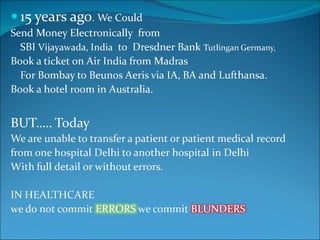
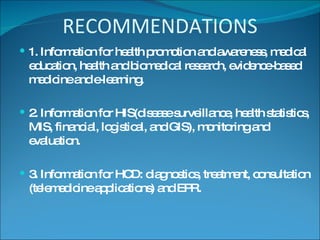
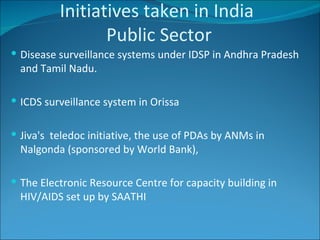
Last year, doctors in India used new ICT tools like pen scanners, email, GPRS, MMS, SMS, and Bluetooth in medical education, which led to question papers being leaked for entrance exams. The document discusses the relationship between health and information and communication technology (ICT) in India, including current uses of eHealth and telemedicine as well as challenges. It provides examples of both public and private sector initiatives using ICT and telemedicine in India. The future of eHealth in India is seen to include improved access to care through telemedicine and more advanced use of health records and mobile technologies.