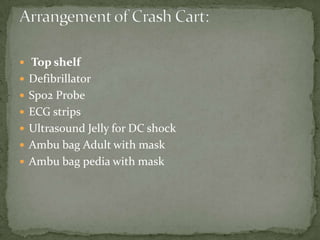
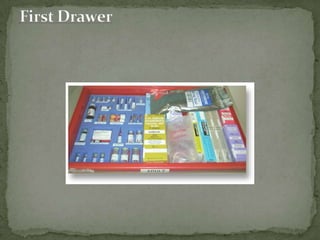
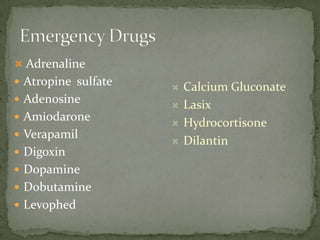
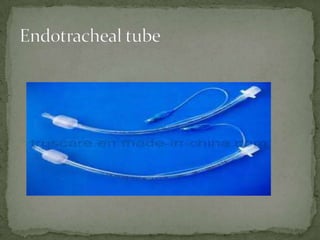
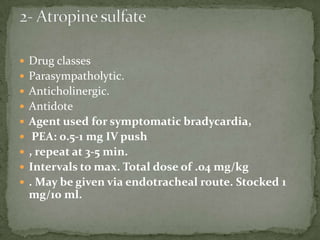
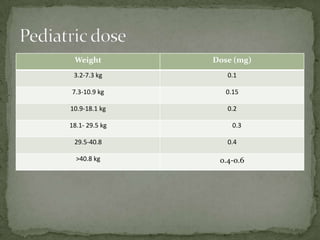
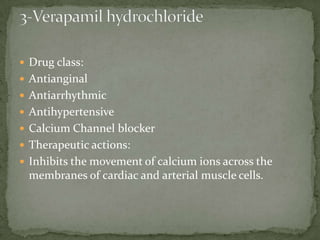
This document provides information about crash cart contents and procedures at CBAHI. It defines a crash cart as a means of storing and transporting emergency equipment and drugs. The first crash cart was created in 1962. Crash carts must be checked regularly by nurses and biomed to ensure proper function and expiration dates. Contents are arranged in a standardized way and include airway management, resuscitation medications, and equipment for defibrillation and monitoring. Nurses must check crash carts at the beginning of each shift to ensure readiness for emergencies.