohoty
- 77. 27/7/1441 77 Diagnosis: 1 Clinical + 1 Laboratory • Diagnostic criteria for the classification of definite APS are agreed by an international panel in 1999, & updated in 2006. 3/21/20 elbohoty 3/21/20 elbohoty Test Details Anticardiolipin Antibodies Anti-beta2Glycoprotein I Antibodies Lupus Anticoagulant Antibodies detected IgG and IgM antibodies against cardiolipin and cardiolipin-bound beta2 glycoprotein I IgG and IgM antibodies against cardiolipin-bound beta2 glycoprotein I Immunoglobulins that cause prolonged clotting times in vitro but are associated with thrombosis in vivo Titres considered positive Medium to high: > 99th percentile, or > 40 IgG or IgM phospholipid units* Medium to high: > 99th percentile, or IgG or IgM phospholipid units* Not applicable Influenced by anticoagulation therapy? No No False positive test if on heparin and may prolong prothrombin time if on warfarin Abbreviations: IgG, immunoglobulin G; IgM, immunoglobulin M.
- 78. 27/7/1441 78 Management of APS in Pregnancy • General issues • A detailed past medical & obstetric history should be taken & the circumstances of any past thrombotic event (provoked or spontaneous, arterial or venous) assessed. • Any associated conditions should be assessed, such as SLE. • Evidence of any organ damage sought. • Other risk factor contributing to thrombotic risk, such as obesity & maternal age should be taken into account in the overall assessment, as it will contribute in making an appropriate individualised treatment plan. 3/21/20 elbohoty Pre-Pregnancy Planning • There may circumstances where pregnancy should be discouraged; for example • If pulmonary hypertension is present the risk of maternal death is > 35% • A clear plan for pregnancy management should be developed. 3/21/20 elbohoty
- 79. 27/7/1441 79 Management of APS in Pregnancy • General issues • It may be that the conflicting results are due to heterogeneity of the cause of disorder, & that further stratification is necessary in treatment according to clinical phenotype, as suggested by Bramham et al. • A summary of management of women with APS or aPL is given in the following table: 3/21/20 elbohoty How should women with antiphospholipid antibodies be treated? • Persistent antiphospholipid antibodies (lupus anticoagulant and/or anticardiolipin and/or β2-glycoprotein 1 antibodies) in women without previous VTE should be considered as a risk factor for thrombosis such that if she has other risk factors she may be considered for antenatal or postnatal thromboprophylaxis as above. 3/21/20 elbohoty
- 80. 27/7/1441 80 Fetal monitoring • Fetal growth scan + Umblical artery doppler from 26 and follow up every 4 weeks 3/21/20 elbohoty Management of women with aPL & multiple previous venous events, or venous plus arterial events • This group of women will be on long-term warfarin, possible at higher range international normalised ratio (INR). • They are at very high risk in pregnancy. • Pre-pregnancy counselling is particularly important, so that the extent of risk can be clarified on an individual basis, pre- pregnancy health optimised, & the risk with clear plan convoyed to the woman & documented. 3/21/20 elbohoty
- 81. 27/7/1441 81 Management of women with APS as part of SLE • Women with SLE may have flare-up of symptoms during pregnancy & requires steroids. • Hydroxychloroquine & azathioprine are regularly used in SLE. • They are safe in pregnancy & so should be continued as necessary. 3/21/20 elbohoty Management of women with APS & thrombocytopenia • Many patients with APS have thrombocytopenia (platelets < 100 x 109/l). • The pathogenic antibodies are directed toward platelet membrane glycoprotein & are distinct from aPL. • Patients should be managed in the same way for immune thrombocytopenia. • When there have been previous thromboses, the fine balance between bleeding & thrombotic risk must be carefully managed. • A platelet count of > 50 x 109/l should be to allow safe pharmacological thromboprophylaxis. 3/21/20 elbohoty
- 82. 27/7/1441 82 CATASTROPHIC ANTIPHOSPHOLIPID SYNDROME (CAPS) Catastrophic APS • This term defines a severe, accelerated form of APS resulting in multi-organ failure from widespread thromboses, which are usually microvascular rather than large-vessel occlusions. • The syndrome is of acute onset, defined by the involvement of at least 3 different organ systems over a period of days to weeks. • Triggers such as infection or surgery exacerbate an already pro-coagulable state. 3/21/20 elbohoty
- 83. 27/7/1441 83 Catastrophic antiphospholipid syndrome • It is a life- threatening disease conferring 50% mortality. • It complicates less than 1% of antiphospholipid syndrome cases • It is characterised by • the onset of rapidly progressive and • widespread thrombotic microangiopathy and • by multi- organ failure. • The severity of the maternal impact of this condition justifies aggressive therapy, included • Anticoagulation • high-dose steroids and • plasma exchange.
