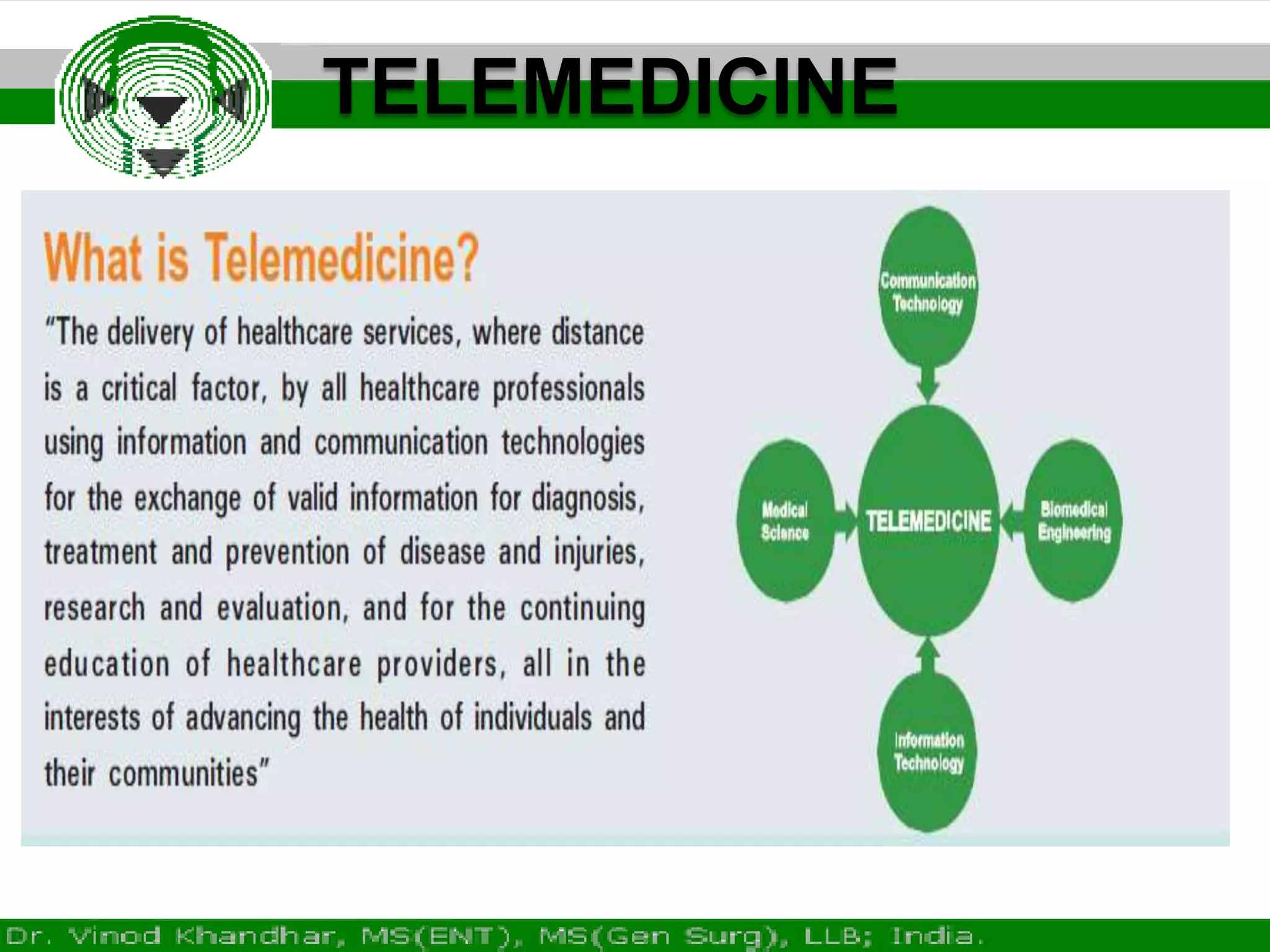
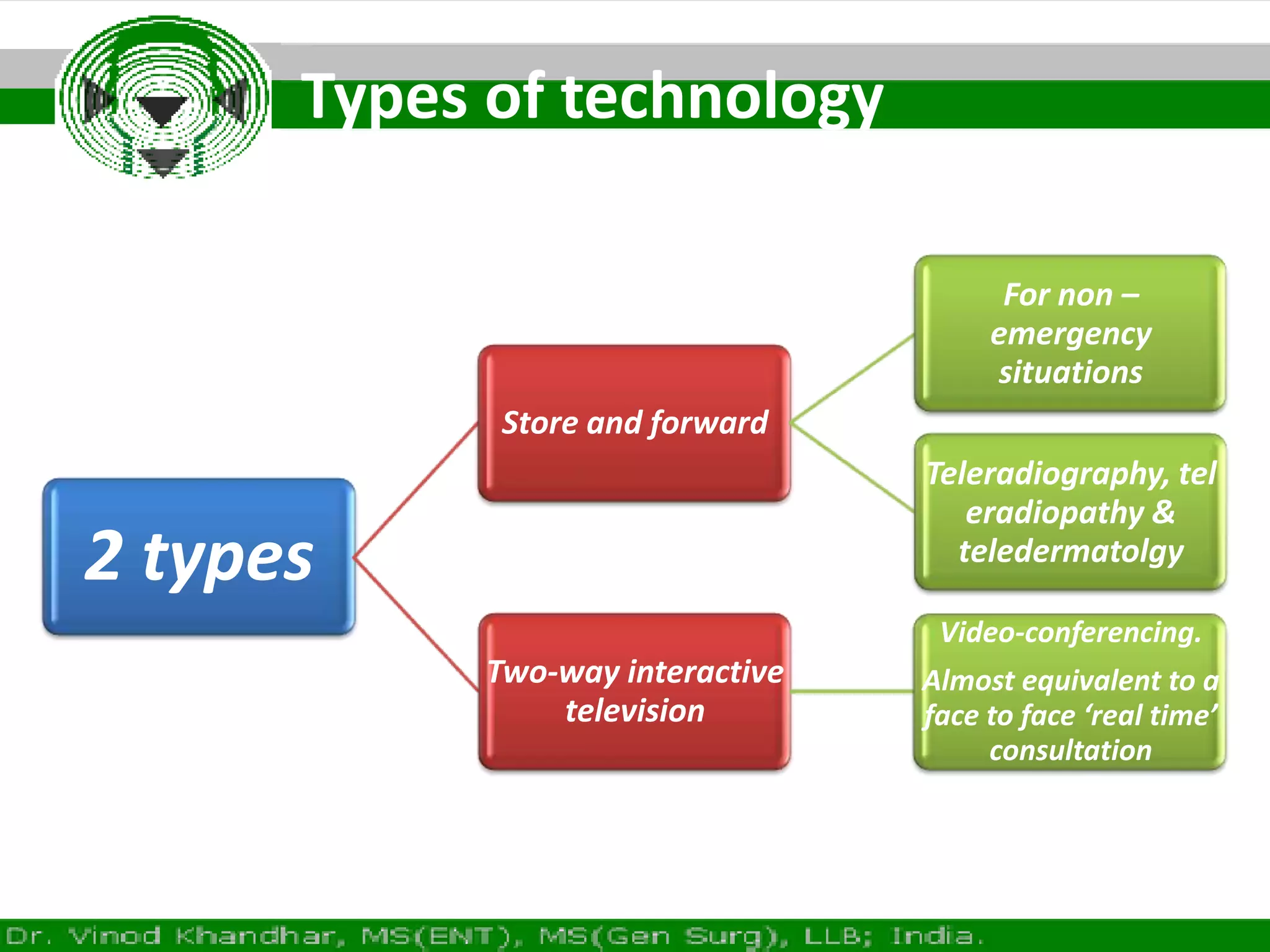
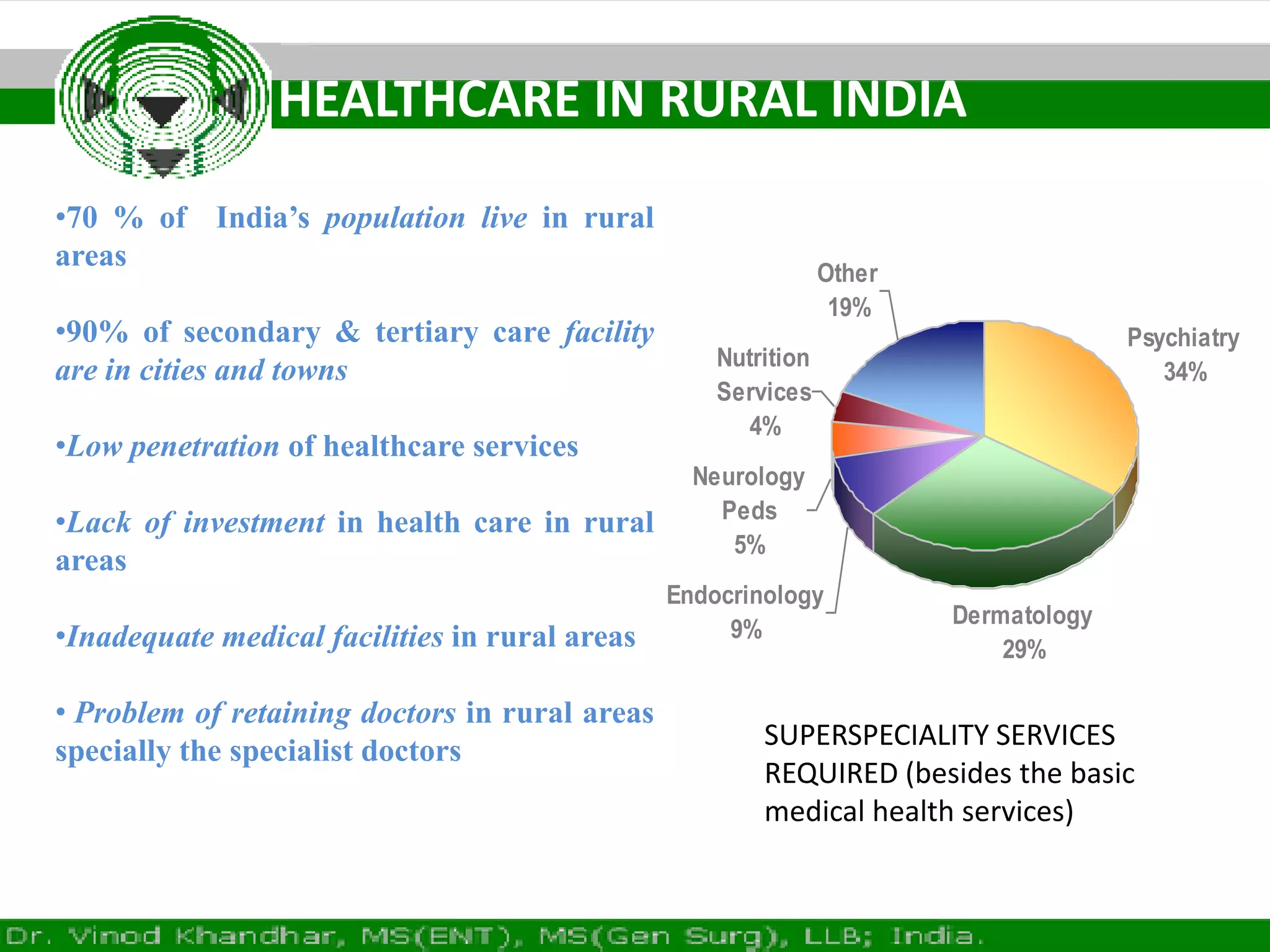
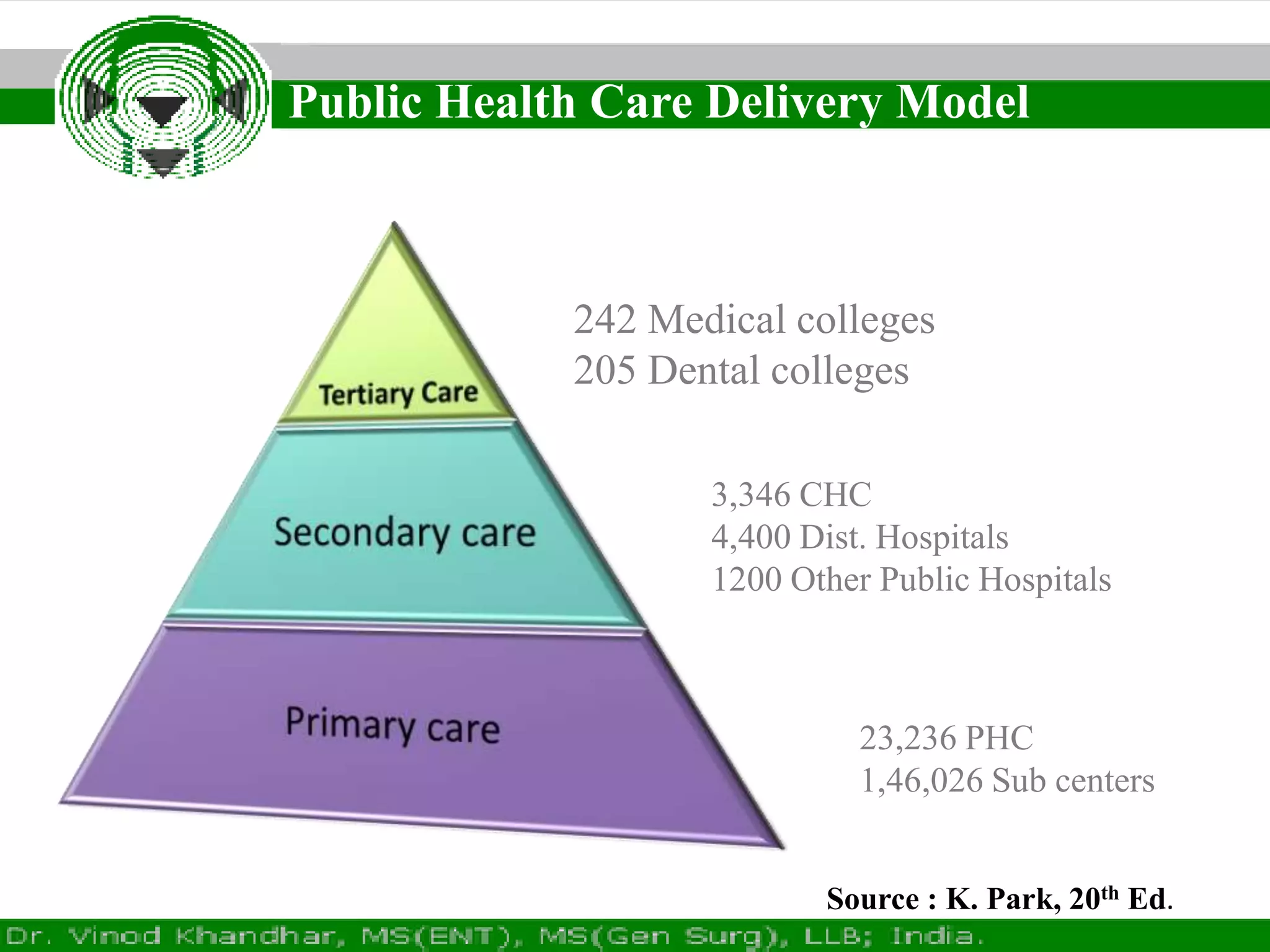
This document discusses telemedicine projects and initiatives in India. It outlines the benefits of telemedicine including improved access to specialized healthcare for rural populations, cost savings from reduced travel, and continued education for healthcare professionals. It describes the types of telemedicine technologies used in India and provides an overview of the current telemedicine landscape and infrastructure in the country. Key goals of national telemedicine networks are highlighted along with ongoing challenges and the need for standardized software, trained personnel, and stable electricity and bandwidth.