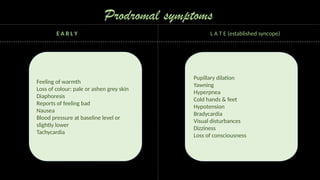
This presentation provides an overview of syncope, a common medical emergency in dental practice. Created during my internship, this presentation aims to educate dental students on the causes, symptoms, diagnosis and management of syncope with a focus on dental specific considerations.