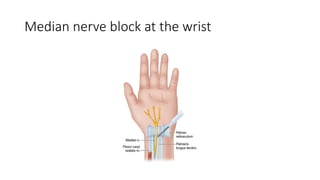
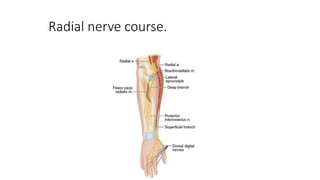
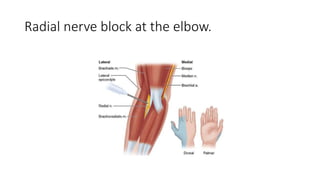
The document describes nerve blocks for the median, ulnar, radial, and musculocutaneous nerves. It provides details on locating each nerve, inserting the needle, and injecting local anesthetic. It also describes digital nerve blocks, an intercostobrachial nerve block, and intravenous regional anesthesia (Bier block).