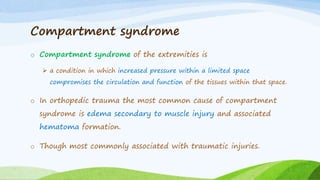
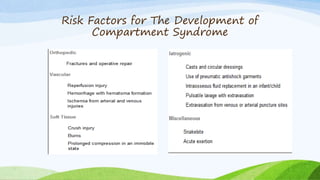
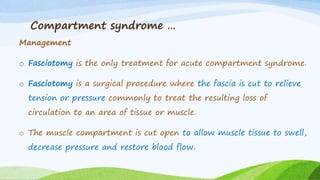
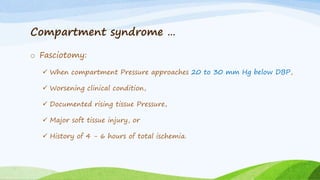
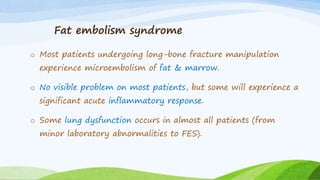
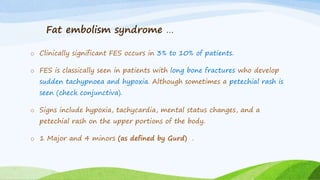
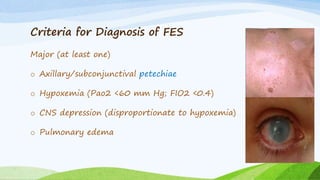
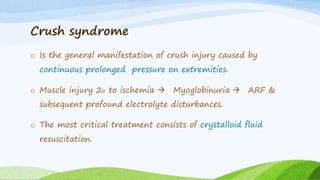
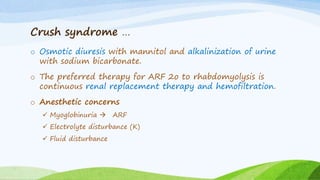
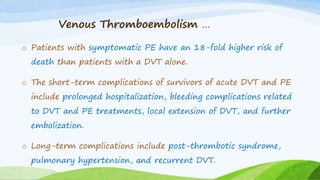
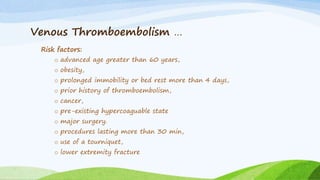
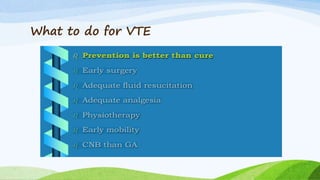
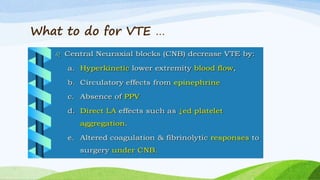
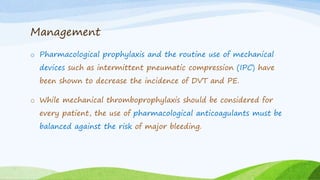
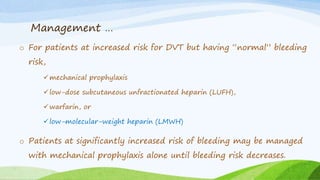
This document discusses several orthopedic trauma considerations for anesthesia. It compares general anesthesia (GA) versus regional anesthesia (RA) for orthopedic trauma, noting advantages and disadvantages of each. It also discusses risks like fat embolism syndrome, compartment syndrome, crush syndrome, and venous thromboembolism (VTE). For each condition, it describes causes, risk factors, signs/symptoms, diagnostic criteria, and treatment approaches. Throughout, it emphasizes the importance of early stabilization of fractures to prevent complications.