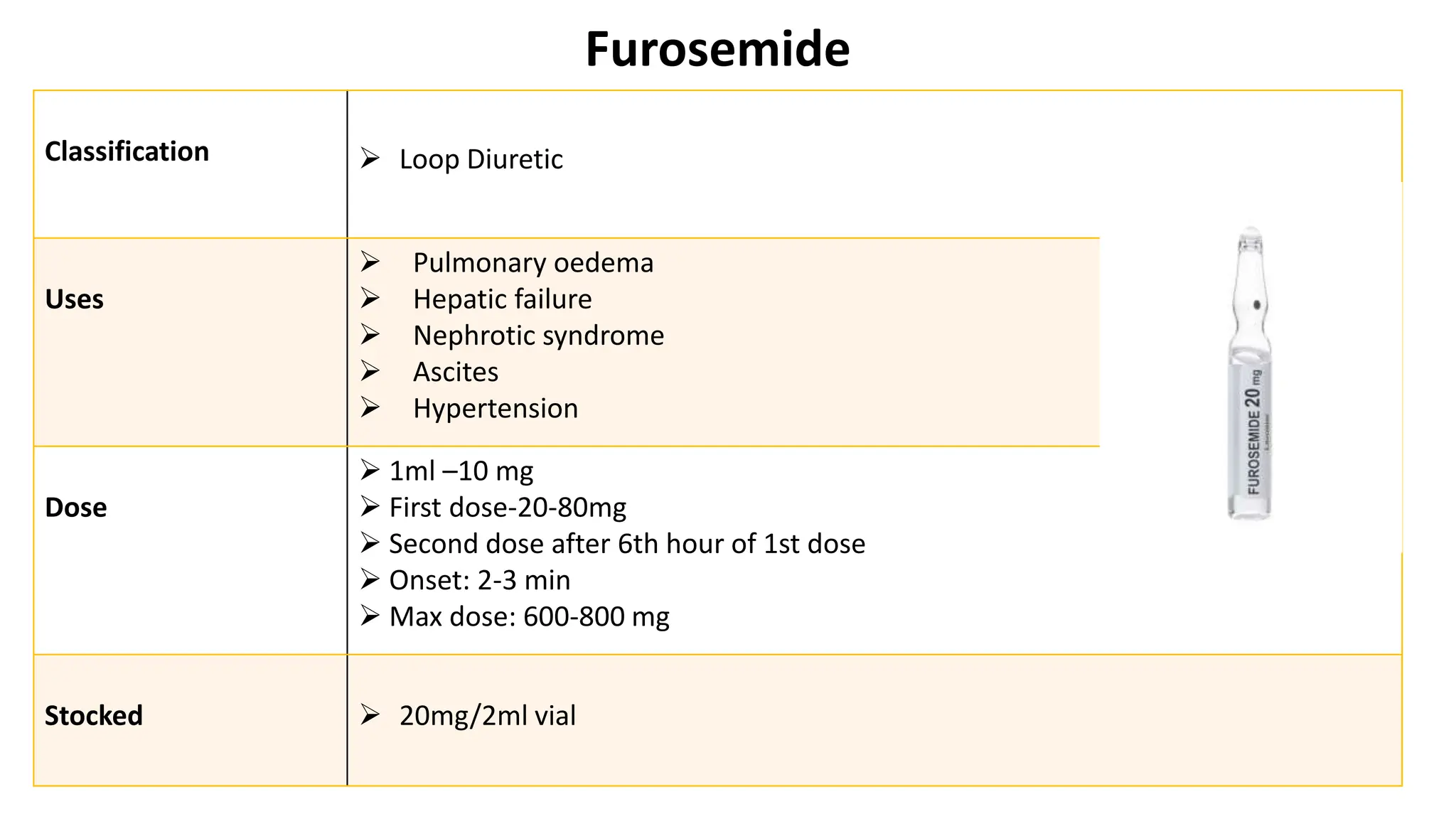
The document outlines the learning objectives and protocols for managing critical care situations, particularly during code blue emergencies. It details the phases of response, required medications, their classifications, uses, dosages, and nursing responsibilities for administering these drugs. Key medications discussed include epinephrine, atropine, amiodarone, and others used in emergency settings, along with their specific nursing protocols to ensure effective patient care.