- 84. 27/7/1441 84 Management: • Current treatment guidelines suggest, in addition to early diagnosis, aggressive therapies to avoid the potentially fatal outcome. • The combination of: - high doses of intravenous (i.v.) heparin, - i.v. steroids, - i.v. immunoglobulins and/or - Repeated plasma exchanges are the basic treatment of choice for all patients with this severe condition
- 85. 27/7/1441 85 A case of catastrophic antiphospholipid syndrome • A 25-year-old para 0 books in for antenatal care at 15 weeks of gestation. Her first pregnancy four years previously was complicated by a fetal death in utero at 18 weeks of gestation as a consequence of catastrophic antiphospholipid syndrome with strongly positive ß2- glycoprotein and anticardiolipin antibodies. • She developed significant microangiopathic haemolysis which responded to plasma exchange and steroid treatment. • Placental histology revealed accelerated villous maturation, infarction and maternal vasculopathy. She attended pre- pregnancy counselling with a plan for antenatal thromboprophylaxis with aspirin 150 mg nocte and LMWH (enoxaparin 60 mg subcutaneously daily). • Apart from mild thrombocytopenia she had an uneventful antenatal course, receiving high-risk care in a multidisciplinary setting. • Following induction of labour at 38 weeks of gestation, she delivered a healthy baby boy weighing 3480 g. She received postpartum thromboprophylaxis for 6 weeks. The role of thrombophilia testing in women with adverse pregnancy outcomes
- 86. 27/7/1441 86 • Thrombophilias are a diverse group of coagulation disorders associated with a predisposition to thrombotic events and placenta-mediated pregnancy complications. • Evidence-based evaluation and treatment of patients with adverse pregnancy outcomes is often impeded by two factors: • understandably emotionally charged parents who would ‘do anything’ to have a successful pregnancy outcome, and are thus accepting of unproven and unnecessary invasive treatments, and • clinicians’ uncertainty and the willingness to ‘try anything’ in this context. • At present, within a heterogeneous set of underlying causes, inherited thrombophilias appear to be, at best, a weak contributor to adverse pregnancy outcomes. • As always, association does not prove causation, and even if causation is established, effective therapies need to be available before routine testing can be justified. • This is not the case for heritable thrombophilias, and as a result, testing for them in women who have sustained adverse pregnancy outcomes cannot currently be recommended.
- 87. 27/7/1441 87 • Their increased prevalence in this population does not justify testing with a view to improving long-term maternal health outcomes either, as this approach has not been shown to confer a net benefit, and has potential harms associated with insurance risk profiles and familial consequences of this genetic information. • In recent years, numerous studies, trials and meta-analyses have been published. • Most recently, the well-conducted TIPPS trial clearly demonstrated negative evidence for heparin treatment in improving pregnancy outcomes among women with thrombophilias. thrombophilia testing • should only be performed when results will be used to improve or modify management. • testing is performed far more frequently than can be justified based on available evidence and that the majority of testing is not of benefit to the patient, but may actually be harmful • In its 2016 Choosing Wisely initiative, the Society for Maternal and Fetal Medicine in the USA has urged clinicians to refrain from thrombophilia evaluation for women with histories of pregnancy loss, fetal growth restriction, severe pre-eclampsia and abruption.
