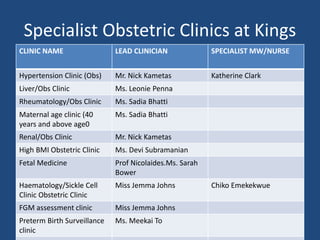
This document discusses venous thromboembolism (VTE) in pregnancy. It notes that VTE is more common in pregnant women than non-pregnant women, with an incidence of 85/100,000 pregnancies. Risk factors include blood group A, multiple pregnancy, cesarean delivery, and increased age or BMI. Diagnosis involves ultrasound or CT scans, with D-dimer testing not recommended. Treatment involves low molecular weight heparin until diagnosis is ruled out. Specialist obstetric clinics are available at King's Hospital for conditions like preeclampsia, liver disease, rheumatology and more.