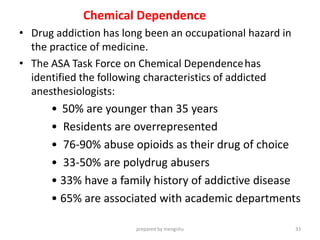
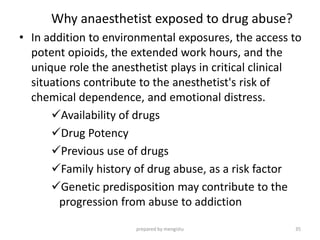
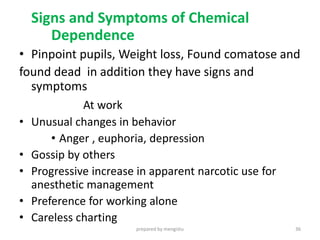
This document discusses occupational hazards faced by anesthetists. It begins by outlining course objectives to understand hazards and minimize risks. It then explores various types of hazards including chemical (anesthetic gases), radiation, infectious diseases, and physical risks. Specific health risks from exposure like fatigue and effects on performance are examined. The document provides details on minimizing different hazards through techniques like gas scavenging and personal protective equipment.