- 88. 27/7/1441 88 To test? • The problem with testing for underlying thrombophilias and modified management in a subsequent pregnancy can be illustrated with an example: • evidence provided in a systematic review and meta- analysis reported an 81% increased risk of recurrent pregnancy loss in women with prothrombin gene mutation; while this significant relationship is acknowledged, there is currently no evidence that acting on these test results alters pregnancy course and outcome. • The same argument applies to factor V Leiden mutation (FVL) status and the small increased risk of late pregnancy loss In APS • It is imperative to note that antiphospholipid antibodies may be present in healthy patients without disease. • Although women with antiphospholipid antibodies had higher rates of low birthweight and placental infarctions, there was no difference in rates of fetal loss or maternal disease overall when compared with the control group. • It seems plausible that the primary cause of adverse pregnancy outcome in antiphospholipid syndrome relates to inflammation, rather than thrombosis.
- 89. 27/7/1441 89 APs • Based on somewhat limited data aspirin and LMWH are recommended for obstetrical antiphospholipid syndrome, although there is no clear evidence that additional treatment with LMWH improves live-birth rates. • The first-line treatment for women with obstetrical antiphospholipid syndrome should be low-dose aspirin. • Although the use of LMWH in women with obstetrical antiphospholipid syndrome has been widely adopted, significant methodological heterogeneity between studies exists with regard to study population, intervention dose and timing, inclusion criteria and composite outcomes, leading to lack of conclusive evidence to support or withhold treatment. Subsequent pregnancy care • Prenatal care in women with previous adverse pregnancy outcomes should be provided in an empathetic, high-quality clinical care setting including emotional and mental health support, increased ultrasound surveillance, frequent visits and timely delivery. • Treatment with LMWH in women with inheritable thrombophilias is currently not recommended. • Efforts should be made to optimise treatment with aspirin, taking into account recent evidence to suggest that treatment with higher doses of aspirin (100–150 mg) administered ideally at nighttime and commenced before 16 weeks of gestation improves subsequent pregnancy outcome. • Although these data are derived from studies evaluating the recurrence reduction in the setting of pre-eclampsia and fetal growth restriction, dosing regimens may be adopted for the purpose of risk reduction in other placenta-mediated pregnancy complications as outlined above.
- 90. 27/7/1441 90 Additional thromboprophylaxis with LMWH may be indicated in • women with positive antiphospholipid syndrome antibodies • a history of catastrophic antiphospholipid syndrome or venous thromboembolism; • ideally these women should be cared for in a multidisciplinary care setting with haematology input Questions 3/21/20 elbohoty acquired 20%
- 91. 27/7/1441 91 Questions 3/21/20 elbohoty 30 – 50% at least one Questions 3/21/20 elbohoty
- 93. 27/7/1441 93 Questions 3/21/20 elbohoty 10 – 20 % Previous obstetric outcome Thromboprophylaxis in surgical patients • All surgical interventions carry a risk of VTE and attention should be paid to modifiable risk factors. • a 2-fold increased risk in women using a combined pill. • So stoppage of CHC prior to planned surgery reduces the risk of VTE. 3/21/20 elbohoty
- 94. 27/7/1441 94 RISK OF VTE for abdominal surgery in patients who did not receive specific thromboprophylaxis • asymptomatic DVT at post operative screening 25% • asymptomatic proximal DVT at post operative screening 7% • symptomatic DVT 6% • symptomatic non-fatal PE 1-2% • fatal PE 0.5% 3/21/20 elbohoty VTE prophylaxis for surgery • Patients undergoing abdominal surgery who are at risk due to the procedure or personal risk factors should receive thromboprophylaxis with mechanical methods and either subcutaneous LMWH, UFH or fondaparinux. • In patients undergoing gynaecological surgery, when assessment of risk favours pharmacological thromboprophylaxis, UFH or LMWH may be used. • Mechanical methods can be considered in addition to pharmacological methods. • Anti-embolism stockings AES or intermittent pneumatic compression devices are recommended for prophylaxis in surgical patients. • In patients undergoing abdominal surgery Anti Embolic Stocking (AES) can be used alone when pharmacological agents are contraindicated, for example due to high bleeding risk. • Aspirin is not recommended as the sole pharmacological agent for VTE prophylaxis in surgical patients, as other available agents are more effective. • Pharmacological thromboprophylaxis is typically continued until discharge. Extended prophylaxis should be considered on a case-by-case basis, for example when multiple thrombosis risk factors are present. • The use of AES should continue until there is a return to the pre-morbid level of mobility. 3/21/20 elbohoty
